Ann Rehabil Med.
2020 Oct;44(5):353-361. 10.5535/arm.19164.
Association Between Latency of Dermatomal Sensory-Evoked Potentials and Quantitative Radiologic Findings of Narrowing in Lumbar Spinal Stenosis
- Affiliations
-
- 1Department of Health Service, Gunsan-si Health Center, Gunsan, Korea
- 2Department of Physical Medicine and Rehabilitation, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea
- 3Department of Neurosurgery, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea
- KMID: 2508460
- DOI: http://doi.org/10.5535/arm.19164
Abstract
Objective
To identify the difference of quantitative radiologic stenosis between a normal latency group and an abnormal latency group, and to investigate the association of dermatomal somatosensory-evoked potential (DSEP) with magnetic resonance imaging (MRI) findings of narrowing in patients with lumbar spinal stenosis (LSS).
Methods
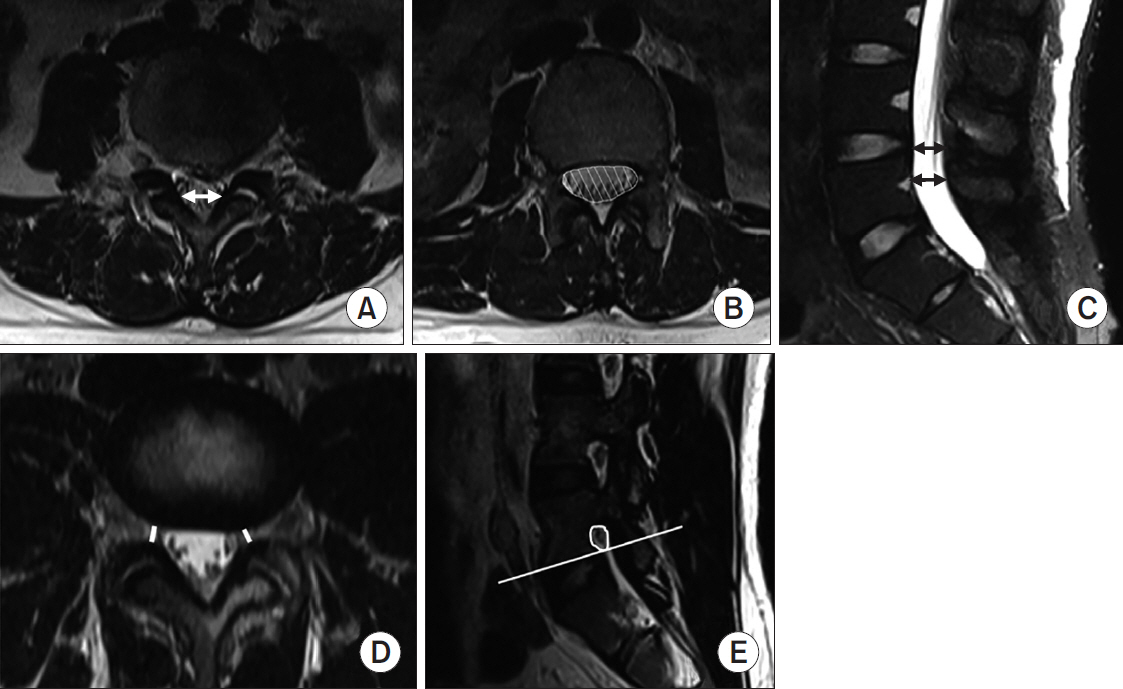
We retrospectively reviewed the clinical records and P40 latencies of L5 DSEP of 40 patients with unilateral symptoms of LSS at the L4–5 disc level. Quantitative assessments of stenosis in lumbar spine MRI were performed with measurements of the anteroposterior diameter (APD), cross-sectional area (CSA) of the dural sac, ligamentous interfacet distance (LID), CSA of the neural foramen (CSA-NF), and subarticular zone width. Analyses were conducted through comparisons of radiologic severity between the normal and abnormal latency groups and correlation between radiologic severity of stenosis and latency of DSEP in absolute (APD <10 mm) and relative (APD <13 mm) stenosis.
Results
The radiologic severities of lumbar stenosis were not significantly different between the normal and abnormal latency groups. In absolute and relative stenosis, latency showed a significant negative correlation with APD (r=-0.539, r=-0.426) and LID (r=-0.459, r=-0.494). In patients with relative stenosis, a weak significant positive correlation was found between latency and CSA-NF (r=0.371, p=0.048). LID was the only significant factor for latency (β=-0.930, p=0.011).
Conclusion
The normal and abnormal DSEP groups showed no significant differences inradiologic severity. The latency of DSEP had a negative correlation with the severity of central stenosis, and LID was an influencing factor.
Figure
Reference
-
1. Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013; 13:734–43.
Article2. Fraser JF, Huang RC, Girardi FP, Cammisa FP Jr. Pathogenesis, presentation, and treatment of lumbar spinal stenosis associated with coronal or sagittal spinal deformities. Neurosurg Focus. 2003; 14:e6.
Article3. Geisser ME, Haig AJ, Tong HC, Yamakawa KS, Quint DJ, Hoff JT, et al. Spinal canal size and clinical symptoms among persons diagnosed with lumbar spinal stenosis. Clin J Pain. 2007; 23:780–5.
Article4. Lee SY, Kim TH, Oh JK, Lee SJ, Park MS. Lumbar stenosis: a recent update by review of literature. Asian Spine J. 2015; 9:818–28.
Article5. Lurie JD, Tosteson TD, Tosteson A, Abdu WA, Zhao W, Morgan TS, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2015; 40:63–76.6. De Schepper EI, Overdevest GM, Suri P, Peul WC, Oei EH, Koes BW, et al. Diagnosis of lumbar spinal stenosis: an updated systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976). 2013; 38:E469–81.7. Wassenaar M, van Rijn RM, van Tulder MW, Verhagen AP, van der Windt DA, Koes BW, et al. Magnetic resonance imaging for diagnosing lumbar spinal pathology in adult patients with low back pain or sciatica: a diagnostic systematic review. Eur Spine J. 2012; 21:220–7.
Article8. Steurer J, Roner S, Gnannt R, Hodler J; LumbSten Research Collaboration. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review. BMC Musculoskelet Disord. 2011; 12:175.
Article9. Mamisch N, Brumann M, Hodler J, Held U, Brunner F, Steurer J, et al. Radiologic criteria for the diagnosis of spinal stenosis: results of a Delphi survey. Radiology. 2012; 264:174–9.
Article10. American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine: somatosensory evoked potentials: clinical uses. Muscle Nerve Suppl. 1999; 8:S111–8.11. Snowden ML, Haselkorn JK, Kraft GH, Bronstein AD, Bigos SJ, Slimp JC, et al. Dermatomal somatosensory evoked potentials in the diagnosis of lumbosacral spinal stenosis: comparison with imaging studies. Muscle Nerve. 1992; 15:1036–44.
Article12. Egli D, Hausmann O, Schmid M, Boos N, Dietz V, Curt A. Lumbar spinal stenosis: assessment of cauda equina involvement by electrophysiological recordings. J Neurol. 2007; 254:741–50.
Article13. Han TR, Kim JH, Paik NJ. Electrodiagnostic study in spinal stenosis. J Korean Acad Rehabil Med. 1992; 16:460–6.14. Eltantawi GA, Hassan MM, Sultan HE, Elnekiedy AA, Naby HM. Somatosensory-evoked potentials as an add-on diagnostic procedure to imaging studies in patients with lumbosacral spinal canal stenosis. Alex J Med. 2012; 48:207–14.
Article15. Shen N, Wang G, Chen J, Wu X, Wang Y. Evaluation of degree of nerve root injury by dermatomal somatosensory evoked potential following lumbar spinal stenosis. Neural Regen Res. 2008; 3:1249–52.16. Aminoff MJ, Goodin DS, Barbaro NM, Weinstein PR, Rosenblum ML. Dermatomal somatosensory evoked potentials in unilateral lumbosacral radiculopathy. Ann Neurol. 1985; 17:171–6.17. Han TR. Considerations in measuring somatosensory evoked potential. J Korean Acad Rehabil Med. 1993; 17:151–6.18. Liu X, Konno S, Miyamoto M, Gembun Y, Horiguchi G, Ito H. Clinical usefulness of assessing lumbar somatosensory evoked potentials in lumbar spinal stenosis: clinical article. J Neurosurg Spine. 2009; 11:71–8.19. Sipola P, Leinonen V, Niemelainen R, Aalto T, Vanninen R, Manninen H, et al. Visual and quantitative assessment of lateral lumbar spinal canal stenosis with magnetic resonance imaging. Acta Radiol. 2011; 52:1024–31.
Article20. Strojnik T. Measurement of the lateral recess angle as a possible alternative for evaluation of the lateral recess stenosis on a CT scan. Wien Klin Wochenschr. 2001; 113 Suppl 3:53–8.21. Essa ZM, Al-Hashimi AF, Nema IS. Dermatomal versus mixed somatosensory evoked potentials in the diagnosis of lumbosacral spinal canal stenosis. J Clin Neurophysiol. 2018; 35:388–98.
Article22. Kuittinen P, Sipola P, Aalto TJ, Maatta S, Parviainen A, Saari T, et al. Correlation of lateral stenosis in MRI with symptoms, walking capacity and EMG findings in patients with surgically confirmed lateral lumbar spinal canal stenosis. BMC Musculoskelet Disord. 2014; 15:247.
Article23. Andreisek G, Deyo RA, Jarvik JG, Porchet F, Winklhofer SF, Steurer J, et al. Consensus conference on core radiological parameters to describe lumbar stenosis: an initiative for structured reporting. Eur Radiol. 2014; 24:3224–32.24. Andreisek G, Imhof M, Wertli M, Winklhofer S, Pfirrmann CW, Hodler J, et al. A systematic review of semiquantitative and qualitative radiologic criteria for the diagnosis of lumbar spinal stenosis. AJR Am J Roentgenol. 2013; 201:W735–46.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Determination of Neurological Impairment Level in Thoracic SpinalCord Injuries using Dermatomal Somatosensory Evoked Potentials
- Diagnostic Usefulness of Dermatomal Somatosensory Evoked Potentials by Low Intensity Stimulation in Lumbar Radiculopathy
- The relationship between the configuration of the spine and somatosensory evoked potential in lumbar spinal stenosis
- Changes of motor evoked potentials and spinal cord evoked potentials following spinal cord injury in rats
- Changes in Dermatomal Somatosensory Evoked Potentials according to Stimulation Intensity and Severity of Carpal Tunnel Syndrome