J Korean Neurosurg Soc.
2020 Nov;63(6):757-766. 10.3340/jkns.2019.0230.
Early versus Delayed Surgery for Spinal Epidural Abscess : Clinical Outcome and Health-Related Quality of Life
- Affiliations
-
- 1Department of Neurosurgery, Goethe University, Frankfurt am Main, Germany
- KMID: 2508606
- DOI: http://doi.org/10.3340/jkns.2019.0230
Abstract
Objective
: Spinal epidural abscess (SEA) is a severe and life-threatening disease. Although commonly performed, the effect of timing in surgical treatment on patient outcome is still unclear. With this study, we aim to provide evidence for early surgical treatment in patients with SEA.
Methods
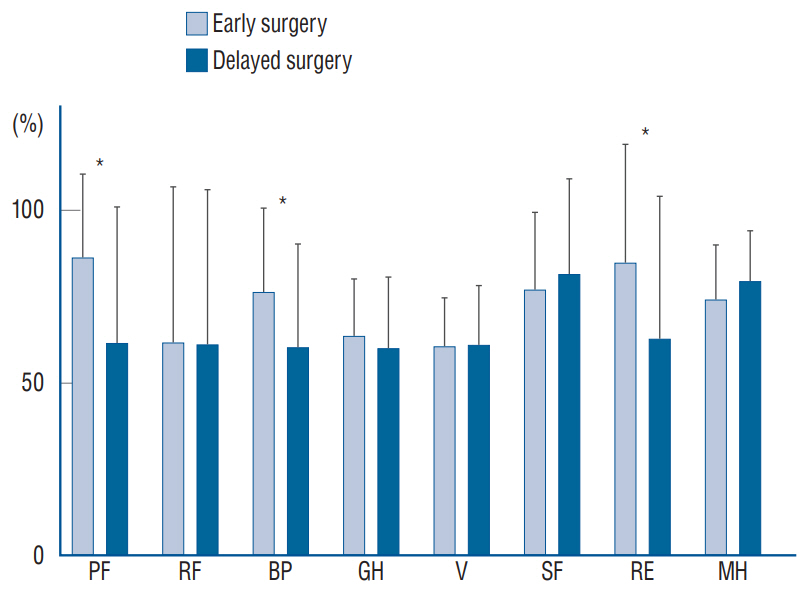
: Patients treated for SEA in the authors’ department between 2007 and 2016 were included for analysis and retrospectively analyzed for basic clinical parameters and outcome. Pre- and postoperative neurological status were assessed using the American Spinal Injury Association Impairment Scale (AIS). The self-reported quality of life (QOL) based on the Short-Form Health Survey 36 (SF-36) was assessed prospectively. Surgery was defined as “early”, when performed within 12 hours after admission and “late” when performed thereafter. Conservative therapy was preferred and recommend in patients without neurological deficits and in patients denying surgical intervention.
Results
: One hundred and twenty-three patients were included in this study. Forty-nine patients (39.8%) underwent early, 47 patients (38.2%) delayed surgery and 27 (21.9%) conservative therapy. No significant differences were observed regarding mean age, sex, diabetes, prior history of spinal infection, and bony destruction. Patients undergoing early surgery revealed a significant better clinical outcome before discharge than patients undergoing late surgery (p=0.001) and conservative therapy. QOL based on SF-36 were significantly better in the early surgery cohort in two of four physical items (physical functioning and bodily pain) and in one of four psychological items (role limitation) after a mean follow-up period of 58 months. Readmission to the hospital and failure of conservative therapy were observed more often in patients undergoing conservative therapy.
Conclusion
: Our data on both clinical outcome and QOL provide evidence for early surgery within 12 hours after admission in patients with SEA.
Figure
Reference
-
References
1. Adogwa O, Karikari IO, Carr KR, Krucoff M, Ajay D, Fatemi P, et al. Spontaneous spinal epidural abscess in patients 50 years of age and older: a 15-year institutional perspective and review of the literature: clinical article. J Neurosurg Spine. 20:344–349. 2014.
Article2. Bydon M, De la Garza-Ramos R, Macki M, Naumann M, Sciubba DM, Wolinsky JP, et al. Spinal instrumentation in patients with primary spinal infections does not lead to greater recurrent infection rates: an analysis of 118 cases. World Neurosurg. 82:e807–e814. 2014.
Article3. Connor DE Jr, Chittiboina P, Caldito G, Nanda A. Comparison of operative and nonoperative management of spinal epidural abscess: a retrospective review of clinical and laboratory predictors of neurological outcome. J Neurosurg Spine. 19:119–127. 2013.
Article4. Curry WT Jr, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: clinical presentation, management, and outcome. Surg Neurol. 63:364–371. discussion 371. 2005.
Article5. Danner RL, Hartman BJ. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 9:265–274. 1987.6. Darouiche RO. Spinal epidural abscess. N Engl J Med. 355:2012–2020. 2006.
Article7. Darouiche RO, Hamill RJ, Greenberg SB, Weathers SW, Musher DM. Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore). 71:369–385. 1992.8. Davis DP, Wold RM, Patel RJ, Tran AJ, Tokhi RN, Chan TC, et al. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 26:285–291. 2004.
Article9. Dietz N, Sharma M, Alhourani A, Ugiliweneza B, Wang D, Nuño M, et al. Outcomes of decompression and fusion for treatment of spinal infection. Neurosurg Focus. 46:E7. 2019.
Article10. Feldenzer JA, McKeever PE, Schaberg DR, Campbell JA, Hoff JT. Experimental spinal epidural abscess: a pathophysiological model in the rabbit. Neurosurgery. 20:859–867. 1987.
Article11. Foreman SC, Schwaiger BJ, Gempt J, Jungmann PM, Kehl V, Delbridge C, et al. MR and CT Imaging to optimize CT-guided biopsies in suspected spondylodiscitis. World Neurosurg. 99:726–734.e7. 2017.
Article12. Garrido E, Rosenwasser RH. Experience with the suction-irrigation technique in the management of spinal epidural infection. Neurosurgery. 12:678–679. 1983.
Article13. Gessler F, Mutlak H, Lamb S, Hartwich M, Adelmann M, Platz J, et al. The impact of tracheostomy timing on clinical outcome and adverse events in poor-grade subarachnoid hemorrhage. Crit Care Med. 43:2429–2438. 2015.
Article14. Gessler F, Mutlak H, Tizi K, Senft C, Setzer M, Seifert V, et al. Postoperative patient-controlled epidural analgesia in patients with spondylodiscitis and posterior spinal fusion surgery. J Neurosurg Spine. 24:965–970. 2016.
Article15. Ghobrial GM, Beygi S, Viereck MJ, Maulucci CM, Sharan A, Heller J, et al. Timing in the surgical evacuation of spinal epidural abscesses. Neurosurg Focus. 37:E1. 2014.
Article16. Hlavin ML, Kaminski HJ, Ross JS, Ganz E. Spinal epidural abscess: a ten-year perspective. Neurosurgery. 27:177–184. 1990.
Article17. Karikari IO, Powers CJ, Reynolds RM, Mehta AI, Isaacs RE. Management of a spontaneous spinal epidural abscess: a single-center 10-year experience. Neurosurgery. 65:919–923. discussion 923-924. 2009.18. Khanna RK, Malik GM, Rock JP, Rosenblum ML. Spinal epidural abscess: evaluation of factors influencing outcome. Neurosurgery. 39:958–964. 1996.
Article19. Kim SD, Melikian R, Ju KL, Zurakowski D, Wood KB, Bono CM, et al. Independent predictors of failure of nonoperative management of spinal epidural abscesses. Spine J. 14:1673–1679. 2014.
Article20. Koo DW, Townson AF, Dvorak MF, Fisher CG. Spinal epidural abscess: a 5-year case-controlled review of neurologic outcomes after rehabilitation. Arch Phys Med Rehabil. 90:512–516. 2009.
Article21. Kuklo TR, Potter BK, Bell RS, Moquin RR, Rosner MK. Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech. 19:376–382. 2006.
Article22. Lu ML, Niu CC, Tsai TT, Fu TS, Chen LH, Chen WJ. Transforaminal lumbar interbody debridement and fusion for the treatment of infective spondylodiscitis in the lumbar spine. Eur Spine J. 24:555–560. 2015.
Article23. Lyu RK, Chen CJ, Tang LM, Chen ST. Spinal epidural abscess successfully treated with percutaneous, computed tomography-guided, needle aspiration and parenteral antibiotic therapy: case report and review of the literature. Neurosurgery. 51:509–512. discussion 512. 2002.
Article24. Özkan N, Wrede K, Ardeshiri A, Hagel V, Dammann P, Ringelstein A, et al. Cervical spondylodiscitis--a clinical analysis of surgically treated patients and review of the literature. Clin Neurol Neurosurg. 117:86–92. 2014.
Article25. Patel AR, Alton TB, Bransford RJ, Lee MJ, Bellabarba CB, Chapman JR. Spinal epidural abscesses: risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 14:326–330. 2014.
Article26. Przybylski GJ, Sharan AD. Single-stage autogenous bone grafting and internal fixation in the surgical management of pyogenic discitis and vertebral osteomyelitis. J Neurosurg. 94(1 Suppl):1–7. 2001.
Article27. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 23:175–204. discussion 205. 2000.
Article28. Rigamonti D, Liem L, Sampath P, Knoller N, Namaguchi Y, Schreibman DL, et al. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 52:189–196. discussion 197. 1999.
Article29. Sampath P, Rigamonti D. Spinal epidural abscess: a review of epidemiology, diagnosis, and treatment. J Spinal Disord. 12:89–93. 1999.30. Savage K, Holtom PD, Zalavras CG. Spinal epidural abscess: early clinical outcome in patients treated medically. Clin Orthop Relat Res. 439:56–60. 2005.31. Siddiq F, Chowfin A, Tight R, Sahmoun AE, Smego RA Jr. Medical vs surgical management of spinal epidural abscess. Arch Intern Med. 164:2409–2412. 2004.
Article32. Sinha S, Singh AK, Gupta V, Singh D, Takayasu M, Yoshida J. Surgical management and outcome of tuberculous atlantoaxial dislocation: a 15-year experience. Neurosurgery. 52:331–338. discussion 338-339. 2003.
Article33. Soehle M, Wallenfang T. Spinal epidural abscesses: clinical manifestations, prognostic factors, and outcomes. Neurosurgery. 51:79–85. discussion 86-87. 2002.
Article34. Stratton A, Gustafson K, Thomas K, James MT. Incidence and risk factors for failed medical management of spinal epidural abscess: a systematic review and meta-analysis. J Neurosurg Spine. 26:81–89. 2017.
Article35. Suppiah S, Meng Y, Fehlings MG, Massicotte EM, Yee A, Shamji MF. How best to manage the spinal epidural abscess? A current systematic review. World Neurosurg. 93:20–28. 2016.
Article36. Tuchman A, Pham M, Hsieh PC. The indications and timing for operative management of spinal epidural abscess: literature review and treatment algorithm. Neurosurg Focus. 37:E8. 2014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Spinal Epidural Abscess after Epidural Analgesia: Case Report
- Spinal Epidural and Subdural Abscess following Epidural Catheterization: A case report
- Lumbar Spinal Epidural Abscess Combined with Cauda Equina Syndrome: A Case Report
- Epidural Abscess Following Epidural Catheterization for Painless Mobilization after Total Knee Arthroplasty
- Rapidly Progressive Gas-containing Lumbar Spinal Epidural Abscess