J Korean Med Sci.
2020 Dec;35(47):e418. 10.3346/jkms.2020.35.e418.
Three-month Follow-up Study of Survivors of Coronavirus Disease 2019 after Discharge
- Affiliations
-
- 1Department of Respiratory and Critical Care Medicine, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- KMID: 2509450
- DOI: http://doi.org/10.3346/jkms.2020.35.e418
Abstract
- Background
Most patients including health care workers (HCWs) survived the coronavirus disease 2019 (COVID-19), however, knowledge about the sequelae of COVID-19 after discharge remains limited.
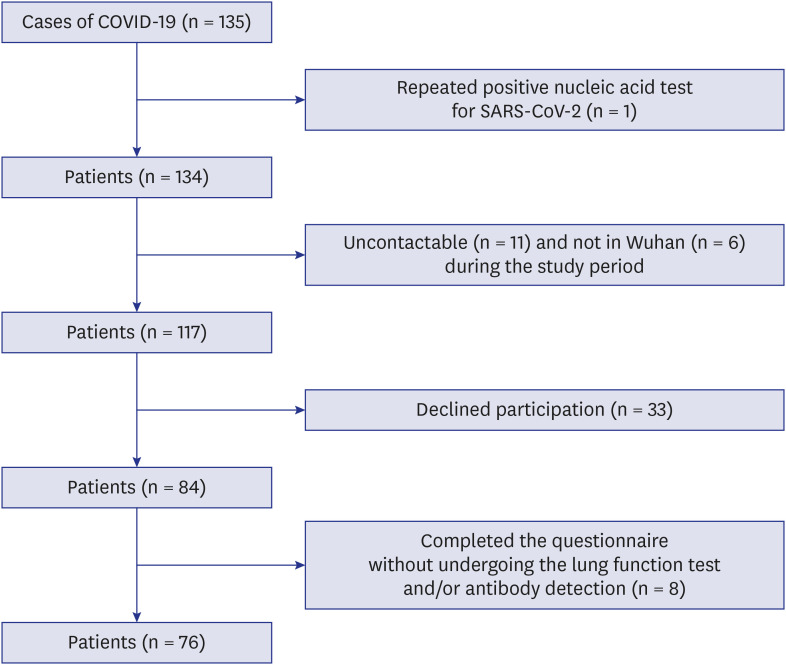
Methods
A prospectively observational 3-month follow-up study evaluated symptoms, dynamic changes of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) IgG and IgM, lung function, and high resolution computed tomography (HRCT) of survivors of COVID-19 after discharge at Wuhan Union Hospital, China.
Results
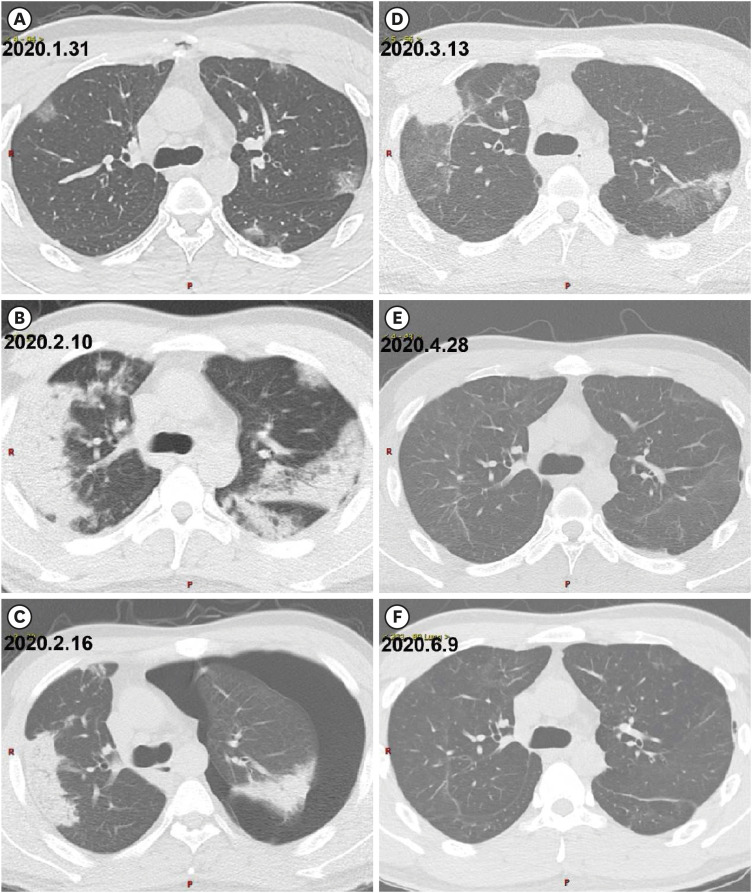
Seventy-six survivors (55 females) with a mean age of 41.3 ± 13.8 years were enrolled, and 65 (86%) were HCWs. A total of 69 (91%) patients had returned to their original work at 3-months after discharge. Most of the survivors had symptoms including fever, sputum production, fatigue, diarrhea, dyspnea, cough, chest tightness on exertion and palpitations in the three months after discharge. The serum troponin-I levels during the acute illness showed high correlation with the symptom of fatigue after hospital discharge (r = 0.782; P = 0.008) and lymphopenia was correlated with the symptoms of chest tightness and palpitations on exertion of patients after hospital discharge (r = −0.285, P = 0.027; r = −0.363, P = 0.004, respectively). The mean values of forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), FEV1/FVC, total lung capacity and diffusion capacity were all normal (> 80% predicted) and lung HRCTs returned to normal in most of the patients (82%), however, 42% of survivors had mild pulmonary function abnormalities at 3-months after discharge. SARS-CoV-2 IgG turned negative in 11% (6 of 57 patients), 8% (4 of 52 patients) and 13% (7 of 55 patients), and SARS-CoV-2 IgM turned negative in 72% (41 of 57 patients), 85% (44 of 52 patients) and 87% (48 of 55 patients) at 1-month, 2-months and 3-months after discharge, respectively.
Conclusion
Infection by SARS-CoV-2 caused some mild impairments of survivors within the first three months of their discharge and the duration of SARS-CoV-2 antibody was limited, which indicates the necessity of long-term follow-up of survivors of COVID-19.
Keyword
Figure
Cited by 1 articles
-
Comprehensive Rehabilitation in Severely Ill Inpatients With COVID-19: A Cohort Study in a Tertiary Hospital
Hyeonseong Woo, Sanghee Lee, Hyun Sung Lee, Hyun Jun Chae, Jongtak Jung, Myung Jin Song, Sung Yoon Lim, Yeon Joo Lee, Young-Jae Cho, Eu Suk Kim, Hong Bin Kim, Jae-Young Lim, Kyoung-Ho Song, Jaewon Beom
J Korean Med Sci. 2022;37(34):e262. doi: 10.3346/jkms.2022.37.e262.
Reference
-
1. Johns Hopkins University & Medicine. Coronavirus COVID-19 global cases by the Center for Systems Science and Engineering (CSSE). Updated 2020. Accessed July 24, 2020. https://coronavirus.jhu.edu/map.html.2. The Wuhan Municipal Headquarters for COVID-19 Epidemic Prevention and Control. Full text of Wuhan’s notification on revising numbers of confirmed COVID-19 cases, deaths. Wuhan, China: The Wuhan Municipal Headquarters for COVID-19 Epidemic. Prev Control. 2020.3. World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Geneva: World Health Organization;2020.4. National Health Commission of the People's Republic of China. Diagnosis and Treatment Program of New Coronary Pneumonia. 7th ed. Beijing: Department of Medical Administration, Ministry of Health (MOH) of the PRC;2020.5. Wang X, Zhou Q, He Y, Liu L, Ma X, Wei X, et al. Nosocomial outbreak of COVID-19 pneumonia in Wuhan, China. Eur Respir J. 2020; 55(6):2000544. PMID: 32366488.
Article6. Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med. 2019; 200(8):e70–88. PMID: 31613151.
Article7. Stocks J, Quanjer PH. Official Statement of The European Respiratory Society. Reference values for residual volume, functional residual capacity and total lung capacity. ATS Workshop on Lung Volume Measurements. Eur Respir J. 1995; 8(3):492–506. PMID: 7789503.8. Graham BL, Brusasco V, Burgos F, Cooper BG, Jensen R, Kendrick A, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. 2017; 49(1):1600016. PMID: 28049168.
Article9. Hsu HH, Tzao C, Wu CP, Chang WC, Tsai CL, Tung HJ, et al. Correlation of high-resolution CT, symptoms, and pulmonary function in patients during recovery from severe acute respiratory syndrome. Chest. 2004; 126(1):149–158. PMID: 15249456.
Article10. Antonio GE, Wong KT, Hui DS, Wu A, Lee N, Yuen EH, et al. Thin-section CT in patients with severe acute respiratory syndrome following hospital discharge: preliminary experience. Radiology. 2003; 228(3):810–815. PMID: 12805557.
Article11. Ooi GC, Khong PL, Müller NL, Yiu WC, Zhou LJ, Ho JC, et al. Severe acute respiratory syndrome: temporal lung changes at thin-section CT in 30 patients. Radiology. 2004; 230(3):836–844. PMID: 14990845.
Article12. Society AT. American Thoracic Society. Evaluation of impairment/disability secondary to respiratory disorders. Am Rev Respir Dis. 1986; 133(6):1205–1209. PMID: 3509148.13. Böhm M, Frey N, Giannitsis E, Sliwa K, Zeiher AM. Coronavirus disease 2019 (COVID-19) and its implications for cardiovascular care: expert document from the German Cardiac Society and the World Heart Federation. Clin Res Cardiol. Forthcoming 2020. DOI: 10.1007/s00392-020-01656-3.
Article14. Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020; 12(4):372–389.
Article15. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020; 395(10234):1417–1418. PMID: 32325026.
Article16. Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5(11):1265–1273. PMID: 32730619.
Article17. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497–506. PMID: 31986264.
Article18. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061–1069. PMID: 32031570.
Article19. Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020; 13(11):2330–2339. PMID: 32763118.
Article20. Shah P, Doshi R, Chenna A, Owens R, Cobb A, Ivey H, et al. Prognostic value of elevated cardiac troponin i in hospitalized Covid-19 patients. Am J Cardiol. 2020; 135:150–153. PMID: 32861733.
Article21. Fathi N, Rezaei N. Lymphopenia in COVID-19: therapeutic opportunities. Cell Biol Int. 2020; 44(9):1792–1797. PMID: 32458561.
Article22. Liu J, Li S, Liu J, Liang B, Wang X, Wang H, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020; 55:102763. PMID: 32361250.
Article23. Ong KC, Ng AW, Lee LS, Kaw G, Kwek SK, Leow MK, et al. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur Respir J. 2004; 24(3):436–442. PMID: 15358703.
Article24. Park WB, Jun KI, Kim G, Choi JP, Rhee JY, Cheon S, et al. Correlation between pneumonia severity and pulmonary complications in Middle East respiratory syndrome. J Korean Med Sci. 2018; 33(24):e169. PMID: 29892209.
Article25. Hui DS, Joynt GM, Wong KT, Gomersall CD, Li TS, Antonio G, et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005; 60(5):401–409. PMID: 15860716.
Article26. Ng CK, Chan JW, Kwan TL, To TS, Chan YH, Ng FY, et al. Six month radiological and physiological outcomes in severe acute respiratory syndrome (SARS) survivors. Thorax. 2004; 59(10):889–891. PMID: 15454656.
Article27. Ong KC, Ng AW, Lee LS, Kaw G, Kwek SK, Leow MK, et al. 1-year pulmonary function and health status in survivors of severe acute respiratory syndrome. Chest. 2005; 128(3):1393–1400. PMID: 16162734.
Article28. Hui DS, Wong KT, Ko FW, Tam LS, Chan DP, Woo J, et al. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest. 2005; 128(4):2247–2261. PMID: 16236881.
Article29. Ngai JC, Ko FW, Ng SS, To KW, Tong M, Hui DS. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010; 15(3):543–550. PMID: 20337995.
Article30. Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003; 348(8):683–693. PMID: 12594312.
Article31. Xiang F, Wang X, He X, Peng Z, Yang B, Zhang J, et al. Antibody detection and dynamic characteristics in patients with coronavirus disease 2019. Clin Infect Dis. 2020; 71(8):1930–1934. PMID: 32306047.
Article32. Cao WC, Liu W, Zhang PH, Zhang F, Richardus JH. Disappearance of antibodies to SARS-associated coronavirus after recovery. N Engl J Med. 2007; 357(11):1162–1163. PMID: 17855683.
Article33. Choe PG, Perera RA, Park WB, Song KH, Bang JH, Kim ES, et al. MERS-CoV antibody responses 1 year after symptom onset, South Korea, 2015. Emerg Infect Dis. 2017; 23(7):1079–1084.
Article34. Xia Z, Liu X, Hu X, Zhong Z, Wang Y, Peng G, et al. Failed antibody response in a renal transplant recipient with SARS-CoV-2 infected. Transpl Infect Dis. 2020; e13349:e13349.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of New Frailty at Hospital Discharge in Severe COVID-19 Survivors and Its Associated Factors
- Current Treatments of Coronavirus Disease 2019 in Elderly
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Insomnia Disorder Among Coronavirus Disease Survivors: A South Korean Nationwide Cohort Study
- Hemopneumothorax as an Unusual and Delayed Complication of Coronavirus Disease 2019 Pneumonia: A Case Report