J Korean Med Sci.
2020 Apr;35(14):e97. 10.3346/jkms.2020.35.e97.
Trends of Premature and Early Menopause: a Comparative Study of the US National Health and Nutrition Examination Survey and the Korea National Health and Nutrition Examination Survey
- Affiliations
-
- 1CHA Fertility Center, Seoul Station, Seoul, Korea.
- 2Department of Epidemiology, Graduate School of Public Health, Brown University, Providence, RI, USA.
- 3Graduate School of Public Health, Institute of Health and Environment, Seoul National University, Seoul, Korea.
- KMID: 2509612
- DOI: http://doi.org/10.3346/jkms.2020.35.e97
Abstract
- Background
While evidence shows a tendency toward delays in menopause worldwide, whether prevalence of premature (< 40 years) or early menopause (40–44 years) is also reduced in different ethnic groups is uncertain. The aim of this study was to explore birth cohort effect in the prevalence of premature and early menopause in United States (US) and Korea.
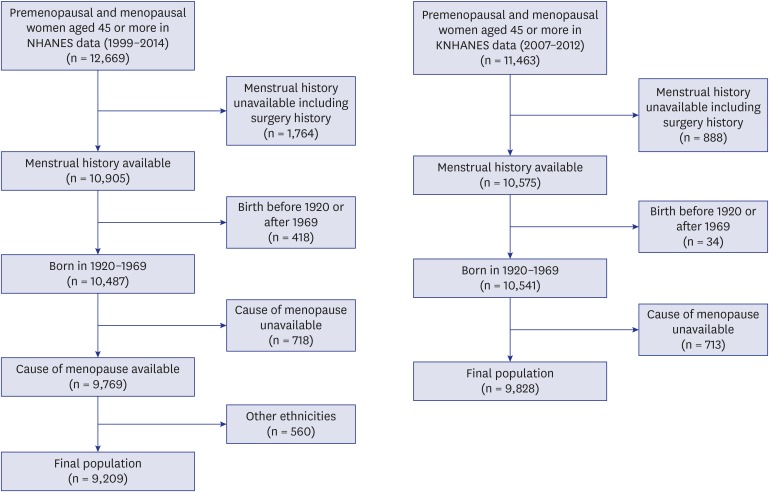
Methods
This is a retrospective study using the National Health and Nutrition Examination Survey (NHANES, 1999–2014) and the Korea NHANES (KNHANES, 2007–2012). We analyzed prevalence of premature and early menopause in three ethnic groups of US and Korea. We restricted our analysis to women aged ≥ 45 years at the time of the survey born between 1920 and 1969. The data of both eligible 9,209 US women and 9,828 Korean was included in final analysis. We calculated odds ratios (OR) for each outcome adjusting for biological and socioeconomic factors, respectively.
Results
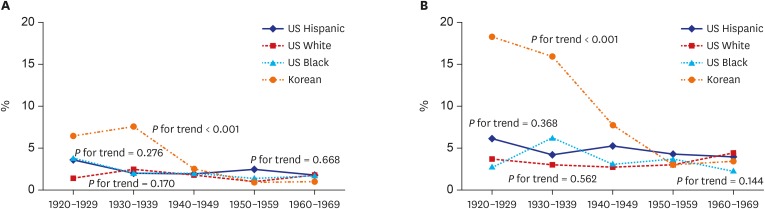
Prevalence of premature menopause was 1.7% in US, 2.8% in Korean women. Early menopause occurred in 3.4% and 7.2% of US and Korean, respectively. In US women, prevalence of premature and early menopause did not change and did not differ across three ethnicities. Korean women showed highest and consistently decreasing prevalence (P < 0.001). When we adjusted for covariates, birth lower risk for premature menopause was evident in US Non-Hispanic black born in 1950s and in Korean born between 1940s and 1960s compared to those born in 1920s. In the analysis of early menopause, excluding premature menopause patients, lower risk of more recent generation (born in 1940s and later) was evident in Korean women.
Conclusion
The trend and birth cohort effect in occurrence of premature and early menopause among the US and Korea women are different. Prevalences of premature and early menopause decrease only in Korean.
Keyword
Figure
Reference
-
1. McKinlay SM. The normal menopause transition: an overview. Maturitas. 1996; 23(2):137–145. PMID: 8735352.
Article2. Reynolds RF, Obermeyer CM. Age at natural menopause in Spain and the United States: results from the DAMES project. Am J Hum Biol. 2005; 17(3):331–340. PMID: 15849704.
Article3. Luborsky JL, Meyer P, Sowers MF, Gold EB, Santoro N. Premature menopause in a multi-ethnic population study of the menopause transition. Hum Reprod. 2003; 18(1):199–206. PMID: 12525467.
Article4. Haller-Kikkatalo K, Uibo R, Kurg A, Salumets A. The prevalence and phenotypic characteristics of spontaneous premature ovarian failure: a general population registry-based study. Hum Reprod. 2015; 30(5):1229–1238. PMID: 25712230.
Article5. Mishra GD, Pandeya N, Dobson AJ, Chung HF, Anderson D, Kuh D, et al. Early menarche, nulliparity and the risk for premature and early natural menopause. Hum Reprod. 2017; 32(3):679–686. PMID: 28119483.
Article6. Wu X, Cai H, Kallianpur A, Li H, Yang G, Gao J, et al. Impact of premature ovarian failure on mortality and morbidity among Chinese women. PLoS One. 2014; 9(3):e89597. PMID: 24603759.
Article7. Podfigurna-Stopa A, Czyzyk A, Grymowicz M, Smolarczyk R, Katulski K, Czajkowski K, et al. Premature ovarian insufficiency: the context of long-term effects. J Endocrinol Invest. 2016; 39(9):983–990. PMID: 27091671.
Article8. Muka T, Oliver-Williams C, Kunutsor S, Laven JS, Fauser BC, Chowdhury R, et al. Association of age at onset of menopause and time since onset of menopause with cardiovascular outcomes, intermediate vascular traits, and all-cause mortality: a systematic review and meta-analysis. JAMA Cardiol. 2016; 1(7):767–776. PMID: 27627190.9. Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019; 34(Suppl 1):e75. PMID: 30923488.
Article10. Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015; 18(4):483–491. PMID: 25845383.
Article11. Girard R, Météreau E, Thomas J, Pugeat M, Qu C, Dreher JC. Hormone therapy at early post-menopause increases cognitive control-related prefrontal activity. Sci Rep. 2017; 7(1):44917. PMID: 28322310.
Article12. Tibiletti MG, Testa G, Vegetti W, Alagna F, Taborelli M, Dalprà L, et al. The idiopathic forms of premature menopause and early menopause show the same genetic pattern. Hum Reprod. 1999; 14(11):2731–2734. PMID: 10548611.
Article13. Hoyos LR, Thakur M. Fragile X premutation in women: recognizing the health challenges beyond primary ovarian insufficiency. J Assist Reprod Genet. 2017; 34(3):315–323. PMID: 27995424.
Article14. Beck-Peccoz P, Persani L. Premature ovarian failure. Orphanet J Rare Dis. 2006; 1(1):9. PMID: 16722528.
Article15. Persani L, Rossetti R, Cacciatore C. Genes involved in human premature ovarian failure. J Mol Endocrinol. 2010; 45(5):257–279. PMID: 20668067.
Article16. Hewlett M, Mahalingaiah S. Update on primary ovarian insufficiency. Curr Opin Endocrinol Diabetes Obes. 2015; 22(6):483–489. PMID: 26512773.
Article17. Zsakai A, Mascie-Taylor N, Bodzsar EB. Relationship between some indicators of reproductive history, body fatness and the menopausal transition in Hungarian women. J Physiol Anthropol. 2015; 34(1):35. PMID: 26494263.
Article18. Hardy R, Kuh D. Reproductive characteristics and the age at inception of the perimenopause in a British National Cohort. Am J Epidemiol. 1999; 149(7):612–620. PMID: 10192308.
Article19. Gold EB. The timing of the age at which natural menopause occurs. Obstet Gynecol Clin North Am. 2011; 38(3):425–440. PMID: 21961711.
Article20. Forman MR, Mangini LD, Thelus-Jean R, Hayward MD. Life-course origins of the ages at menarche and menopause. Adolesc Health Med Ther. 2013; 4:1–21. PMID: 24600293.
Article21. Chang SH, Kim CS, Lee KS, Kim H, Yim SV, Lim YJ, et al. Premenopausal factors influencing premature ovarian failure and early menopause. Maturitas. 2007; 58(1):19–30. PMID: 17531410.
Article22. Yasui T, Hayashi K, Mizunuma H, Kubota T, Aso T, Matsumura Y, et al. Factors associated with premature ovarian failure, early menopause and earlier onset of menopause in Japanese women. Maturitas. 2012; 72(3):249–255. PMID: 22572589.
Article23. Hardy R, Kuh D. Social and environmental conditions across the life course and age at menopause in a British birth cohort study. BJOG. 2005; 112(3):346–354. PMID: 15713152.
Article24. Luoto R, Kaprio J, Uutela A. Age at natural menopause and sociodemographic status in Finland. Am J Epidemiol. 1994; 139(1):64–76. PMID: 8296776.
Article25. Lawlor DA, Ebrahim S, Smith GD. The association of socio-economic position across the life course and age at menopause: the British Women's Heart and Health Study. BJOG. 2003; 110(12):1078–1087. PMID: 14664879.
Article26. Kriplani A, Banerjee K. An overview of age of onset of menopause in northern India. Maturitas. 2005; 52(3-4):199–204. PMID: 16257611.
Article27. Kaczmarek M. The timing of natural menopause in Poland and associated factors. Maturitas. 2007; 57(2):139–153. PMID: 17307314.
Article28. Nichols HB, Trentham-Dietz A, Hampton JM, Titus-Ernstoff L, Egan KM, Willett WC, et al. From menarche to menopause: trends among US Women born from 1912 to 1969. Am J Epidemiol. 2006; 164(10):1003–1011. PMID: 16928728.
Article29. Pakarinen M, Raitanen J, Kaaja R, Luoto R. Secular trend in the menopausal age in Finland 1997–2007 and correlation with socioeconomic, reproductive and lifestyle factors. Maturitas. 2010; 66(4):417–422. PMID: 20537824.
Article30. Wang D, Wang M, Cheng N, Zheng T, Hu X, Li H, et al. Sulfur dioxide exposure and other factors affecting age at natural menopause in the Jinchuan cohort. Climacteric. 2015; 18(5):722–732. PMID: 25853925.
Article31. Mirel LB, Mohadjer LK, Dohrmann SM, Clark J, Burt VL, Johnson CL, et al. National health and nutrition examination survey: estimation procedures, 2007–2010. Vital Health Stat 2. 2013; (159):1–17.32. Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, et al. National health and nutrition examination survey: sample design, 2007–2010. Vital Health Stat 2. 2013; (160):1–23.33. Park HA. The Korea national health and nutrition examination survey as a primary data source. Korean J Fam Med. 2013; 34(2):79. PMID: 23560205.
Article34. Wise LA, Krieger N, Zierler S, Harlow BL. Lifetime socioeconomic position in relation to onset of perimenopause. J Epidemiol Community Health. 2002; 56(11):851–860. PMID: 12388578.
Article35. Tawfik H, Kline J, Jacobson J, Tehranifar P, Protacio A, Flom JD, et al. Life course exposure to smoke and early menopause and menopausal transition. Menopause. 2015; 22(10):1076–1083. PMID: 25803667.
Article36. Park YJ, Kim HS, Kang HC. The age at menopause and related factors in Korean women. J Korean Acad Nurs. 2002; 32(7):1024–1031.
Article37. Shin YJ, Song JY, Kim MJ, Choi JI, Han KD, Lee HN. Relationship between age at last delivery and age at menopause: the Korea national health and nutrition examination survey. Obstet Gynecol Sci. 2017; 60(4):362–368. PMID: 28791268.
Article38. Committee Opinion No. 605: primary ovarian insufficiency in adolescents and young women. Obstet Gynecol. 2014; 123:193–197.39. Agaba P, Meloni S, Sule H, Ocheke A, Agaba E, Idoko J, et al. Factors associated with early menopause among women in Nigeria. J Virus Erad. 2017; 3(3):145–151. PMID: 28758022.
Article40. Deering VA. Prevalence of premature ovarian failure and premature menopause in refugee and immigrant women in the U.S. compared to that of women born in the United States [Thesis]. New York, NY: Stony Brook University;2014.41. Elias SG, van Noord PA, Peeters PH, den Tonkelaar I, Grobbee DE. Caloric restriction reduces age at menopause: the effect of the 1944-1945 Dutch famine. Menopause. 2003; 10(5):399–405. PMID: 14501600.
Article42. Wang N, Huang Y, Wen J, Su Q, Huang Y, Cai L, et al. Early life exposure to famine and reproductive aging among Chinese women. Menopause. 2019; 26(5):463–468. PMID: 30516712.
Article43. Yarde F, Broekmans FJ, van der Pal-de Bruin KM, Schönbeck Y, te Velde ER, Stein AD, et al. Prenatal famine, birthweight, reproductive performance and age at menopause: the Dutch hunger winter families study. Hum Reprod. 2013; 28(12):3328–3336. PMID: 23966246.
Article44. Hardy R, Kuh D. Does early growth influence timing of the menopause? Evidence from a British birth cohort. Hum Reprod. 2002; 17(9):2474–2479. PMID: 12202444.
Article45. Wang M, Yi Y, Roebothan B, Colbourne J, Maddalena V, Wang PP, et al. Body mass index trajectories among middle-aged and elderly Canadians and associated health outcomes. J Environ Public Health. 2016; 2016:7014857. PMID: 26925112.
Article46. de Vries E, den Tonkelaar I, van Noord PA, van der Schouw YT, te Velde ER, Peeters PH. Oral contraceptive use in relation to age at menopause in the DOM cohort. Hum Reprod. 2001; 16(8):1657–1662. PMID: 11473959.47. van Noord PA, Dubas JS, Dorland M, Boersma H, te Velde E. Age at natural menopause in a population-based screening cohort: the role of menarche, fecundity, and lifestyle factors. Fertil Steril. 1997; 68(1):95–102. PMID: 9207591.
Article48. Daniels K, Abma JC. Current contraceptive status among women aged 15–49: United States, 2015–2017. Updated 2018. https://nchstats.com/2018/12/19/current-contraceptive-status-among-women-aged-15-49-united-states-2015-2017/.49. Pokoradi AJ, Iversen L, Hannaford PC. Factors associated with age of onset and type of menopause in a cohort of UK women. Am J Obstet Gynecol. 2011; 205(1):34.e1–34.13. PMID: 21514918.
Article50. Ferreira JM, Monteiro I, Castro S, Villarroel M, Silveira C, Bahamondes L. The use of long acting reversible contraceptives and the relationship between discontinuation rates due to menopause and to female and male sterilizations. Rev Bras Ginecol Obstet. 2016; 38(5):210–217. PMID: 27187927.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Current Status and the Perspectives of Nutrition Survey
- The Korea National Health and Nutrition Examination Survey (KNHANES): Current Status and Challenges
- Comparison of quality of life and related factors according to premature menopause using the Korea National Health and Nutrition Examination Survey (2014-2017)
- Complex sample design effects and inference for Korea National Health and Nutrition Examination Survey data
- The Korea National Health and Nutrition Examination Survey data linked Cause of Death data