J Rhinol.
2020 Nov;27(2):145-149. 10.18787/jr.2020.00329.
A Case of Endoscopic Drainage of Pterygoid Fossa Abscess Induced by Fungal Invasion
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, School of Medicine, Kosin Gospel University, Busan, Korea
- KMID: 2508962
- DOI: http://doi.org/10.18787/jr.2020.00329
Abstract
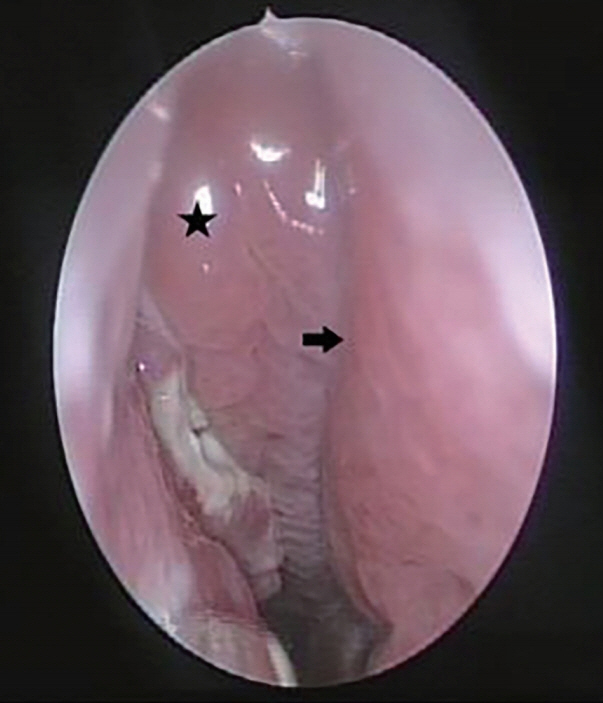
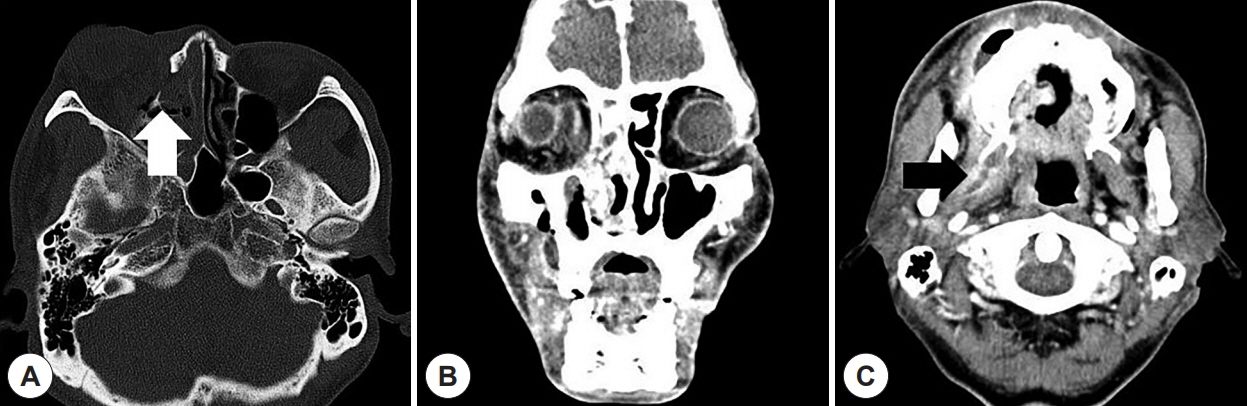
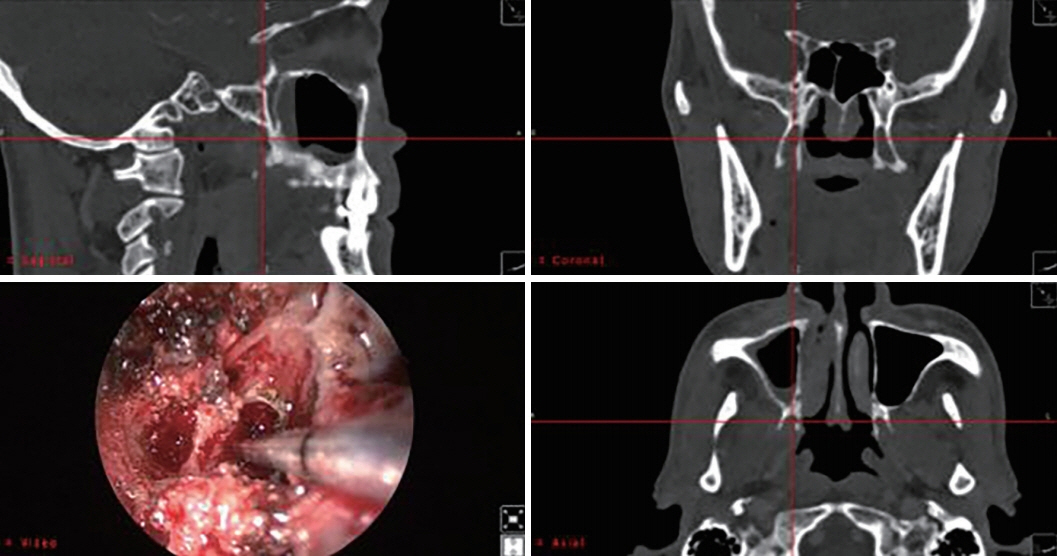
- The infratemporal fossa consists of critical structures affecting patient quality of life. Though abscess formation in the infratemporal fossa is very rare, drainage is highly recommended to avoid severe complications. We recently experienced a rare case of infratemporal fossa abscess. Such an abscess is easy to misdiagnose due to its rarity. Endoscopic drainage of the infratemporal fossa was conducted in this case, and its limited invasiveness was an advantage for a conservative approach. We present this case with a brief review of the approach to abscess of the infratemporal fossa area.
Keyword
Figure
Reference
-
References
1. Schwimmer AM, Roth SE, Morrison SN. The use of computerized tomography in the diagnosis and management of temporal and infratemporal space abscesses. Oral Surgery, Oral Medicine, Oral Pathology. 1988; 66(1):17–20.2. Chang Y, Chen P, Hung J, Chen H, Lai C, Ou C, et al. Orbital complications of paranasal sinusitis in taiwan, 1988 through 2015: acute ophthalmological manifestations, diagnosis, and management. PloS One. 2017; 12(10):e0184477.3. Singh V. Fungal rhinosinusitis: Unravelling the disease spectrum. Journal of Maxillofacial and Oral Surgery. 2019; 18(2):164–79.4. Kasahara K, Ogawa C, Matsuzaka K, Yamamura T, Takano M, Saitou C, et al. A case of infratemporal fossa abscess with signs of chronic maxillary osteomyelitis. Bull Tokyo Dent Coll. 2015; 56(2):121–9.5. Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina W, Kita H, et al. Fungal rhinosinusitis: a categorization and definitional schema addressing current controversies. Laryngoscope. 2009; 119(9):1809–18.6. Weiss BR. Infratemporal fossa abscess unusual complication of maxillary sinus fracture. Laryngoscope. 1977; 87(7):1130–3.7. Raghava N, Evans K, Basu S. Infratemporal fossa abscess: complication of maxillary sinusitis. The Journal of Laryngology & Otology. 2004; 118(5):377–8.8. Park M, Kim H, Ko H, Kim M, Kim B. Infratemporal fossa abscess of dental origin: a rare, severe and misdiagnosed infection. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2018; 44(1):37–9.9. Arya S, Rane P, D’Cruz A, Hathiram B, Khattar V. Infratemporal fossa, masticator space and parapharyngeal space: Can the radiologist and surgeon speak the same language. Int J Otorhinolaryngol Clin. 2012; 4(3):125–35.10. Ramdas S. An unusual foreign body in the infratemporal fossa. Indian J Plast Surg. 2016; 49(2):275–8.11. Barbosa JF. Surgery of extensive cancer of paranasal sinuses: presentation of a new technique. Archives of Otolaryngology. 1961; 73(2):129–38.12. Sekhar LN, Schramm VL, Jones NF. Subtemporal-preauricular infratemporal fossa approach to large lateral and posterior cranial base neoplasms. J Neurosurg. 1987; 67(4):488–99.13. Arriaga MA, Janecka IP. Facial translocation approach to the cranial base: the anatomic basis. Skull Base Surg. 1991; 1(1):26–33.14. Plzák J, Kratochvil V, Kešner A, Šurda P, Vlasák A, Zvěřina E. Endoscopic endonasal approach for mass resection of the pterygopalatine fossa. Clinics. 2017; 72(9):554–61.15. Nomura K, Hidaka H, Takata Y, Katori Y. Minimally invasive transnasal approach to infratemporal fossa abscess. J Laryngol Otol. 2015; 129(8):812.16. Sundaram SS, Rajan P, Balasubramanian A. Endoscopic transmaxillary drainage of an infratemporal fossa abscess. BMJ Case Rep. 2014; 2014:bcr2013200637.17. DelGaudio JM. Endoscopic transnasal approach to the pterygopalatine fossa. Archives of Otolaryngology–Head & Neck Surgery. 2003; 129(4):441–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Surgery for Intraorbital Abscess: A Report of One Case
- A Case of an Orbital Abscess Managed by Endonasal Endoscopic Surgery
- Endoscopic Treatment of Extensive Deep Abscess in Distal Posterior Thigh: A Case Report
- Esophageal Stricture after Endoscopic Drainage of Esophageal Abscess as a Complication of Acute Phlegmonous Esophagitis: A Case Report
- A Case of Infratemporal Fossa Abscess Caused by Acute Sinusitis