J Korean Med Sci.
2020 Nov;35(44):e364. 10.3346/jkms.2020.35.e364.
Renal Syndromic Hearing Loss Is Common in Childhood-onset Chronic Kidney Disease
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University Medical Center, Seoul, Korea
- 4Department of Biomedical Engineering, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- 6Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea
- 7Kidney Research Institute, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea
- 8Wide River Institute of Immunology, Seoul National University, Seoul, Korea
- KMID: 2508765
- DOI: http://doi.org/10.3346/jkms.2020.35.e364
Abstract
- Background
Hearing loss (HL) in children may adversely affect their development. HL is more prevalent in patients with chronic kidney disease (CKD) than in the general population. This study evaluated the prevalence of HL and its underlying diseases in patients with childhood-onset in CKD.
Methods
In this retrospective study of a tertiary referral center, childhood-onset CKD patients (stage 2–5, age at onset of renal symptom < 18 years) were recruited. We referred to the “renal” syndromic HL as cases with genetic or syndromic diseases, or extra-renal anomalies in addition to HL and CKD.
Results
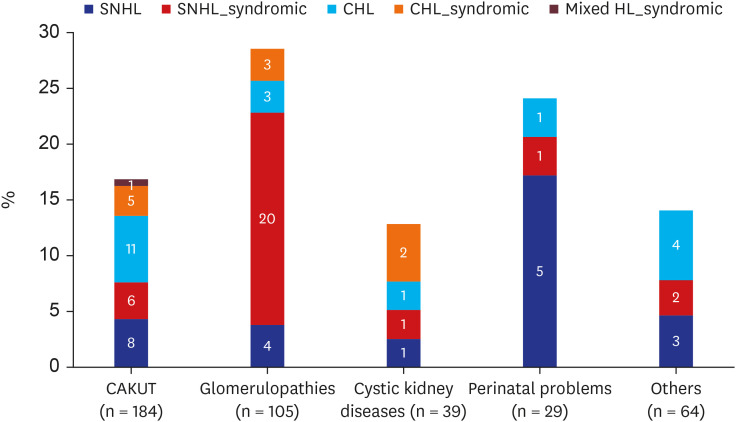
A total of 421 patients (male:female = 279:142) were reviewed according to the causes of CKD: congenital anomalies of the kidney and urinary tract (CAKUT; n = 184, 43.7%), glomerulopathies (GP; n = 105, 24.9%), cystic kidney diseases (CYST; n = 39, 9.3%), perinatal problems (PP; n = 29, 6.9%), and others (n = 64, 15.2%). HL was detected in 82 (19.5%) patients, including 51 (12.1%) patients with sensorineural hearing loss (SNHL), 30 (7.1%) with conductive hearing loss (CHL), and 1 patient with mixed HL. The prevalence of HL in each group was as follows: 16.8% in the CAKUT group, 28.6% in the GP group, 12.8% in the CYST group, 24.1% in the PP group, and 14.1% in the others group. HL was more common in higher CKD stages, especially CHL in end-stage renal disease. SNHL was more prevalent in CKD from GP. Of the 82 patients with HL, 50% had renal syndromic HL: 58.8% of SNHL and one-third of CHL were renal syndromic HL.
Conclusion
One-fifth of the childhood-onset CKD had HL. Collectively, renal syndromic HL comprised half of the HL in this study. To improve the quality of life in patients with childhood-onset CKD, we suggest that HL should be considered, requiring surveillance, and if necessary, early intervention.
Figure
Cited by 1 articles
-
Alport syndrome: new advances in the last decade
Ji Hyun Kim
Child Kidney Dis. 2022;26(1):31-39. doi: 10.3339/ckd.22.022.
Reference
-
1. Wang J, Quach J, Sung V, Carew P, Edwards B, Grobler A, et al. Academic, behavioural and quality of life outcomes of slight to mild hearing loss in late childhood: a population-based study. Arch Dis Child. 2019; 104(11):1056–1063. PMID: 31079073.
Article2. Kennedy CR, McCann DC, Campbell MJ, Law CM, Mullee M, Petrou S, et al. Language ability after early detection of permanent childhood hearing impairment. N Engl J Med. 2006; 354(20):2131–2141. PMID: 16707750.
Article3. Sugaya A, Fukushima K, Takao S, Kasai N, Maeda Y, Fujiyoshi A, et al. Impact of reading and writing skills on academic achievement among school-aged hearing-impaired children. Int J Pediatr Otorhinolaryngol. 2019; 126:109619. PMID: 31398591.
Article4. Lieu JE, Tye-Murray N, Karzon RK, Piccirillo JF. Unilateral hearing loss is associated with worse speech-language scores in children. Pediatrics. 2010; 125(6):e1348–e1355. PMID: 20457680.
Article5. Liu W, Meng Q, Wang Y, Yang C, Liu L, Wang H, et al. The association between reduced kidney function and hearing loss: a cross-sectional study. BMC Nephrol. 2020; 21(1):145. PMID: 32321468.
Article7. Smith RJ, Bale JF Jr, White KR. Sensorineural hearing loss in children. Lancet. 2005; 365(9462):879–890. PMID: 15752533.
Article8. Thodi C, Thodis E, Danielides V, Pasadakis P, Vargemezis V. Hearing in renal failure. Nephrol Dial Transplant. 2006; 21(11):3023–3030. PMID: 16935898.
Article9. Bergstrom L, Thompson P, Sando I, Wood RP 2nd. Renal disease. Its pathology, treatment, and effects on the ear. Arch Otolaryngol. 1980; 106(9):567–572. PMID: 6996658.
Article10. Nikolopoulos TP, Kandiloros DC, Segas JV, Nomicos PN, Ferekidis EA, Michelis KE, et al. Auditory function in young patients with chronic renal failure. Clin Otolaryngol Allied Sci. 1997; 22(3):222–225. PMID: 9222626.
Article11. Costa KV, Ferreira SM, Menezes PL. Hearing handicap in patients with chronic kidney disease: a study of the different classifications of the degree of hearing loss. Rev Bras Otorrinolaringol (Engl Ed). 2017; 83(5):580–584.
Article12. Mancini ML, Dello Strologo L, Bianchi PM, Tieri L, Rizzoni G. Sensorineural hearing loss in patients reaching chronic renal failure in childhood. Pediatr Nephrol. 1996; 10(1):38–40. PMID: 8611353.
Article13. Annear NM, Gale DP, Loughlin S, Dorkins HR, Maxwell PH. End-stage renal failure associated with congenital deafness. NDT Plus. 2008; 1(3):171–175. PMID: 25983868.
Article14. Kimberling WJ, Borsa N, Smith RJ. Hearing loss disorders associated with renal disease. Adv Otorhinolaryngol. 2011; 70:75–83. PMID: 21358188.
Article15. Jain S, Kim HG, Lacbawan F, Meliciani I, Wenzel W, Kurth I, et al. Unique phenotype in a patient with CHARGE syndrome. Int J Pediatr Endocrinol. 2011; 2011(1):11. PMID: 21995344.
Article16. Pierides AM, Athanasiou Y, Demetriou K, Koptides M, Deltas CC. A family with the branchio-oto-renal syndrome: clinical and genetic correlations. Nephrol Dial Transplant. 2002; 17(6):1014–1018. PMID: 12032190.
Article17. Bache M, Dheu C, Doray B, Fothergill H, Soskin S, Paris F, et al. Frasier syndrome, a potential cause of end-stage renal failure in childhood. Pediatr Nephrol. 2010; 25(3):549–552. PMID: 19921279.
Article18. Naderpour M, Mortazavi F, Jabbari-Moghaddam Y, Sharifi-Movaghar MH. Auditory brain stem response and otoacoustic emission results in children with end-stage renal disease. Int J Pediatr Otorhinolaryngol. 2011; 75(5):704–707. PMID: 21420741.
Article19. Hirvonen M, Ojala R, Korhonen P, Haataja P, Eriksson K, Gissler M, et al. Visual and hearing impairments after preterm birth. Pediatrics. 2018; 142(2):e20173888. PMID: 30018154.
Article20. Kim SY, Choi BY, Jung EY, Park H, Yoo HN, Park KH. Risk factors for failure in the newborn hearing screen test in very preterm twins. Pediatr Neonatol. 2018; 59(6):586–594. PMID: 29428705.
Article21. Crump C, Sundquist J, Winkleby MA, Sundquist K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ. 2019; 365:l1346. PMID: 31043374.
Article22. Carmody JB, Charlton JR. Short-term gestation, long-term risk: prematurity and chronic kidney disease. Pediatrics. 2013; 131(6):1168–1179. PMID: 23669525.
Article23. Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009; 20(3):629–637. PMID: 19158356.
Article24. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003; 139(2):137–147. PMID: 12859163.
Article25. Olusanya BO, Neumann KJ, Saunders JE. The global burden of disabling hearing impairment: a call to action. Bull World Health Organ. 2014; 92(5):367–373. PMID: 24839326.
Article26. Koffler T, Ushakov K, Avraham KB. Genetics of hearing loss: syndromic. Otolaryngol Clin North Am. 2015; 48(6):1041–1061. PMID: 26443487.27. Rhee J, Lee D, Lim HJ, Park MK, Suh MW, Lee JH, et al. Hearing loss in Korean adolescents: the prevalence thereof and its association with leisure noise exposure. PLoS One. 2019; 14(1):e0209254. PMID: 30608926.
Article28. Bains KS, Chopra H, Sandhu JS, Aulakh BS. Cochlear function in chronic kidney disease and renal transplantation: a longitudinal study. Transplant Proc. 2007; 39(5):1465–1468. PMID: 17580163.
Article29. Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M, et al. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Public Health. 2013; 23(1):146–152. PMID: 22197756.
Article30. Ari-Even Roth D, Hildesheimer M, Maayan-Metzger A, Muchnik C, Hamburger A, Mazkeret R, et al. Low prevalence of hearing impairment among very low birthweight infants as detected by universal neonatal hearing screening. Arch Dis Child Fetal Neonatal Ed. 2006; 91(4):F257–62. PMID: 16531449.
Article31. Cristobal R, Oghalai JS. Hearing loss in children with very low birth weight: current review of epidemiology and pathophysiology. Arch Dis Child Fetal Neonatal Ed. 2008; 93(6):F462–8. PMID: 18941031.
Article32. Youn Y, Lee SM, Hwang JH, Cho SJ, Kim EK, Kim EA, et al. National registry data from Korean Neonatal Network: two-year outcomes of Korean very low birth weight infants born in 2013-2014. J Korean Med Sci. 2018; 33(48):e309. PMID: 30473651.
Article33. American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007; 120(4):898–921. PMID: 17908777.34. Wroblewska-Seniuk K, Greczka G, Dabrowski P, Szyfter-Harris J, Mazela J. Hearing impairment in premature newborns–Analysis based on the national hearing screening database in Poland. PLoS One. 2017; 12(9):e0184359. PMID: 28910311.
Article35. Kroes HY, Van Zanten BG, De Ru SA, Boon M, Mancini GM, Van der Knaap MS, et al. Is hearing loss a feature of Joubert syndrome, a ciliopathy? Int J Pediatr Otorhinolaryngol. 2010; 74(9):1034–1038. PMID: 20591505.
Article36. Kim SY, Kang HG, Kim EK, Choi JH, Choi Y, Cheong HI. Survival over 2 years of autosomal-recessive renal tubular dysgenesis. Clin Kidney J. 2012; 5(1):56–58. PMID: 26069751.
Article37. Dallapiccola B, Zelante L, Mingarelli R, Pellegrino M, Bertozzi V. Baller-Gerold syndrome: case report and clinical and radiological review. Am J Med Genet. 1992; 42(3):365–368. PMID: 1536180.
Article38. Robb PJ, Williamson I. Otitis media with effusion in children: current management. J Paediatr Child Health. 2016; 26(1):9–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetic Background of Congenital Hearing Loss
- Nephronophthisis
- Renal Failure with Branchio-Oto-Renal Syndrome
- Etiology of Hearing Loss and Genetic Hearing Loss
- A 250-kb Microdeletion Identified in Chromosome 16 Is Associated With Non-Syndromic Sensorineural Hearing Loss in a South Indian Consanguineous Family