J Cardiovasc Imaging.
2020 Apr;28(2):109-120. 10.4250/jcvi.2019.0094.
Echocardiographic Assessment of Right Ventriculo-arterial Coupling: Clinical Correlates and Prognostic Impact in Heart Failure Patients Undergoing Cardiac Resynchronization Therapy
- Affiliations
-
- 1Instituto de Ciências Biomédicas Abel Salazar, University of Porto, Porto, Portugal
- 2Centro Hospitalar Universitário do Porto, Porto, Portugal
- KMID: 2509453
- DOI: http://doi.org/10.4250/jcvi.2019.0094
Abstract
- BACKGROUND
Right ventriculo-arterial coupling (RV-PA) can be estimated by echocardiography using the ratio between tricuspid annular plane systolic excursion (TAPSE) and pulmonary artery systolic pressure (PASP) and it has prognostic value in the general heart failure (HF) population. We aimed to study the clinical correlates and prognostic value of RV-PA in HF patients undergoing cardiac resynchronization therapy (CRT).
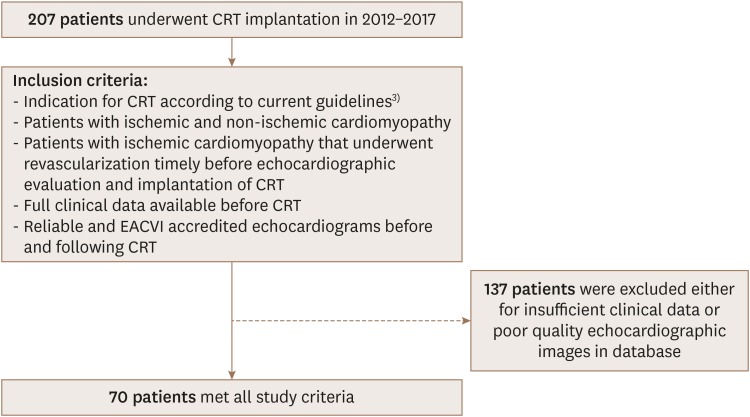
METHODS
We retrospectively studied 70 HF patients undergoing CRT implantation.
RESULTS
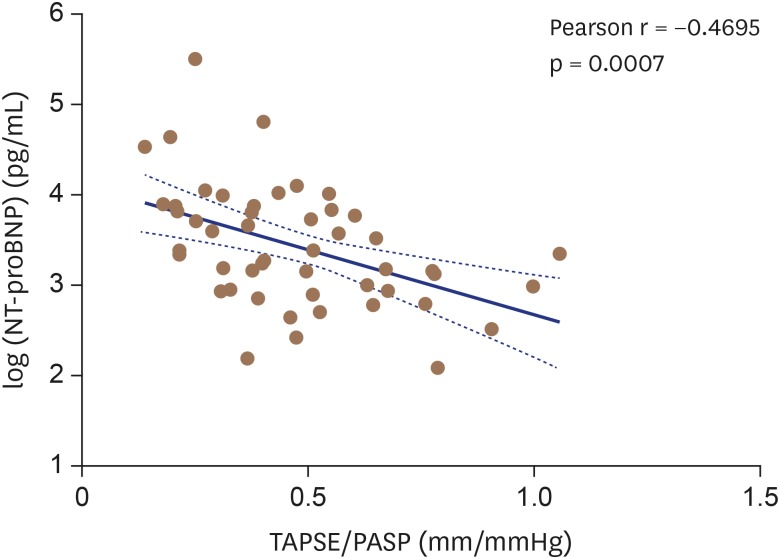
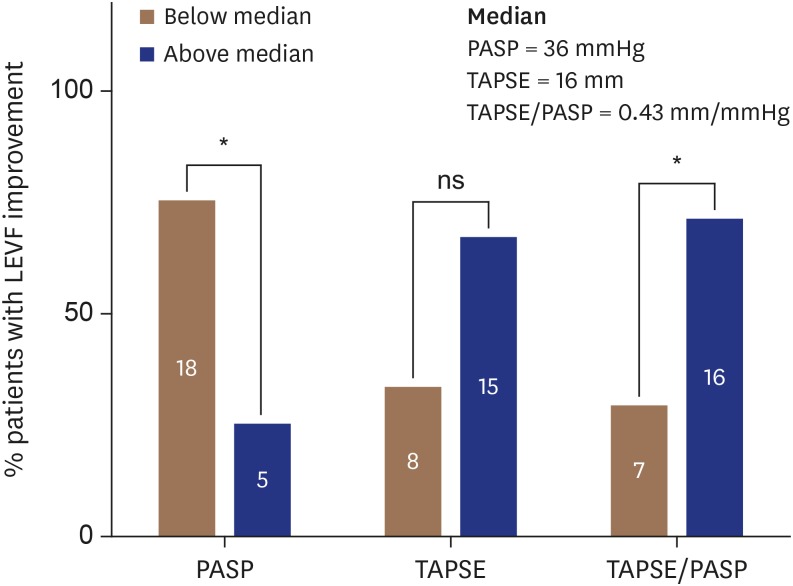
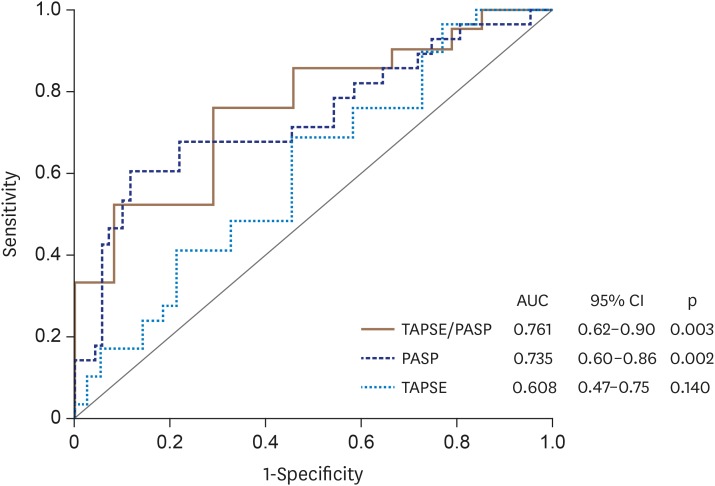
RV-PA coupling was estimated by TAPSE/PASP ratio using baseline echocardiography. Non-response to CRT was defined as improvement of left ventricular ejection fraction < 5% in a follow-up echo 6-12 months after CRT. Those with lower TAPSE/PASP ratios (worse RV-PA coupling) had higher NT-proBNP concentrations and increased E/e′ ratio. TAPSE/PASP ratio and PASP, but not TAPSE, predicted nonresponse to CRT with TAPSE/PASP ratio showing the best discriminative ability with a sensitivity of 76% and specificity of 71%. Among these parameters, PASP independently predicted all-cause mortality.
CONCLUSIONS
RV-PA coupling estimated by TAPSE/PASP ratio was associated with established prognostic markers in HF. It numerically outperformed PASP and TAPSE in predicting the response to CRT. Our data suggest that this simple and widely available echocardiographic parameter conveys significant pathophysiological and prognostic meaning in HF patients undergoing CRT.
Keyword
Figure
Reference
-
1. Goldenberg I, Kutyifa V, Klein HU, et al. Survival with cardiac-resynchronization therapy in mild heart failure. N Engl J Med. 2014; 370:1694–1701. PMID: 24678999.2. Chinitz JS, d'Avila A, Goldman M, Reddy V, Dukkipati S. Cardiac resynchronization therapy: who benefits? Ann Glob Health. 2014; 80:61–68. PMID: 24751566.3. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129–2200. PMID: 27206819.4. Mullens W, Grimm RA, Verga T, et al. Insights from a cardiac resynchronization optimization clinic as part of a heart failure disease management program. J Am Coll Cardiol. 2009; 53:765–773. PMID: 19245967.5. Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001; 37:183–188. PMID: 11153735.6. Guazzi M, Bandera F, Pelissero G, et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol. 2013; 305:H1373–H1381. PMID: 23997100.7. Filippetti L, Voilliot D, Bellino M, Citro R, Go YY, Lancellotti P. The right heart-pulmonary circulation unit and left heart valve disease. Heart Fail Clin. 2018; 14:431–442. PMID: 29966640.8. Chatterjee NA, Upadhyay GA, Singal G, et al. Pre-capillary pulmonary hypertension and right ventricular dilation predict clinical outcome in cardiac resynchronization therapy. JACC Heart Fail. 2014; 2:230–237. PMID: 24952689.9. Stern J, Heist EK, Murray L, et al. Elevated estimated pulmonary artery systolic pressure is associated with an adverse clinical outcome in patients receiving cardiac resynchronization therapy. Pacing Clin Electrophysiol. 2007; 30:603–607. PMID: 17461868.10. Burri H, Domenichini G, Sunthorn H, et al. Right ventricular systolic function and cardiac resynchronization therapy. Europace. 2010; 12:389–394. PMID: 19966321.11. van Everdingen WM, Walmsley J, Cramer MJ, et al. Echocardiographic prediction of cardiac resynchronization therapy response requires analysis of both mechanical dyssynchrony and right ventricular function: a combined analysis of patient data and computer simulations. J Am Soc Echocardiogr. 2017; 30:1012–1020.e2. PMID: 28801203.12. Szulik M, Streb W, Lenarczyk R, et al. The incremental value of right ventricular indices for predicting response to cardiac resynchronization therapy. J Am Soc Echocardiogr. 2011; 24:170–179.e3. PMID: 21177070.13. Ricci F, Mele D, Bianco F, Bucciarelli V, De Caterina R, Gallina S. Right heart-pulmonary circulation unit and cardiac resynchronization therapy. Am Heart J. 2017; 185:1–16. PMID: 28267462.14. Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiéry JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016; 37:942–954. PMID: 26508169.15. Aronson D, Eitan A, Dragu R, Burger AJ. Relationship between reactive pulmonary hypertension and mortality in patients with acute decompensated heart failure. Circ Heart Fail. 2011; 4:644–650. PMID: 21606213.16. Guazzi M, Dixon D, Labate V, et al. RV contractile function and its coupling to pulmonary circulation in heart failure with preserved ejection fraction: stratification of clinical phenotypes and outcomes. JACC Cardiovasc Imaging. 2017; 10:1211–1221. PMID: 28412423.17. Guazzi M, Naeije R. Pulmonary hypertension in heart failure: pathophysiology, pathobiology, and emerging clinical perspectives. J Am Coll Cardiol. 2017; 69:1718–1734. PMID: 28359519.18. Guazzi M, Naeije R, Arena R, et al. Echocardiography of right ventriculoarterial coupling combined with cardiopulmonary exercise testing to predict outcome in heart failure. Chest. 2015; 148:226–234. PMID: 25633590.19. Tello K, Wan J, Dalmer A, et al. Validation of the tricuspid annular plane systolic excursion/systolic pulmonary artery pressure ratio for the assessment of right ventricular-arterial coupling in severe pulmonary hypertension. Circ Cardiovasc Imaging. 2019; 12:e009047. PMID: 31500448.20. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–612. PMID: 19414839.21. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.22. Chung K, Strange G, Codde J, Celermajer D, Scalia GM, Playford D. Left heart disease and pulmonary hypertension: are we seeing the full picture? Heart Lung Circ. 2018; 27:301–309. PMID: 29102471.23. Brenyo A, Barsheshet A, Rao M, et al. Brain natriuretic peptide and cardiac resynchronization therapy in patients with mildly symptomatic heart failure. Circ Heart Fail. 2013; 6:998–1004. PMID: 23801020.24. Aksoy H, Okutucu S, Kaya EB, et al. Clinical and echocardiographic correlates of improvement in left ventricular diastolic function after cardiac resynchronization therapy. Europace. 2010; 12:1256–1261. PMID: 20478931.25. Venkateswaran RV, Freeman C, Chatterjee N, et al. Anemia and its association with clinical outcome in heart failure patients undergoing cardiac resynchronization therapy. J Interv Card Electrophysiol. 2015; 44:297–304. PMID: 26453528.26. Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005; 352:1011–1023. PMID: 15758012.27. Berger R, Shankar A, Fruhwald F, et al. Relationships between cardiac resynchronization therapy and N-terminal pro-brain natriuretic peptide in patients with heart failure and markers of cardiac dyssynchrony: an analysis from the Cardiac Resynchronization in Heart Failure (CARE-HF) study. Eur Heart J. 2009; 30:2109–2116. PMID: 19493864.28. Fruhwald FM, Fahrleitner-Pammer A, Berger R, et al. Early and sustained effects of cardiac resynchronization therapy on N-terminal pro-B-type natriuretic peptide in patients with moderate to severe heart failure and cardiac dyssynchrony. Eur Heart J. 2007; 28:1592–1597. PMID: 17298973.29. Bakos Z, Chatterjee NC, Reitan C, Singh JP, Borgquist R. Prediction of clinical outcome in patients treated with cardiac resynchronization therapy - the role of NT-ProBNP and a combined response score. BMC Cardiovasc Disord. 2018; 18:70. PMID: 29699498.30. Whalley GA, Gamble GD, Doughty RN. The prognostic significance of restrictive diastolic filling associated with heart failure: a meta-analysis. Int J Cardiol. 2007; 116:70–77. PMID: 16901562.31. Meta-analysis Research Group in Echocardiography (MeRGE) Heart Failure Collaborators. Doughty RN, Klein AL, et al. Independence of restrictive filling pattern and LV ejection fraction with mortality in heart failure: an individual patient meta-analysis. Eur J Heart Fail. 2008; 10:786–792. PMID: 18617438.32. Gradaus R, Stuckenborg V, Löher A, et al. Diastolic filling pattern and left ventricular diameter predict response and prognosis after cardiac resynchronisation therapy. Heart. 2008; 94:1026–1031. PMID: 17984216.33. Facchini E, Varalda M, Sartori C, Burkhoff D, Marino PN. Systolic heart failure and cardiac resynchronization therapy: a focus on diastole. Int J Cardiovasc Imaging. 2014; 30:897–905. PMID: 24706254.34. Campbell P, Takeuchi M, Bourgoun M, et al. Right ventricular function, pulmonary pressure estimation, and clinical outcomes in cardiac resynchronization therapy. Circ Heart Fail. 2013; 6:435–442. PMID: 23524528.35. Sharma A, Lavie CJ, Vallakati A, et al. Changes in parameters of right ventricular function with cardiac resynchronization therapy. Clin Cardiol. 2017; 40:1033–1043. PMID: 28898433.36. Sharma A, Bax JJ, Vallakati A, et al. Meta-analysis of the relation of baseline right ventricular function to response to cardiac resynchronization therapy. Am J Cardiol. 2016; 117:1315–1321. PMID: 26879068.37. Bosch L, Lam CSP, Gong L, et al. Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur J Heart Fail. 2017; 19:1664–1671. PMID: 28597497.38. Martens P, Verbrugge FH, Bertrand PB, et al. Effect of cardiac resynchronization therapy on exercise-induced pulmonary hypertension and right ventricular-arterial coupling. Circ Cardiovasc Imaging. 2018; 11:e007813. PMID: 30354673.39. Schmeisser A, Rauwolf T, Ghanem A, et al. Right heart function interacts with left ventricular remodeling after CRT: A pressure volume loop study. Int J Cardiol. 2018; 268:156–161. PMID: 29548538.40. Shalaby A, Voigt A, El-Saed A, Saba S. Usefulness of pulmonary artery pressure by echocardiography to predict outcome in patients receiving cardiac resynchronization therapy heart failure. Am J Cardiol. 2008; 101:238–241. PMID: 18178413.41. Wang J, Su Y, Bai J, Wang W, Qin S, Ge J. Elevated pulmonary artery pressure predicts poor outcome after cardiac resynchronization therapy. J Interv Card Electrophysiol. 2014; 40:171–178. PMID: 24728706.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implication of Echocardiographic-Based Right Ventriculo-arterial Coupling in Cardiac Resynchronization Referred Patients
- Clinical Implication of Mechanical Dyssynchrony in Heart Failure
- Implantable Cardioverter-Defibrillator and Cardiac Resynchronization Therapy
- The Past, Present and Future of Cardiac Resynchronization Therapy
- Cardiac Resynchronization Therapy Defibrillator Treatment in a Child with Heart Failure and Ventricular Arrhythmia