Int J Thyroidol.
2020 Nov;13(2):155-164. 10.11106/ijt.2020.13.2.155.
Urinary Iodine Concentration and Thyroid Peroxidase Antibodies in the Korean Population Using Korea National Health and Nutrition Examination Survey VI
- Affiliations
-
- 1Department of Surgery, Dankook University College of Medicine, Cheonan, Korea
- KMID: 2509198
- DOI: http://doi.org/10.11106/ijt.2020.13.2.155
Abstract
- Background and Objectives
This study was planned to investigate the relationship between iodine intake and thyroid peroxidase antibody in Korean population.
Materials and Methods
We used the data of the 6th Korea National Health and Nutrition Examination Survey from 2013 to 2015. A total of 6564 subjects who had the data of thyroid function test were included. We analyzed urinary iodine concentration and thyroid peroxidase antibody using the complex sample method. Univariate and multivariate analysis were performed according to clinical factors and thyroid function tests.
Results
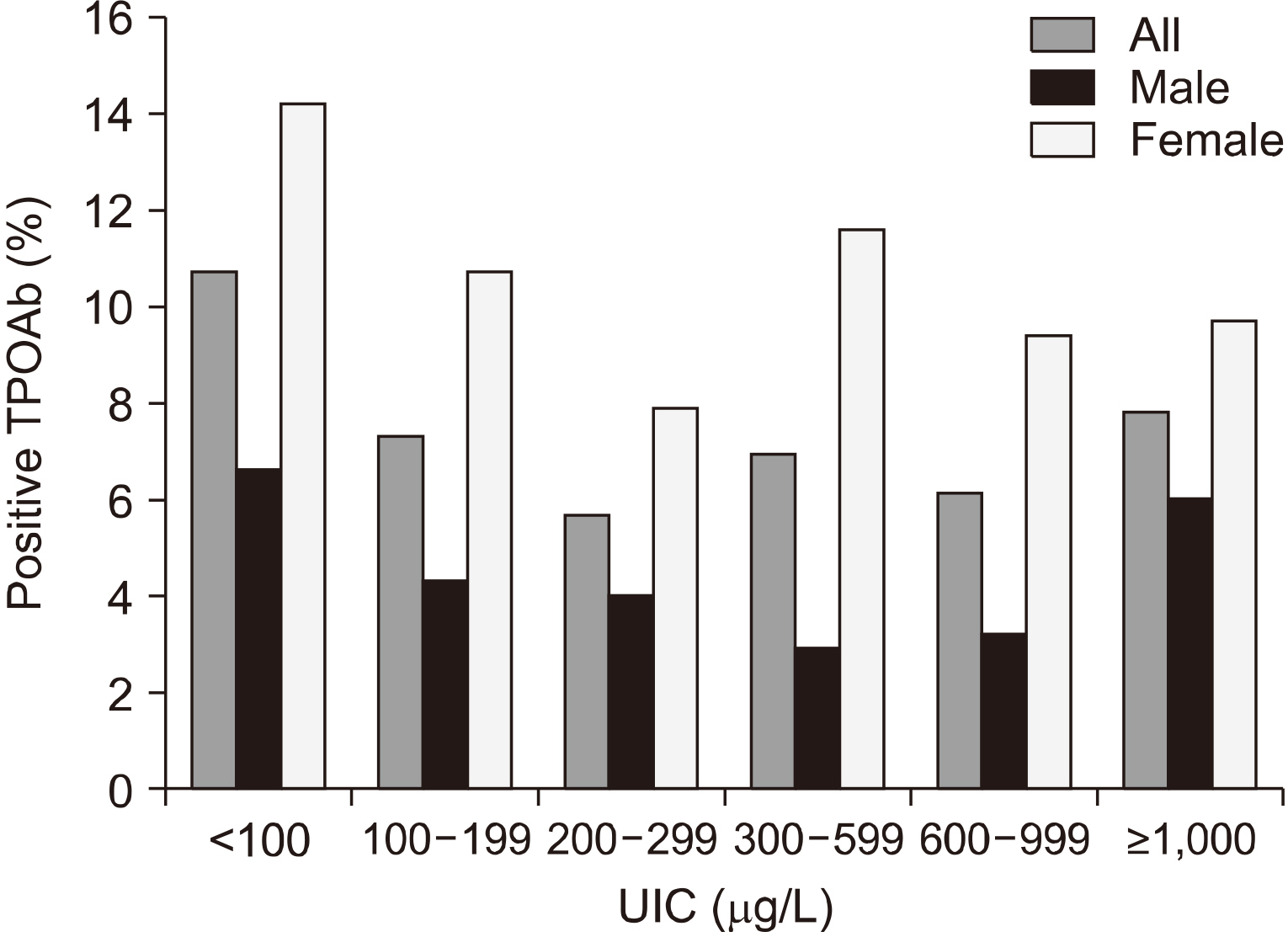
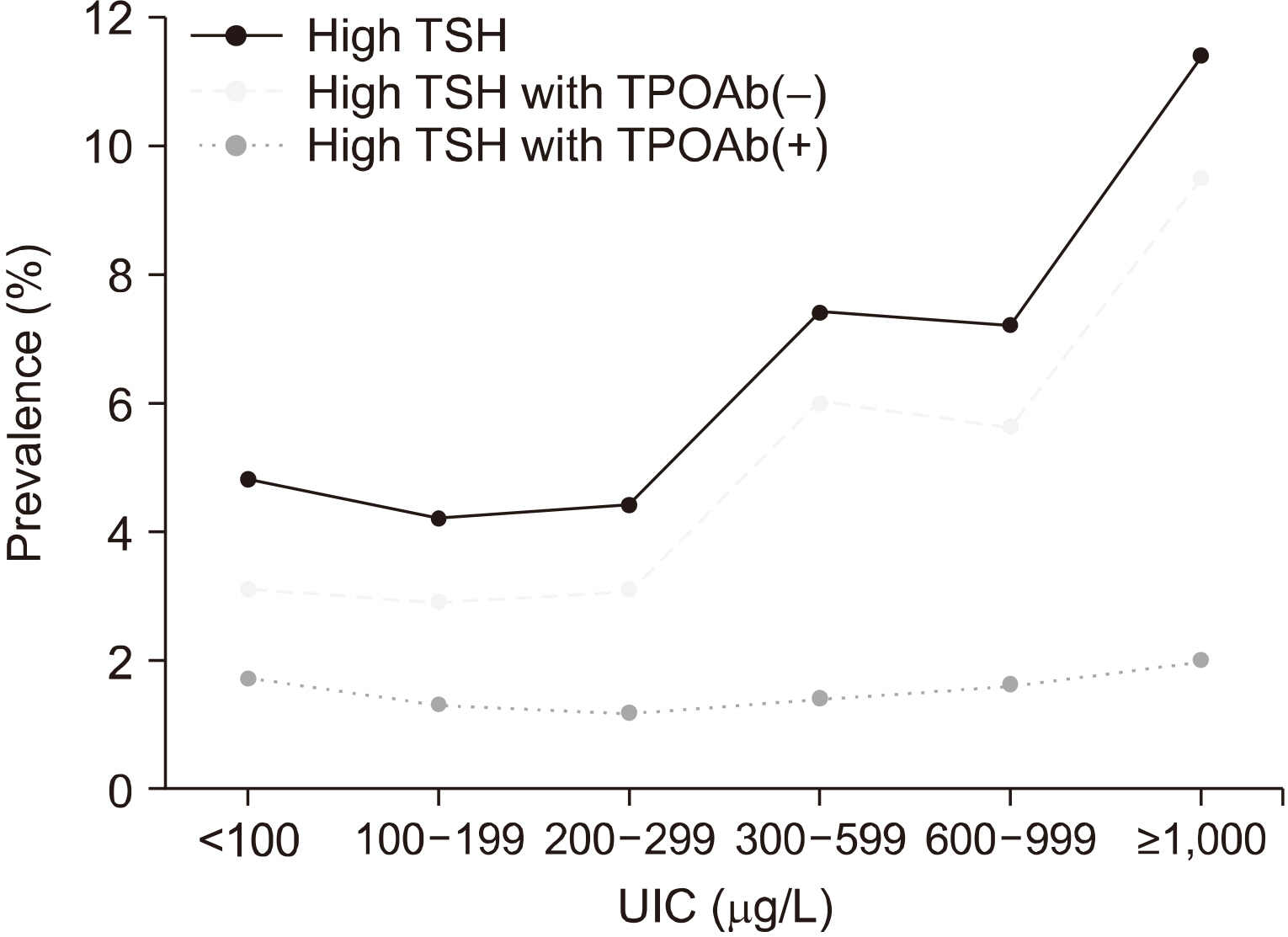
In the multivariate analysis, the thyroid peroxidase antibody positivity was not related to urinary iodine concentration in the total group (p=0.102), male group (p=0.245) and female group (p=0.098). The urinary iodine concentration was associated with thyroid stimulating hormone (TSH) (p=0.001) and free T4 (p=0.001) but not associated with thyroid peroxidase antibody (p=0.218). When high TSH group was divided into the positive and negative thyroid peroxidase antibody, high TSH group with negative thyroid peroxidase antibody increased according to increasing urinary iodine concentration (p<0.001). But there was no difference in the high TSH group with positive thyroid peroxidase antibody (p=0.826).
Conclusion
This study did not show a statistically significant relationship between urinary iodine concentration and thyroid peroxidase antibody. As urinary iodine concentration increased, thyroid function was decreased only in the negative thyroid peroxidase antibody group. This confirmed that the increased urinary iodine concentration caused hypothyroidism which was not associated with thyroid peroxidase antibody.
Figure
Reference
-
References
1. Iodine Global Network. 2020. Global scorecard of iodine nutrition in 2020. Iodine Global Network;Seattle: Available from URL: https://www.ign.org/cm_data/Global-Scorecard-2020-3-June-2020.pdf. cited September 4, 2020.2. Farebrother J, Zimmermann MB, Andersson M. 2019; Excess iodine intake: sources, assessment, and effects on thyroid function. Ann N Y Acad Sci. 1446(1):44–65. DOI: 10.1111/nyas.14041. PMID: 30891786.
Article3. Dong YH, Fu DG. 2014; Autoimmune thyroid disease: mechanism, genetics and current knowledge. Eur Rev Med Pharmacol Sci. 18(23):3611–8. PMID: 25535130.4. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. 2014; Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 43(1):69–77. DOI: 10.1093/ije/dyt228. PMID: 24585853. PMCID: PMC3937975.
Article5. Kim WG, Kim WB, Woo G, Kim H, Cho Y, Kim TY, et al. 2017; Thyroid stimulating hormone reference range and prevalence of thyroid dysfunction in the Korean population: Korea National Health and Nutrition Examination Survey 2013 to 2015. Endocrinol Metab (Seoul). 32(1):106–14. DOI: 10.3803/EnM.2017.32.1.106. PMID: 28116874. PMCID: PMC5368108.
Article6. WHO. Urinary iodine concentrations for determining iodine status deficiency in populations. Vitamin and Mineral Nutrition Information System. World Health Organization;Geneva: Available from URL: http://www.who.int/vmnis/indicators/urinaryiodine. cited September 4, 2020.7. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. 2002; Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 87(2):489–99. DOI: 10.1210/jcem.87.2.8182. PMID: 11836274.
Article8. Amouzegar A, Bakhtiyari M, Mansournia MA, Etemadi A, Mehran L, Tohidi M, et al. 2016; Sex- and age-specific reference values and cutoff points for TPOAb: Tehran Thyroid Study. Thyroid. 26(3):458–65. DOI: 10.1089/thy.2015.0276. PMID: 26650261.
Article9. Teng D, Yang W, Shi X, Li Y, Ba J, Chen B, et al. 2020; An inverse relationship between iodine intake and thyroid antibodies: a national cross-sectional survey in Mainland China. Thyroid. 30(11):1656–65. DOI: 10.1089/thy.2020.0037. PMID: 32586221.
Article10. Li Y, Teng D, Ba J, Chen B, Du J, He L, et al. 2020; Efficacy and safety of long-term universal salt iodization on thyroid disorders: epidemiological evidence from 31 provinces of Mainland China. Thyroid. 30(4):568–79. DOI: 10.1089/thy.2019.0067. PMID: 32075540.
Article11. Kasagi K, Takahashi N, Inoue G, Honda T, Kawachi Y, Izumi Y. 2009; Thyroid function in Japanese adults as assessed by a general health checkup system in relation with thyroid-related antibodies and other clinical parameters. Thyroid. 19(9):937–44. DOI: 10.1089/thy.2009.0205. PMID: 19678737.
Article12. Pedersen IB, Knudsen N, Carle A, Vejbjerg P, Jorgensen T, Perrild H, et al. 2011; A cautious iodization programme bringing iodine intake to a low recommended level is associated with an increase in the prevalence of thyroid autoantibodies in the population. Clin Endocrinol (Oxf). 75(1):120–6. DOI: 10.1111/j.1365-2265.2011.04008.x. PMID: 21521277.
Article13. Aghini Lombardi F, Fiore E, Tonacchera M, Antonangeli L, Rago T, Frigeri M, et al. 2013; The effect of voluntary iodine prophylaxis in a small rural community: the Pescopagano survey 15 years later. J Clin Endocrinol Metab. 98(3):1031–9. DOI: 10.1210/jc.2012-2960. PMID: 23436921.
Article14. Zaletel K, Gaberscek S, Pirnat E. 2011; Ten-year follow-up of thyroid epidemiology in Slovenia after increase in salt iodization. Croat Med J. 52(5):615–21. DOI: 10.3325/cmj.2011.52.615. PMID: 21990079. PMCID: PMC3195970.
Article15. Golkowski F, Buziak-Bereza M, Trofimiuk M, Baldys-Waligorska A, Szybinski Z, Huszno B. 2007; Increased prevalence of hyperthyroidism as an early and transient side-effect of im-plementing iodine prophylaxis. Public Health Nutr. 10(8):799–802. DOI: 10.1017/S1368980007585939. PMID: 17381939.16. Fountoulakis S, Philippou G, Tsatsoulis A. 2007; The role of iodine in the evolution of thyroid disease in Greece: from endemic goiter to thyroid autoimmunity. Hormones (Athens). 6(1):25–35. PMID: 17324915.17. Hong A, Stokes B, Otahal P, Owens D, Burgess JR. 2017; Temporal trends in thyroid-stimulating hormone (TSH) and thyroid peroxidase antibody (ATPO) testing across two phases of iodine fortification in Tasmania (1995-2013). Clin Endocrinol (Oxf). 87(4):386–93. DOI: 10.1111/cen.13371. PMID: 28500624.
Article18. Li Y, Teng D, Shan Z, Teng X, Guan H, Yu X, et al. 2008; Antithyroperoxidase and antithyroglobulin antibodies in a five-year follow-up survey of populations with different iodine intakes. J Clin Endocrinol Metab. 93(5):1751–7. DOI: 10.1210/jc.2007-2368. PMID: 18270254.
Article19. Shan Z, Chen L, Lian X, Liu C, Shi B, Shi L, et al. 2016; Iodine status and prevalence of thyroid disorders after introduction of mandatory universal salt iodization for 16 years in China: a cross-sectional study in 10 cities. Thyroid. 26(8):1125–30. DOI: 10.1089/thy.2015.0613. PMID: 27370068.
Article20. Nagata K, Takasu N, Akamine H, Ohshiro C, Komiya I, Murakami K, et al. 1998; Urinary iodine and thyroid antibodies in Okinawa, Yamagata, Hyogo, and Nagano, Japan: the differences in iodine intake do not affect thyroid antibody positivity. Endocr J. 45(6):797–803. DOI: 10.1507/endocrj.45.797. PMID: 10395237.
Article21. Teng X, Shan Z, Chen Y, Lai Y, Yu J, Shan L, et al. 2011; More than adequate iodine intake may increase subclinical hypothyroidism and autoimmune thyroiditis: a cross-sectional study based on two Chinese communities with different iodine intake levels. Eur J Endocrinol. 164(6):943–50. DOI: 10.1530/EJE-10-1041. PMID: 21444648.
Article22. Wan S, Qu M, Wu H, Ren B, Jiang W, Wang X, et al. 2020; Autoimmune thyroid diseases after 25 years of universal salt iodisation: an epidemiological study of Chinese adults in areas with different water iodine levels. Br J Nutr. 124(8):853–64. DOI: 10.1017/S0007114520001786. PMID: 32436480.
Article23. Kim HI, Oh HK, Park SY, Jang HW, Shin MH, Kim SW, et al. 2019; Urinary iodine concentration and thyroid hormones: Korea National Health and Nutrition Examination Survey 2013-2015. Eur J Nutr. 58(1):233–40. DOI: 10.1007/s00394-017-1587-8. PMID: 29188371.
Article24. Jeon MJ, Kim WG, Kwon H, Kim M, Park S, Oh HS, et al. 2017; Excessive iodine intake and thyrotropin reference interval: data from the Korean National Health and Nutrition Examination Survey. Thyroid. 27(7):967–72. DOI: 10.1089/thy.2017.0078. PMID: 28471294.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Thyroid Hormone Levels and Urinary Iodine Concentrations in Koreans Based on the Data from Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
- Update on Thyroid Hormone Levels and Thyroid Dysfunction in the Korean Population Based on Data from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
- A study to evaluate the safety of iodine intake levels in women of childbearing age: 2013–2015 Korea National Health and Nutrition Examination Survey
- Iodine status and characteristics of Korean adolescents and their parents based on urinary iodine concentration: a nationwide cross-sectional study
- Evaluation of Iodine Status among Korean Patients with Papillary Thyroid Cancer Using Dietary and Urinary Iodine