J Korean Med Sci.
2020 Dec;35(47):e402. 10.3346/jkms.2020.35.e402.
Comparison of Suicide Risk by Mental Illness: a Retrospective Review of 14-Year Electronic Medical Records
- Affiliations
-
- 1Department of Neuropsychiatry, Seoul National University Hospital, Seoul, Korea
- 2Department of Psychiatry, Seoul National University College of Medicine, Seoul, Korea
- 3Institute of Human Behavioral Medicine, Seoul National University Medical Research Center, Seoul, Korea
- KMID: 2509445
- DOI: http://doi.org/10.3346/jkms.2020.35.e402
Abstract
- Background
Korea is one of the countries with the highest rate of suicide, while suicidality is known to be closely related to mental illnesses. The study aimed to evaluate the suicide rates in psychiatric patients, to compare it to that of the general population, and to investigate the differences among psychiatric diagnoses and comorbidities.
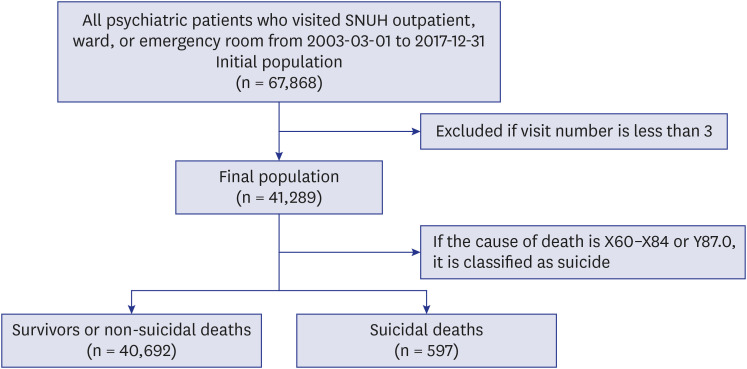
Methods
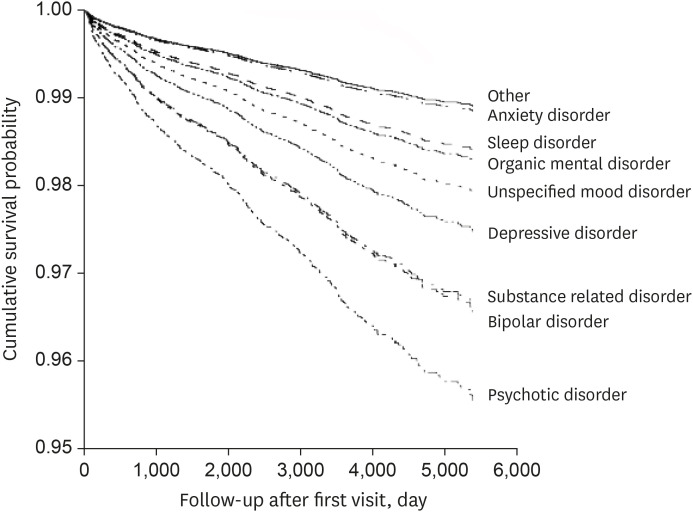
Medical records and mortality statistics of psychiatric patients at Seoul National University Hospital from 2003 to 2017 were reviewed. The standardized mortality ratio (SMR) for suicide was calculated to compare the psychiatric patients with the general population. The diagnosis-specific standardized mortality rate and hazard ratio (HR) were adjusted by age, sex, and psychiatric comorbidity (i.e., personality disorder and/or pain disorder).
Results
A total of 40,692 survivors or non-suicidal deaths and 597 suicidal death were included. The suicide rate among psychiatric patients was 5.13-fold higher than that of the general population. Psychotic disorder had the highest SMR (13.03; 95% confidence interval [CI], 11.23–15.03), followed by bipolar disorder (10.26; 95% CI, 7.97–13.00) and substancerelated disorder (6.78; 95% CI, 4.14–10.47). In survival analysis, psychotic disorder had the highest HR (4.16; 95% CI, 2.86–6.05), which was further increased with younger age, male sex, and comorbidity of personality disorder.
Conclusion
All psychiatric patients are at a higher risk of suicide compared to the general population, and the risk is highest for those diagnosed with psychotic disorder.
Keyword
Figure
Cited by 1 articles
-
Association of the COVID-19 Pandemic and Low-rescue Suicide Attempts in Patients Visiting the Emergency Department after Attempting Suicide
Juneyoung Lee, Daehee Kim, Woon Jeong Lee, Seon Hee Woo, Sikyoung Jeong, Seong Hee Kim
J Korean Med Sci. 2021;36(34):e243. doi: 10.3346/jkms.2021.36.e243.
Reference
-
1. Sadock BJ, Kaplan HI, Sadock VA. Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2003.2. Osborn D, Levy G, Nazareth I, King M. Suicide and severe mental illnesses. Cohort study within the UK general practice research database. Schizophr Res. 2008; 99(1-3):134–138. PMID: 18155881.
Article3. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010; 24(4):Suppl. 81–90. PMID: 20923923.4. Hansson C, Joas E, Pålsson E, Hawton K, Runeson B, Landén M. Risk factors for suicide in bipolar disorder: a cohort study of 12 850 patients. Acta Psychiatr Scand. 2018; 138(5):456–463. PMID: 30076611.
Article5. Plans L, Barrot C, Nieto E, Rios J, Schulze TG, Papiol S, et al. Association between completed suicide and bipolar disorder: a systematic review of the literature. J Affect Disord. 2019; 242:111–122. PMID: 30173059.
Article6. Courtet P. Understanding Suicide: from Diagnosis to Personalized Treatment. Cham: Springer;2016.7. Park SC, Lee SK, Oh HS, Jun TY, Lee MS, Kim JM, et al. Hazardous drinking-related characteristics of depressive disorders in Korea: the CRESCEND study. J Korean Med Sci. 2015; 30(1):74–81. PMID: 25552886.
Article8. Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2018; 34(Suppl):(1):e75.
Article9. Mee S, Bunney BG, Bunney WE, Hetrick W, Potkin SG, Reist C. Assessment of psychological pain in major depressive episodes. J Psychiatr Res. 2011; 45(11):1504–1510. PMID: 21831397.
Article10. Olié E, Guillaume S, Jaussent I, Courtet P, Jollant F. Higher psychological pain during a major depressive episode may be a factor of vulnerability to suicidal ideation and act. J Affect Disord. 2010; 120(1-3):226–230. PMID: 19394086.
Article11. Racine M. Chronic pain and suicide risk: a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2018; 87(Pt B):269–280. PMID: 28847525.
Article12. Central Suicide Prevention Center. The suicide rate in Korea, 2018. Updated 2018. Accessed March 1, 2020. http://spckorea-stat.or.kr.13. Organisation for Economic Co-operation and Development. OECD health statistics 2017. Updated 2019. Accessed March 1, 2020. http://www.oecd.org/els/health-systems/OECD-Health-Statistics-2019-Frequently-Requested-Data.xls.14. Statistics Korea. Mortality trend by cause of death. Updated 2020. Accessed March 1, 2020. http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012.15. Shin Y, Park B, Lee HA, Park B, Han H, Choi EJ, et al. Disease-specific mortality and prevalence trends in Korea, 2002–2015. J Korean Med Sci. 2020; 35(4):e27. PMID: 31997615.
Article16. Kim H, Kim B, Kang SG, Kim MD, Kim MH, Kim SI, et al. Attempted suicides in South Korea: a multi-center analysis of causes, methods, and psychiatric diagnoses of suicidal attempters in 2013. Korean J Biol Psychiatry. 2015; 22(4):187–194.17. Office for Government Policy Coordination, Prime Minister's Secretariat. State coordination office of Republic of Korea. National action plan for suicide prevention. Updated 2020. Accessed February 6, 2020. http://www.opm.go.kr/opm/info/project02.do.18. Park E, Choi SJ. Prevalence of suicidal ideation and related risk factors among Korean adults. J Korean Acad Psychiatr Ment Health Nurs. 2013; 22(2):88–96.
Article19. Korea Suicide Prevention Center. Cause of suicide. Updated 2020. Accessed July 24, 2020. https://spckorea-stat.or.kr/korea02.do.20. Lee JS, Choi JW, Park SB, Yoo HI, Hong JP. Preliminary study on the clinical characteristics between suicide attempters and suicide completers who had visited emergency room. J Korean Neuropsychiatr Assoc. 2010; 49(2):185–192.21. World Health Organization. ICD-10 online versions. Updated 2018. Accessed February 5, 2018. https://www.who.int/classifications/icd/icdonlineversions/en/.22. Barak-Corren Y, Castro VM, Javitt S, Hoffnagle AG, Dai Y, Perlis RH, et al. Predicting suicidal behavior from longitudinal electronic health records. Am J Psychiatry. 2017; 174(2):154–162. PMID: 27609239.
Article23. Räsänen S, Hakko H, Viilo K, Meyer-Rochow VB, Moring J. Excess mortality among long-stay psychiatric patients in Northern Finland. Soc Psychiatry Psychiatr Epidemiol. 2003; 38(6):297–304. PMID: 12799779.
Article24. Korea National Statistical Office. Suicide data. Updated 2019. Accessed February 5, 2019. http://kostat.go.kr/portal/korea/index.action.25. Dome P, Rihmer Z, Gonda X. Suicide risk in bipolar disorder: a brief review. Medicina (Kaunas). 2019; 55(8):E403. PMID: 31344941.
Article26. Bauer M, Andreassen OA, Geddes JR, Vedel Kessing L, Lewitzka U, Schulze TG, et al. Areas of uncertainties and unmet needs in bipolar disorders: clinical and research perspectives. Lancet Psychiatry. 2018; 5(11):930–939. PMID: 30146246.
Article27. Allgulander C, Allebeck P, Przybeck TR, Rice JP. Risk of suicide by psychiatric diagnosis in Stockholm County. A longitudinal study of 80,970 psychiatric inpatients. Eur Arch Psychiatry Clin Neurosci. 1992; 241(5):323–326. PMID: 1606198.28. Pompili M, Gonda X, Serafini G, Innamorati M, Sher L, Amore M, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013; 15(5):457–490. PMID: 23755739.
Article29. Dutta R, Boydell J, Kennedy N, VAN Os J, Fearon P, Murray RM. Suicide and other causes of mortality in bipolar disorder: a longitudinal study. Psychol Med. 2007; 37(6):839–847. PMID: 17349107.
Article30. Ösby U, Correia N, Brandt L, Ekbom A, Sparén P. Mortality and causes of death in schizophrenia in Stockholm county, Sweden. Schizophr Res. 2000; 45(1-2):21–28. PMID: 10978869.
Article31. Limosin F, Loze JY, Philippe A, Casadebaig F, Rouillon F. Ten-year prospective follow-up study of the mortality by suicide in schizophrenic patients. Schizophr Res. 2007; 94(1-3):23–28. PMID: 17574389.
Article32. Ko YS, Tsai HC, Chi MH, Su CC, Lee IH, Chen PS, et al. Higher mortality and years of potential life lost of suicide in patients with schizophrenia. Psychiatry Res. 2018; 270:531–537. PMID: 30342411.
Article33. Armstrong BG. Comparing standardized mortality ratios. Ann Epidemiol. 1995; 5(1):60–64. PMID: 7728286.
Article34. Park S, Ahn MH, Na R, Kim SO, Yoon JS, Park JH, et al. Factors associated with suicide method among psychiatric patients in a general hospital in Korea. Psychiatry Res. 2013; 210(3):945–950. PMID: 24055162.
Article35. Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013; 3(4):200–218. PMID: 24167693.
Article36. Kasckow J, Felmet K, Zisook S. Managing suicide risk in patients with schizophrenia. CNS Drugs. 2011; 25(2):129–143. PMID: 21254789.
Article37. Erlangsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am J Geriatr Psychiatry. 2008; 16(3):220–228. PMID: 18310552.
Article38. Draper B, Peisah C, Snowdon J, Brodaty H. Early dementia diagnosis and the risk of suicide and euthanasia. Alzheimers Dement. 2010; 6(1):75–82. PMID: 20129322.
Article39. Bernert RA, Joiner TE. Sleep disturbances and suicide risk: a review of the literature. Neuropsychiatr Dis Treat. 2007; 3(6):735–743. PMID: 19300608.
Article40. Cougle JR, Keough ME, Riccardi CJ, Sachs-Ericsson N. Anxiety disorders and suicidality in the national comorbidity survey-replication. J Psychiatr Res. 2009; 43(9):825–829. PMID: 19147159.
Article41. Couto T, Neves F, Machado MCL, Vasconcelos AG, Correa H, Malloy-Diniz LF. Assessment of impulsivity in bipolar disorder (BD) in comorbidity with generalized anxiety disorder (GAD): revisiting the hypothesis of protective effect. Clin Neuropsychiatry. 2012; 9(2):102–106.42. Fishbain DA, Lewis JE, Gao J. The pain suicidality association: a narrative review. Pain Med. 2014; 15(11):1835–1849. PMID: 24995953.
Article43. Caldwell CB, Gottesman II. Schizophrenia--a high-risk factor for suicide: clues to risk reduction. Suicide Life Threat Behav. 1992; 22(4):479–493. PMID: 1488792.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review on the Components and Improvements of Gatekeeper Training: Focusing on Family Intervention of People With Mental Illness
- The Characteristics of Suicide Attempts and Psychosocial Risk Factors in Correctional Institutions
- Awareness and Attitude Toward Suicide in Community Mental Health Professionals and Hospital Workers
- The Causes of Death of the Institutionalized Population of Kkottongnae: Comparison between Severe Mental Illness Group(SMI) and Non-Severe Mental Illness Group(Non-SMI)
- Suicide Method, the Recent Stressors, Psychiatric Diagnosis of Suicide Attempters and Suicide Completers