J Korean Foot Ankle Soc.
2020 Dec;24(4):156-160. 10.14193/jkfas.2020.24.4.156.
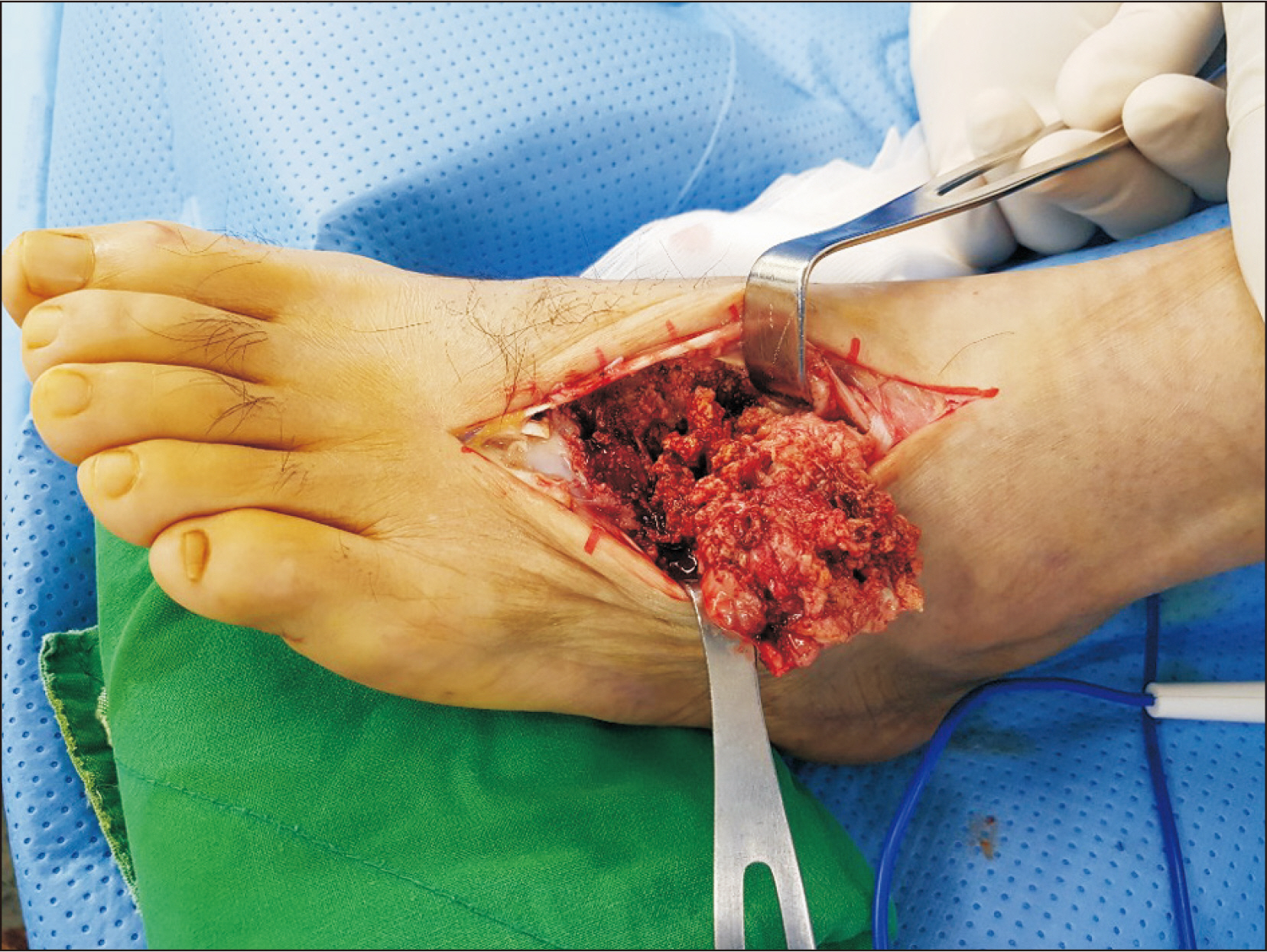
Intraosseous Malignant Peripheral Nerve Sheath Tumor of Multiple Bones of the Midfoot: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Kangdong Sacred Heart Hospital, Seoul, Korea
- KMID: 2509537
- DOI: http://doi.org/10.14193/jkfas.2020.24.4.156
Abstract
- Malignant peripheral nerve sheath tumors (MPNSTs) usually arise in soft tissues; they are rarely found in the bone. This paper reports a case of MPNST in the foot and ankle joint involving the distal tibia, talus, calcaneus, navicular, medial intermediate, and lateral cuneiform, cuboid, and 2nd to 4th metatarsal bone. Palliative treatment was performed. The authors encountered a patient with intraosseous MPNST of the midfoot who presented with nonspecific clinical and radiologic findings. This case shows that a high index of suspicion and a histopathology examination, including immunohistochemistry, will be necessary for an accurate diagnosis.
Keyword
Figure
Reference
-
1. Terry DG, Sauser DD, Gordon MD. 1998; Intraosseous malignant peripheral nerve sheath tumor in a patient with neurofibromatosis. Skeletal Ra-diol. 27:346–9. doi: 10.1007/s002560050395. DOI: 10.1007/s002560050395. PMID: 9677654.
Article2. Lesic A, Bumbasirevic M, Atkinson HD, Maksimovic R, Sopta J, Atanackovic M. 2006; Malignant intraosseous peripheral nerve sheath tumour of the proximal femur: a case report. J Orthop Surg (Hong Kong). 14:84–9. doi: 10.1177/230949900601400119. DOI: 10.1177/230949900601400119. PMID: 16598095.
Article3. Kendi TK, Erakar A, Yildiz HY, Saglik Y, Erekul S. 2004; Intraosseous malig-nant peripheral nerve sheath tumor with local recurrence, lung metas-tases and death. Skeletal Radiol. 33:223–5. doi: 10.1007/s00256-003-0678-1. DOI: 10.1007/s00256-003-0678-1. PMID: 14758514.
Article4. Sham ME, Ghorpade , Shetty A, Hari S, Vinay . 2010; Malignant peripheral nerve cell tumour. J Maxillofac Oral Surg. 9:68–71. doi: 10.1007/s12663-010-0019-6. DOI: 10.1007/s12663-010-0019-6. PMID: 23139572. PMCID: PMC3453695.
Article5. Ma ZW, Ward R, Hoda SA. 1996; Intraosseous malignant peripheral nerve sheath tumor. Arch Pathol Lab Med. 120:517–8.6. Dunnick NR. 2000; Image interpretation session: 1999. Intraosseous ma-lignant peripheral nerve sheath tumor (malignant schwannoma) in a patient with neurofibromatosis. Radiographics. 20:271–3. doi: 10.1148/radiographics.20.1.g00ja27257. DOI: 10.1148/radiographics.20.1.g00ja27257.7. Moon SJ, Lee JK, Seo BR, Kim JH, Kim SH, Lee KH, et al. 2008; An intraos-seous malignant peripheral nerve sheath tumor of the cervical spine: a case report and review of the literature. Spine. 33:E712–6. doi: 10.1097/BRS.0b013e31817e6995. DOI: 10.1097/BRS.0b013e31817e6995. PMID: 18758353.8. Stout AP. 1949; Tumors of the peripheral nervous system. J Mo State Med Assoc. 46:255–9.9. Moon MS, Kim HJ, Lee DS, Kim RK, Seo EJ. 1983; Malignant schwan-noma (a case report). J Korean Orthop Assoc. 18:1029–32. doi: 10.4055/jkoa.1983.18.5.1029. DOI: 10.4055/jkoa.1983.18.5.1029.
Article10. Muthusamy S, Conway SA, Pitcher JD, Temple HT. 2017; Primary intraos-seous malignant peripheral nerve sheath tumor of the medial cunei-form: a case report and review of the literature. J Foot Ankle Surg. 56:129–34. doi: 10.1053/j.jfas.2016.05.013. DOI: 10.1053/j.jfas.2016.05.013. PMID: 27449524.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Peripheral Nerve Sheath Tumor of the Larynx
- Malignant Peripheral Nerve Sheath Tumor of the Cauda Equina in Type I Neurofibromatosis: Case Report
- Intraosseous Nerve Sheath Tumors in the Jaws
- A Case of Malignant Peripheral Nerve Sheath Tumor in Parapharyngeal Space
- A Case of Malignant Peripheral Nerve Sheath Tumor on Paranasal Sinus