J Korean Med Sci.
2020 Nov;35(44):e387. 10.3346/jkms.2020.35.e387.
A Systematic Narrative Review of Comprehensive Preparedness Strategies of Healthcare Resources for a Large Resurgence of COVID-19 Nationally, with Local or Regional Epidemics: Present Era and Beyond
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 2Division of Infectious Diseases, Department of Internal Medicine, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 3Division of Infectious Disease, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Infectious Diseases, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2508767
- DOI: http://doi.org/10.3346/jkms.2020.35.e387
Abstract
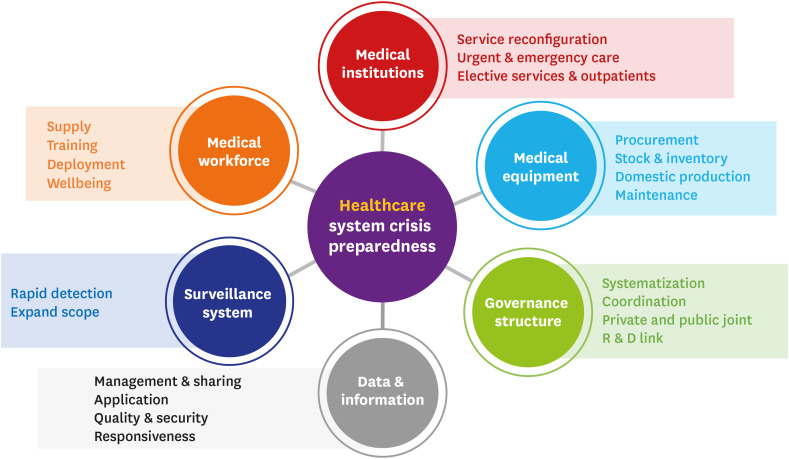
- Coronavirus disease 2019 (COVID-19) has penetrated our daily lives, leading us to a new normal era. The unexpected impact of COVID-19 has posed a unique challenge for the health care system, bringing innovation around the world. Considering the current pandemic pattern, comprehensive preparedness strategies of healthcare resources need to be implemented to prepare for a large resurgence of COVID-19 within a short time. With the unprecedented spread of the new pandemic and the impending influenza season, scientific evidence-based schemes need to be developed through cooperation, coordination, and solidarity. Based on the early experience with the current pandemic, this narrative interpretive review of qualitative studies suggests a 6-domain plan to establish a better health care system that is prepared to deal with the current and future public health crises. The 6 domains are medical institutions, medical workforce, medical equipment, COVID-19 surveillance, data and information application, and governance structure.
Keyword
Figure
Cited by 2 articles
-
Emotional Distress of the COVID-19 Cluster Infection on Health Care Workers Working at a National Hospital in Korea
Og-Jin Jang, Young-In Chung, Jae-Woon Lee, Ho-Chan Kim, Jeong Seok Seo
J Korean Med Sci. 2021;36(47):e324. doi: 10.3346/jkms.2021.36.e324.Impact of COVID-19 Pandemic on Biomedical Publications and Their Citation Frequency
Sooyoung Park, Hyun Jeong Lim, Jaero Park, Yeon Hyeon Choe
J Korean Med Sci. 2022;37(40):e296. doi: 10.3346/jkms.2022.37.e296.
Reference
-
1. Armocida B, Formenti B, Ussai S, Palestra F, Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. 2020; 5(5):e253. PMID: 32220653.
Article2. Lemos DR, D'Angelo SM, Farias LA, Almeida MM, Gomes RG, Pinto GP, et al. Health system collapse 45 days after the detection of COVID-19 in Ceará, Northeast Brazil: a preliminary analysis. Rev Soc Bras Med Trop. 2020; 53:e20200354. PMID: 32638888.
Article3. Liang WH, Guan WJ, Li CC, Li YM, Liang HR, Zhao Y, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicentre) and outside Hubei (non-epicentre): a nationwide analysis of China. Eur Respir J. 2020; 55(6):2000562. PMID: 32269086.
Article4. Coddington DC, Moore KD, Fischer EA. Integrated Health Care: Reorganizing the Physician, Hospital and Health Plan Relationship. Englewood, CO: Center for Research in Ambulatory Health Care Administration (US);1994.5. Dev N, Kumar V, Sankar J. COVID-19 infection outbreak among health care workers: perspective from a low-middle income country. Monaldi Arch Chest Dis. 2020; 90(3):
Article6. Chung HS, Lee DE, Kim JK, Yeo IH, Kim C, Park J, et al. Revised triage and surveillance protocols for temporary emergency department closures in tertiary hospitals as a response to COVID-19 crisis in Daegu Metropolitan City. J Korean Med Sci. 2020; 35(19):e189. PMID: 32419401.
Article7. Saunders-Hastings PR, Krewski D. Reviewing the history of pandemic influenza: understanding patterns of emergence and transmission. Pathogens. 2016; 5(4):66.
Article8. Morens DM, Taubenberger JK, Harvey HA, Memoli MJ. The 1918 influenza pandemic: lessons for 2009 and the future. Crit Care Med. 2010; 38(4):Suppl. e10–e20. PMID: 20048675.
Article9. Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005; 10(Suppl 1):6–20. PMID: 16053580.10. Jones K. Mission drift in qualitative research, or moving toward a systematic review of qualitative studies, moving back to a more systematic narrative review. Qual Rep. 2004; 9(1):94–111.
Article11. Van Nguyen H, Van Hoang M, Dao AT, Nguyen HL, Van Nguyen T, Nguyen PT, et al. An adaptive model of health system organization and responses helped Vietnam to successfully halt the COVID-19 pandemic: What lessons can be learned from a resource-constrained country. Int J Health Plann Manage. 2020; 35(5):988–992. PMID: 32557815.12. Lee CC, Thampi S, Lewin B, Lim TJ, Rippin B, Wong WH, et al. Battling COVID-19: critical care and peri-operative healthcare resource management strategies in a tertiary academic medical centre in Singapore. Anaesthesia. 2020; 75(7):861–871. PMID: 32267963.
Article13. Archbald-Pannone LR, Harris DA, Albero K, Steele RL, Pannone AF, Mutter JB. COVID-19 collaborative model for an academic hospital and long-term care facilities. J Am Med Dir Assoc. 2020; 21(7):939–942. PMID: 32563752.
Article14. Unroe KT, Vest J. Time to leverage health system collaborations: Supporting nursing facilities through the COVID-19 pandemic. J Am Geriatr Soc. 2020; 68(6):1129–1130. PMID: 32392623.15. Kim T. Improving preparedness for and response to coronavirus disease 19 (COVID-19) in long-term care hospitals in Korea. Infect Chemother. 2020; 52(2):133–141. PMID: 32406211.
Article16. Fang D, Pan S, Li Z, Yuan T, Jiang B, Gan D, et al. Large-scale public venues as medical emergency sites in disasters: lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Glob Health. 2020; 5(6):e002815.
Article17. Noh JY, Song JY, Yoon JG, Seong H, Cheong HJ, Kim WJ. Safe hospital preparedness in the era of COVID-19: the Swiss cheese model. Int J Infect Dis. 2020; 98:294–296. PMID: 32619759.
Article18. Daumas RP, Silva GA, Tasca R, Leite ID, Brasil P, Greco DB, et al. The role of primary care in the Brazilian healthcare system: limits and possibilities for fighting COVID-19. Cad Saude Publica. 2020; 36(6):e00104120. PMID: 32609166.19. Kim H, Kim D, Paul C, Lee CK. The spatial allocation of hospitals with negative pressure isolation rooms in Korea: Are we prepared for new outbreaks? Int J Health Policy Manag. Forthcoming. 2020; DOI: 10.34172/ijhpm.2020.118.
Article20. Kim T, Choi MJ, Kim SB, Kim JY, Lee J, Oh HS, et al. Strategical preparedness and response actions in the healthcare system against coronavirus disease 2019 according to transmission scenario in Korea. Infect Chemother. 2020; 52(3):389–395. PMID: 32757499.
Article21. Cancedda C, Davis SM, Dierberg KL, Lascher J, Kelly JD, Barrie MB, et al. Strengthening health systems while responding to a health crisis: Lessons learned by a nongovernmental organization during the Ebola virus disease epidemic in Sierra Leone. J Infect Dis. 2016; 214(suppl 3):S153–S163. PMID: 27688219.
Article22. Choi S. A hidden key to COVID-19 management in Korea: public health doctors. J Prev Med Public Health. 2020; 53(3):175–177. PMID: 32498141.
Article23. Liu Y, Wang H, Chen J, Zhang X, Yue X, Ke J, et al. Emergency management of nursing human resources and supplies to respond to coronavirus disease 2019 epidemic. Int J Nurs Sci. 2020; 7(2):135–138. PMID: 32292632.
Article24. Keeley C, Jimenez J, Jackson H, Boudourakis L, Salway RJ, Cineas N, et al. Staffing up for the surge: expanding the New York City public hospital workforce during the COVID-19 pandemic. Health Aff (Millwood). 2020; 39(8):1426–1430. PMID: 32525704.
Article25. Huh K, Shin HS, Peck KR. Emergent strategies for the next phase of COVID-19. Infect Chemother. 2020; 52(1):105–109. PMID: 32100487.
Article26. Bemah P, Baller A, Cooper C, Massaquoi M, Skrip L, Rude JM, et al. Strengthening healthcare workforce capacity during and post Ebola outbreaks in Liberia: an innovative and effective approach to epidemic preparedness and response. Pan Afr Med J. 2019; 33(Suppl 2):9.
Article27. Ramachandran P, Swamy L, Kaul V, Agrawal A. A national strategy for ventilator and ICU resource allocation during the COVID-19 pandemic. Chest. 2020; 158(3):887–889. PMID: 32413343.28. Romney D, Fox H, Carlson S, Bachmann D, O'Mathuna D, Kman N. Allocation of scarce resources in a pandemic: a systematic review of US state crisis standards of care documents. Disaster Med Public Health Prep. 2020; 1–7.
Article29. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020; 382(21):2049–2055. PMID: 32202722.
Article30. Ranney ML, Griffeth V, Jha AK. Critical supply shortages - The need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med. 2020; 382(18):e41. PMID: 32212516.
Article31. Koonin LM, Pillai S, Kahn EB, Moulia D, Patel A. Strategies to inform allocation of stockpiled ventilators to healthcare facilities during a pandemic. Health Secur. 2020; 18(2):69–74. PMID: 32196387.
Article32. Dargaville T, Spann K, Celina M. Opinion to address the personal protective equipment shortage in the global community during the COVID-19 outbreak. Polym Degrad Stabil. 2020; 176:109162.
Article33. Gopichandran V, Subramaniam S.Response to COVID-19: an ethical imperative to build a resilient health system in India. Indian J Med Ethics. 2020; V(2):1–4.
Article34. Desjardins MR, Hohl A, Delmelle EM. Rapid surveillance of COVID-19 in the United States using a prospective space-time scan statistic: detecting and evaluating emerging clusters. Appl Geogr. 2020; 118:102202. PMID: 32287518.
Article35. Balajee SA, Arthur R, Mounts AW. Global health security: building capacities for early event detection, epidemiologic workforce, and laboratory response. Health Secur. 2016; 14(6):424–432. PMID: 27898218.
Article36. Whitelaw S, Mamas MA, Topol E, Van Spall HG. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit Health. 2020; 2(8):e435–40. PMID: 32835201.
Article37. Kim K, Andrew SA, Jung K. Public health network structure and collaboration effectiveness during the 2015 MERS outbreak in South Korea: an institutional collective action framework. Int J Environ Res Public Health. 2017; 14(9):1064.
Article38. Lai AY. Organizational collaborative capacity in fighting pandemic crises: a literature review from the public management perspective. Asia Pac J Public Health. 2012; 24(1):7–20. PMID: 22345395.39. AlKhaldi M, Kaloti R, Shella D, Al Basuoni A, Meghari H. Health system's response to the COVID-19 pandemic in conflict settings: policy reflections from Palestine. Glob Public Health. 2020; 15(8):1244–1256. PMID: 32552389.
Article40. Ning Y, Ren R, Nkengurutse G. China's model to combat the COVID-19 epidemic: a public health emergency governance approach. Glob Health Res Policy. 2020; 5:34. PMID: 32685691.
Article41. Palagyi A, Marais BJ, Abimbola S, Topp SM, McBryde ES, Negin J. Health system preparedness for emerging infectious diseases: a synthesis of the literature. Glob Public Health. 2019; 14(12):1847–1868. PMID: 31084412.
Article42. Carney T, Bennett B. Framing pandemic management: new governance, science or culture? Health Sociol Rev. 2014; 23(2):136–147.
Article43. Lee HY, Oh MN, Park YS, Chu C, Son TJ. Public health crisis preparedness and response in Korea. Osong Public Health Res Perspect. 2013; 4(5):278–284. PMID: 24298444.
Article44. Peck KR. Early diagnosis and rapid isolation: response to COVID-19 outbreak in Korea. Clin Microbiol Infect. 2020; 26(7):805–807. PMID: 32344168.
Article46. Government of Singapore. Looking for PHPC near you? Updated 2020. Accessed October 13, 2020. https://www.flugowhere.gov.sg/.47. Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020; 35(11):e123. PMID: 32193904.
Article48. Kim SI, Lee JY. Walk-through screening center for COVID-19: an accessible and efficient screening system in a pandemic situation. J Korean Med Sci. 2020; 35(15):e154. PMID: 32301300.
Article49. Park PG, Kim CH, Heo Y, Kim TS, Park CW, Kim CH. Out-of-hospital cohort treatment of coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J Korean Med Sci. 2020; 35(13):e140. PMID: 32242347.
Article50. Sheehy LM. Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveill. 2020; 6(2):e19462. PMID: 32369030.
Article51. National Centre for Infectious Diseases (SG). For patients and visitors. Updated 2020. Accessed October 13, 2020. https://www.ncid.sg/Patients-and-Visitors/Visit-a-Specialist/Overview/Pages/default.aspx.52. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13):1239–1242. PMID: 32091533.53. Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020; 105(1):100–101. PMID: 32147406.
Article54. Liu M, Cheng SZ, Xu KW, Yang Y, Zhu QT, Zhang H, et al. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in Wuhan, China: cross sectional study. BMJ. 2020; 369:m2195. PMID: 32522737.
Article55. World Health Organization. WHO surge calculators. Updated 2020. Accessed October 13, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/covid-19-critical-items.56. World Health Organization. List of priority medical devices for COVID-19 case management. Updated 2020. Accessed October 13, 2020. https://www.who.int/publications/m/item/list-of-priority-medical-devices-for-covid-19-case-management.57. Institute of Medicine (US) Forum on Emerging Infections. Davis JR, Lederberg J. 3. Surveillance. Public Health Systems and Emerging Infections: Assessing the Capabilities of the Public and Private Sectors: Workshop Summary. Washington, D.C.: National Academies Press (US);2000.58. Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev. 1988; 10:164–190. PMID: 3066626.
Article59. Nsubuga P, White ME, Thacker SB, Anderson MA, Blount SB, Broome CV, et al. Chapter 53. Public health surveillance: a tool for targeting and monitoring interventions. In : Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, editors. Disease Control Priorities in Developing Countries. 2nd edition. Washington, D.C.: The International Bank for Reconstruction and Development/The World Bank;2006.60. World Health Organization. Public health surveillance for COVID-19: interim guidance. Updated 2020. Accessed October 13, 2020. https://www.who.int/publications/i/item/who-2019-nCoV-surveillanceguidance-2020.7.61. Setel P, AbouZahr C, Atuheire EB, Bratschi M, Cercone E, Chinganya O, et al. Mortality surveillance during the COVID-19 pandemic. Bull World Health Organ. 2020; 98(6):374. PMID: 32514207.
Article62. World Health Organization. Sentinel surveillance. Accessed October 13, 2020. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/sentinel/en/.63. Korean Center for Disease Control and Prevention. Laboratory surveillance for infectious diseases. Updated 2020. Accessed October 13, 2020. http://www.cdc.go.kr/contents.es?mid=a20301090503.64. Choi WS. The national influenza surveillance system of Korea. Infect Chemother. 2019; 51(2):98–106. PMID: 31270989.
Article65. Center for Infectious Disease Research and Policy. COVID-19: the CIDRAP viewpoint. Updated 2020. Accessed October 13, 2020. https://www.cidrap.umn.edu/sites/default/files/public/downloads/cidrap-covid19-viewpoint-part5.pdf.66. Dighe A, Cattarino L, Cuomo-Dannenburg G, Skarp J, Imai N, Bhatia S, et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. 2020; 18(1):321. PMID: 33032601.
Article67. Ali I. COVID-19: Are we ready for the second wave? Disaster Med Public Health Prep. 2020; 1–3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pertussis in the Post-COVID-19 Era: Resurgence, Diagnosis, and Management
- Role of Daegu Medical Association in the infection control of the COVID-19 outbreak
- Responses against infectious disease pandemics: a narrative review on COVID-19 A narrative review
- Burnout among Healthcare Workers during COVID-19 Pandemic
- Cardiovascular Imaging in the Era of the COVID-19 Outbreak