J Korean Foot Ankle Soc.
2020 Dec;24(4):129-134. 10.14193/jkfas.2020.24.4.129.
A Comparison of Proximal and Distal Chevron Osteotomy for the Correction of Severe Hallux Valgus Deformity
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Chosun University, Gwangju, Korea
- KMID: 2509533
- DOI: http://doi.org/10.14193/jkfas.2020.24.4.129
Abstract
- Purpose
This study compared the results of proximal and distal chevron osteotomy in patients with severe hallux valgus. Several recent studies have shown that the indications for distal metatarsal osteotomy with a distal soft-tissue procedure could be extended to include severe hallux valgus.
Materials and Methods
This study analyzed 127 severe hallux valgus surgeries. Of these, 76 patients (76 feet) were excluded for lack of adequate follow-up and additional procedures (Akin procedure), leaving 51 patients (51 feet) in the study. The mean age of the patients was 58 years (21~83 years), and the mean follow-up duration was 18 months (12~32 months). The patients were divided into two groups. Group 1 underwent distal chevron osteotomy, and group 2 underwent proximal chevron osteotomy performed sequentially by a single surgeon. The patients were interviewed for the American Orthopaedic Foot and Ankle Society (AOFAS) score before and one year after surgery. The anteroposterior weight-bearing radiography of the foot was taken before and one year after surgery.
Results
There were no significant differences in pain and function after one year in either group. Both groups experienced significant pain reduction and an increase in the AOFAS score. Significant improvement of the hallux valgus and intermetatarsal angle corrections was observed in both groups, and the sesamoid position was similar in each group. More improvement in radiographic correction of intermetatarsal angle was noted in group 2. Both procedures gave similar good clinical and radiological outcomes.
Conclusion
This study suggests that a distal chevron osteotomy with a distal soft-tissue procedure is as effective and reliable a means of correcting severe hallux valgus as a proximal chevron osteotomy with a distal soft-tissue procedure.
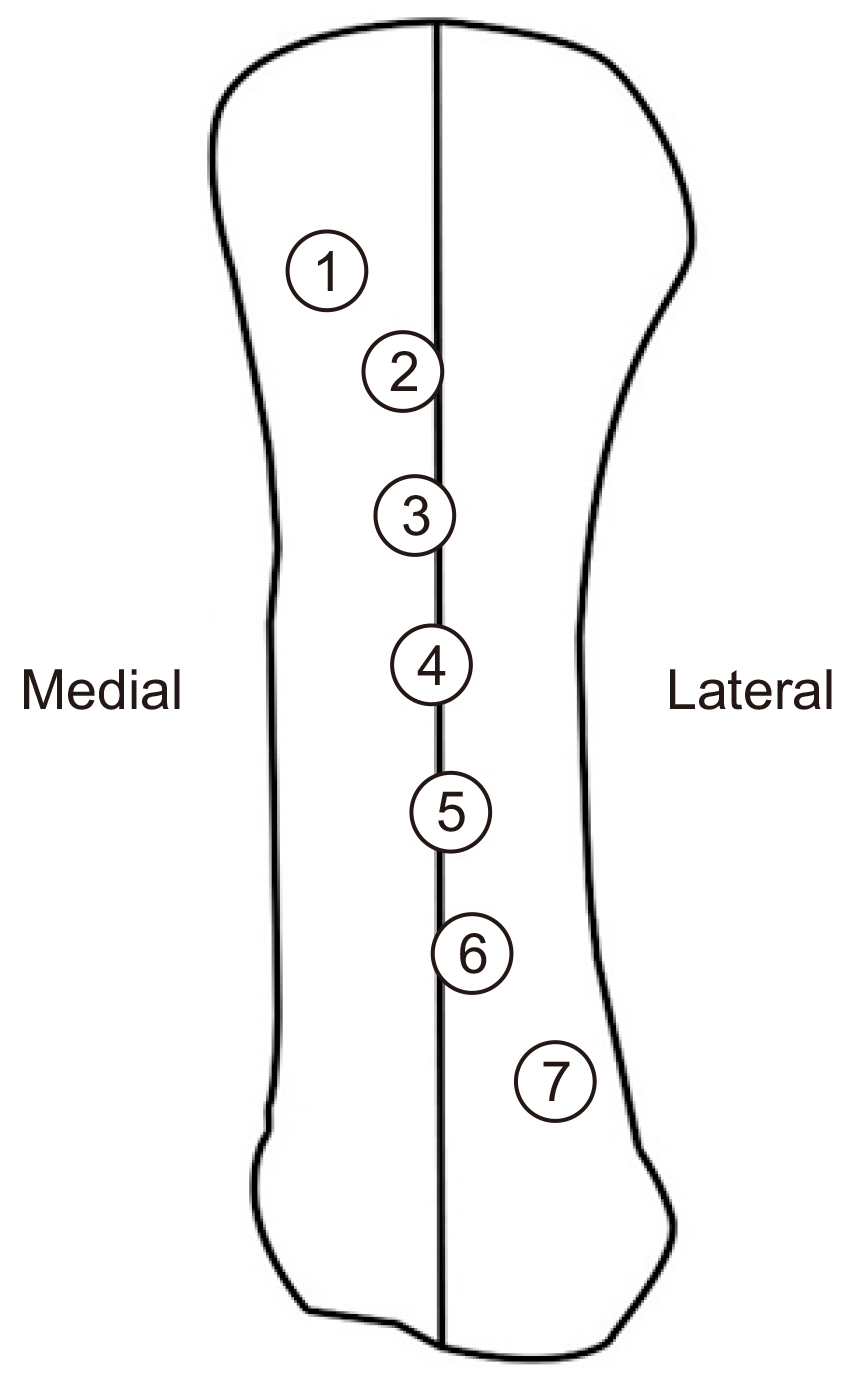
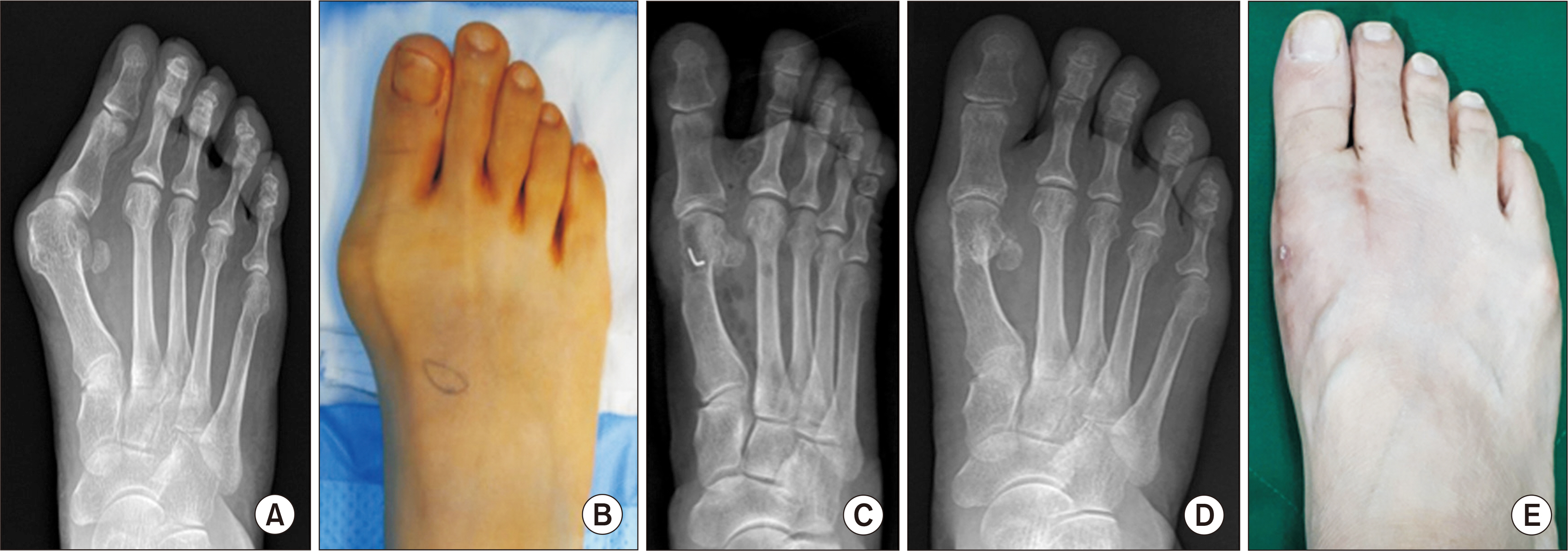
Figure
Reference
-
1. Mann RA. 1986; Hallux valgus. Instr Course Lect. 35:339–53.2. Donnelly RE, Saltzman CL, Kile TA, Johnson KA. 1994; Modified chevron osteotomy for hallux valgus. Foot Ankle Int. 15:642–5. doi: 10.1177/107110079401501202. DOI: 10.1177/107110079401501202. PMID: 7894634.
Article3. Klosok JK, Pring DJ, Jessop JH, Maffulli N. 1993; Chevron or Wilson metatarsal osteotomy for hallux valgus. A prospective randomised trial. J Bone Joint Surg Br. 75:825–9. doi: 10.1302/0301-620X. DOI: 10.1302/0301-620X.75B5.8376450. PMID: 8376450.
Article4. Bai LB, Lee KB, Seo CY, Song EK, Yoon TR. 2010; Distal chevron osteotomy with distal soft tissue procedure for moderate to severe hallux valgus deformity. Foot Ankle Int. 31:683–8. doi: 10.3113/FAI.2010.0683. DOI: 10.3113/FAI.2010.0683. PMID: 20727316.
Article5. Sanhudo JA. 2006; Correction of moderate to severe hallux valgus deformity by a modified chevron shaft osteotomy. Foot Ankle Int. 27:581–5. doi: 10.1177/107110070602700803. DOI: 10.1177/107110070602700803. PMID: 16919209.
Article6. Yoo WJ, Chung MS, Baek GH, Yu CH, Moon HJ. 2008; Distal chevron osteotomy for moderate to severe hallux valgus deformity in patients aged 50 or older. J Korean Orthop Assoc. 43:445–50. doi: 10.4055/. DOI: 10.4055/jkoa.2008.43.4.445.
Article7. Bluth D, Borgeas AT, Brennan RL. Hara B, Locke R, Lowe W, editors. American college of foot surgeons. 1976. Biomechanical considerations. Complications in foot surgery: prevention and management. Williams & Wilkins;Baltimore (MD): p. 41–66.8. Rowe SM, Lee KB, Choi J, Cheon SY, Hur CI. 2005; Radiographic changes in forefoot geometry with weightbearing: hallux valgus angle, intermetatarsal angle, and medial sesamoid. J Korean Foot Ankle Soc. 9:13–9.9. Easley ME, Trnka HJ. 2007; Radiographic changes in forefoot geometry with weightbearing: hallux valgus angle, intermetatarsal angle, and medial sesamoid. Foot Ankle Int. 28:748–58. doi: 10.3113/. DOI: 10.3113/FAI.2007.0748. PMID: 17592710.10. Coughlin MJ, Jones CP. 2007; Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 28:759–77. doi: 10.3113/. DOI: 10.3113/FAI.2007.0759. PMID: 17666168.11. Wang X, Jiang JY, Ma X, Huang JZ, Gu XJ. 2009; Management of the second and third metatarsal in moderate and severe hallux valgus. Orthopedics. 32:892. doi: 10.3928/01477447-20091020-08. DOI: 10.3928/01477447-20091020-08. PMID: 19968220.
Article12. Garrido IM, Rubio ER, Bosch MN, González MS, Paz GB, Llabrés AJ. 2008; Scarf and Akin osteotomies for moderate and severe hallux valgus: clinical and radiographic results. Foot Ankle Surg. 14:194–203. doi: 10.1016/j.fas.2008.02.003. DOI: 10.1016/j.fas.2008.02.003. PMID: 19083642.13. De Lavigne C, Rasmont Q, Hoang B. 2011; Percutaneous double metatarsal osteotomy for correction of severe hallux valgus deformity. Acta Orthop Belg. 77:516–21.14. Sammarco GJ, Idusuyi OB. 2001; Complications after surgery of the hallux. Clin Orthop Relat Res. (391):59–71. doi: 10.1097/00003086-. DOI: 10.1097/00003086-200110000-00008. PMID: 11603690.
Article15. Potenza V, Caterini R, Farsetti P, Forconi F, Savarese E, Nicoletti S, et al. 2009; Chevron osteotomy with lateral release and adductor tenotomy for hallux valgus. Foot Ankle Int. 30:512–6. doi: 10.3113/. DOI: 10.3113/FAI.2009.0512. PMID: 19486628.16. Trnka HJ, Zembsch A, Easley ME, Salzer M, Ritschl P, Myerson MS. 2000; The chevron osteotomy for correction of hallux valgus. J Bone Joint Surg Am. 82:1373–8. DOI: 10.2106/00004623-200010000-00002. PMID: 11057464.
Article17. Miller JW. 1974; Distal first metatarsal displacement osteotomy. J Bone Joint Surg Am. 56:923–31. DOI: 10.2106/00004623-197456050-00005.
Article18. Rush SM, Christensen JC, Johnson CH. 2000; Biomechanics of the first ray. J Foot Ankle Surg. 39:68–77. doi: 10.1016/s1067-2516(00)80030-7. DOI: 10.1016/S1067-2516(00)80030-7.19. Jung HG, Eom JS. Jung HG, editor. 2016. Hallux valgus and bunionette. Foot and ankle disorders. Springer-Verlag;Berlin, Heidelberg: p. 1–55. DOI: 10.1007/978-3-642-54493-4_1.
Article20. Deenik A, van Mameren H, de Visser E, de Waal Malefijt M, Draijer F, de Bie R. 2008; Equivalent correction in scarf and chevron osteotomy in moderate and severe hallux valgus: a randomized controlled trial. Foot Ankle Int. 29:1209–15. doi: 10.3113/FAI.2008.1209. DOI: 10.3113/FAI.2008.1209. PMID: 19138485.
Article21. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Shima H. 2008; Proximal metatarsal osteotomy for hallux valgus: comparison of outcome for moderate and severe deformities. Foot Ankle Int. 29:664–70. doi: 10.3113/FAI.2008.0664. DOI: 10.3113/FAI.2008.0664. PMID: 18785415.
Article22. Chuckpaiwong B. 2012; Comparing proximal and distal metatarsal osteotomy for moderate to severe hallux valgus. Int Orthop. 36:2275–8. doi: 10.1007/s00264-012-1656-9. DOI: 10.1007/s00264-012-1656-9. PMID: 22986505. PMCID: PMC3479288.
Article23. Park CH, Jang JH, Lee SH, Lee WC. 2013; A comparison of proximal and distal chevron osteotomy for the correction of moderate hallux valgus deformity. Bone Joint J. 95(B):649–56. doi: 10.1302/0301-620X.95B5.30181. DOI: 10.1302/0301-620X.95B5.30181. PMID: 23632675.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chevron Osteotomy as the Treatment of Moderate to Severe Hallux Valgus Deformity
- Comparison of Proximal and Modified Distal Chevron Osteotomy for the Treatment of Moderate to Severe Hallux Valgus Deformity
- Comparison of Proximal Metatarsal Osteotomy andDistal Chevron Osteotomy for Correction of Hallux Valgus
- The Results of Distal Chevron Osteotomy with Lateral Soft Tissue Release for Hallux Valgus Deformity
- Comparison of Operative Results of Distal Chevron Osteotomy with and without Akin Osteotomy for Moderate to Severe Hallux Valgus