Arch Hand Microsurg.
2020 Dec;25(4):297-303. 10.12790/ahm.20.0057.
Analysis of Outcomes of Tamai Zone I Digital Replantation in Cases of Severe Crushing Injury
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- KMID: 2508944
- DOI: http://doi.org/10.12790/ahm.20.0057
Abstract
- Purpose
Digital replantation has dramatically changed the fate of mutilated injuries of hand. But in case of severe crushing injury in Tamai zone I, it is a contraindication of replantation. This study aims to determine the replantation survival rate in cases with crushing injury.
Methods
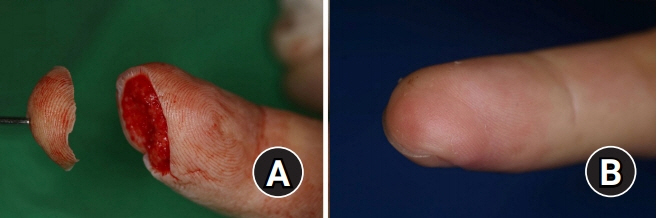
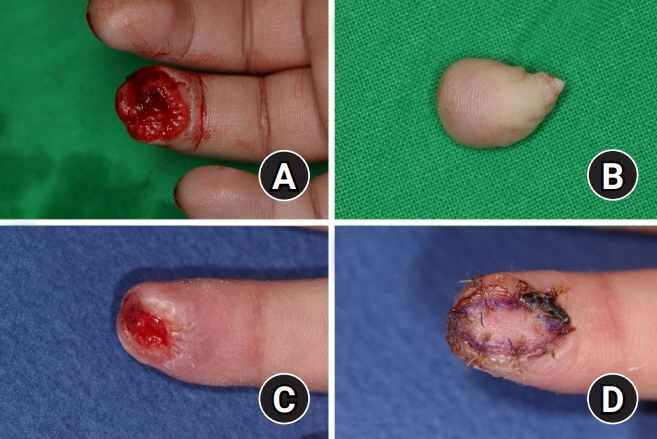
We retrospectively evaluated patients’ charts and photos from January 2015 to December 2019. There were 294 patients (331 fingers) with digital amputation who underwent surgery. Cases with crushing were divided into petechiae-in-skin group and red-line-sign group and compared with the group without crushing. The relationship of survival rate with factors was evaluated using chi-square analysis.
Results
Of these, 199 fingers were defined as severe crushed, and 140 cases with petechiae in skin and 59 cases with red line sign. There was no statistically significant difference in survival rate compared with the group without crushing (p=0.227). Additional surgery was performed more in crushed injury. However, necrotized soft tissue was mainly on margin of amputation, not on crushed area.
Conclusion
The presence of crushing did not affect survival rate in Tamai zone I replantation. However, as the degree of crushing was severe, the need for additional surgery increased. We found that the number of anastomosed arteries and veins influences the survival rate. According to our analysis, even if it’s difficult, finding and doing anastomosis as many vessels as possible can make good results.
Keyword
Figure
Reference
-
1. Sebastin SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011; 128:723–37.
Article2. Hattori Y, Doi K, Ikeda K, Estrella EP. A retrospective study of functional outcomes after successful replantation versus amputation closure for single fingertip amputations. J Hand Surg Am. 2006; 31:811–8.
Article3. Wang K, Sears ED, Shauver MJ, Chung KC. A systematic review of outcomes of revision amputation treatment for fingertip amputations. Hand (N Y). 2013; 8:139–45.
Article4. Neligan PC. Plastic surgery. 4th ed (Vol. 6). London: Elsevier;2018. p. 249–50.5. Kadota H, Imaizumi A, Ishida K, Sashida Y. Successful local use of heparin calcium for congested fingertip replants. Arch Plast Surg. 2020; 47:54–61.
Article6. Matsuda M, Chikamatsu E, Shimizu Y. Correlation between number of anastomosed vessels and survival rate in finger replantation. J Reconstr Microsurg. 1993; 9:1–4.
Article7. Ryu DH, Roh SY, Kim JS, Lee DC, Lee KJ. Multiple venous anastomoses decrease the need for intensive postoperative management in tamai zone I replantations. Arch Plast Surg. 2018; 45:58–61.
Article8. Tamai S. Twenty years’ experience of limb replantation: review of 293 upper extremity replants. J Hand Surg Am. 1982; 7:549–56.9. Lee DC, Kim JS, Ki SH, Roh SY, Yang JW, Chung KC. Partial second toe pulp free flap for fingertip reconstruction. Plast Reconstr Surg. 2008; 121:899–907.
Article10. Kim JS, Yang JW, Lee DC, Ki SH, Roh SY. Challenges in fingertip replantation. Semin Plast Surg. 2013; 27:165–73.11. Zhong-Wei C, Meyer VE, Kleinert HE, Beasley RW. Present indications and contraindications for replantation as reflected by long-term functional results. Orthop Clin North Am. 1981; 12:849–70.
Article12. He JY, Chen SH, Tsai TM. The risk factors for failure of an upper extremity replantation: is the use of cigarettes/tobacco a significant factor? PLoS One. 2015; 10:e0141451.
Article13. Nishijima A, Yamamoto N, Yanagibayashi S, et al. The effect of smoking on necrosis rate in digital replantation and revascularization with prostaglandin E1 therapy: a retrospective study. Plast Reconstr Surg. 2016; 138:848–53.14. van Adrichem LN, Hovius SE, van Strik R, van der Meulen JC. The acute effect of cigarette smoking on the microcirculation of a replanted digit. J Hand Surg Am. 1992; 17:230–4.
Article15. Efanov JI, Rizis D, Landes G, Bou-Merhi J, Harris PG, Danino MA. Impact of the number of veins repaired in short-term digital replantation survival rate. J Plast Reconstr Aesthet Surg. 2016; 69:640–5.
Article16. Huang HF, Yeong EK. Surgical treatment of distal digit amputation: success in distal digit replantation is not dependent on venous anastomosis. Plast Reconstr Surg. 2015; 135:174–8.17. Maricevich M, Carlsen B, Mardini S, Moran S. Upper extremity and digital replantation. Hand (N Y). 2011; 6:356–63.
Article18. Lin CH, Aydyn N, Lin YT, Hsu CT, Lin CH, Yeh JT. Hand and finger replantation after protracted ischemia (more than 24 hours). Ann Plast Surg. 2010; 64:286–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Evaluation of Microreplantation in the Digital Amputation
- A Clinical Study of Replantation of Amputated Upper Limbs and Digits
- A Clinical Study of Replantation of Amputated Digits
- Multiple venous anastomoses decrease the need for intensive postoperative management in tamai zone I replantations
- Predictors of Survival Rate in Fingertip Replantation