Korean Circ J.
2020 Nov;50(11):984-994. 10.4070/kcj.2020.0057.
Impact of Angiotensin II Receptor Blockers on Clinical Outcomes after Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction Based on Data from the Korean National Health Insurance Database (2005–2014)
- Affiliations
-
- 1Department of Cardiology, Sanggye-Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 2Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea
- 3Department of Cardiology, Myeongji Hospital, Goyang, Korea
- 4Cardiovascular & Arrhythmia Center, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2508279
- DOI: http://doi.org/10.4070/kcj.2020.0057
Abstract
- Background and Objectives
The effectiveness of angiotensin II receptor blockers (ARBs) compared with angiotensin converting enzyme inhibitors (ACEIs) in patients with acute myocardial infarction (AMI) has not been established. We investigated the effects of ARBs on clinical outcomes after percutaneous coronary intervention (PCI) in AMI patients.
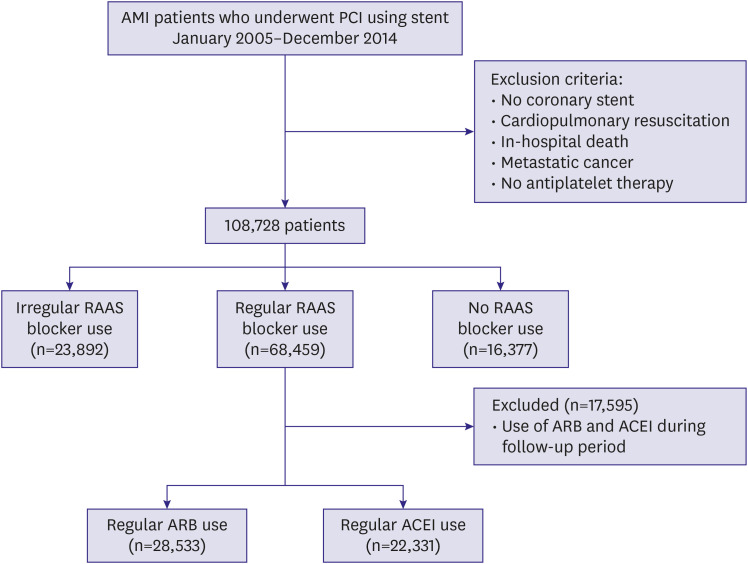
Methods
Patients receiving ACEIs or ARBs after AMI treated with PCI between January 2005 and December 2014 were selected from the Korean National Health Insurance Service database. The primary endpoint was major cardiovascular adverse event (MACE; all-cause death, myocardial infarct [MI], or stroke).
Results
We included patients regularly taking ACEIs (n=22,331) or ARBs (n=28,533) (medication possession ratio ≥80%). Compared with the ACEI group, the ARB group contained more females (31% vs. 18%), were older (mean, 63 vs. 60 years), and had more comorbidities, including hypertension (62.8% vs. 44.8%), diabetes (33.9% vs. 26.4%), congestive heart failure (7.9% vs. 4.3%), chronic obstructive pulmonary disease (25.5% vs. 18.9%), and end-stage renal disease (1.3% vs. 0.4%) (p<0.001 for all). After propensity score–matching, ARBs were associated with a 23% lower risk of MACE (hazard ratio [HR], 0.774; 95% confidence interval [CI], 0.715–0.838; p<0.001) than ACEIs. ARB use was also associated with a significantly reduced risk of death (HR, 0.741; 95% CI, 0.659–0.834; p<0.001), MI (HR, 0.731; 95% CI, 0.638–0.837; p<0.001), and revascularization (HR, 0.816; 95% CI, 0.773–0.861; p<0.001).
Conclusions
ARB use was associated with a lower risk of MACE, MI, and revascularization than ACEIs in our retrospective analysis of AMI patients who underwent PCI.
Keyword
Figure
Cited by 1 articles
-
Renin-Angiotensin System Blockade in Acute Myocardial Infarction: Is There a Winner?
Hak Seung Lee, Jeehoon Kang
Korean Circ J. 2020;50(11):995-997. doi: 10.4070/kcj.2020.0398.
Reference
-
1. Ma TK, Kam KK, Yan BP, Lam YY. Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. Br J Pharmacol. 2010; 160:1273–1292. PMID: 20590619.
Article2. Nehme A, Zibara K. Efficiency and specificity of RAAS inhibitors in cardiovascular diseases: how to achieve better end-organ protection? Hypertens Res. 2017; 40:903–909. PMID: 28680167.
Article3. Pfeffer MA, Braunwald E, Moyé LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. N Engl J Med. 1992; 327:669–677. PMID: 1386652.4. The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet. 1993; 342:821–828. PMID: 8104270.5. Heart Outcomes Prevention Evaluation Study Investigators. Yusuf S, Sleight P, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000; 342:145–153. PMID: 10639539.
Article6. Dagenais GR, Pogue J, Fox K, Simoons ML, Yusuf S. Angiotensin-converting-enzyme inhibitors in stable vascular disease without left ventricular systolic dysfunction or heart failure: a combined analysis of three trials. Lancet. 2006; 368:581–588. PMID: 16905022.
Article7. Danchin N, Cucherat M, Thuillez C, Durand E, Kadri Z, Steg PG. Angiotensin-converting enzyme inhibitors in patients with coronary artery disease and absence of heart failure or left ventricular systolic dysfunction: an overview of long-term randomized controlled trials. Arch Intern Med. 2006; 166:787–796. PMID: 16606817.8. McDowell SE, Coleman JJ, Ferner RE. Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine. BMJ. 2006; 332:1177–1181. PMID: 16679330.
Article9. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 64:e139–e228. PMID: 25260718.10. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37:267–315. PMID: 26320110.11. Dickstein K, Kjekshus J. OPTIMAAL Steering Committee of the OPTIMAAL Study Group. Effects of losartan and captopril on mortality and morbidity in high-risk patients after acute myocardial infarction: the OPTIMAAL randomised trial. Optimal Trial in Myocardial Infarction with Angiotensin II Antagonist Losartan. Lancet. 2002; 360:752–760. PMID: 12241832.12. Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003; 349:1893–1906. PMID: 14610160.
Article13. Kozma CM, Dickson M, Phillips AL, Meletiche DM. Medication possession ratio: implications of using fixed and variable observation periods in assessing adherence with disease-modifying drugs in patients with multiple sclerosis. Patient Prefer Adherence. 2013; 7:509–516. PMID: 23807840.
Article14. Ennezat PV, Berlowitz M, Sonnenblick EH, Le Jemtel TH. Therapeutic implications of escape from angiotensin-converting enzyme inhibition in patients with chronic heart failure. Curr Cardiol Rep. 2000; 2:258–262. PMID: 10980901.
Article15. Lang CC, Struthers AD. Targeting the renin-angiotensin-aldosterone system in heart failure. Nat Rev Cardiol. 2013; 10:125–134. PMID: 23319100.
Article16. Morimoto T, Gandhi TK, Fiskio JM, et al. An evaluation of risk factors for adverse drug events associated with angiotensin-converting enzyme inhibitors. J Eval Clin Pract. 2004; 10:499–509. PMID: 15482412.
Article17. Singh A, Bangalore S. Do angiotensin receptor blockers prevent myocardial infarctions as well as other initial therapies? Curr Opin Cardiol. 2012; 27:381–385. PMID: 22525329.
Article18. Cheng J, Zhang W, Zhang X, et al. Effect of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on all-cause mortality, cardiovascular deaths, and cardiovascular events in patients with diabetes mellitus: a meta-analysis. JAMA Intern Med. 2014; 174:773–785. PMID: 24687000.19. Ricci F, Di Castelnuovo A, Savarese G, Perrone Filardi P, De Caterina R. ACE-inhibitors versus angiotensin receptor blockers for prevention of events in cardiovascular patients without heart failure - A network meta-analysis. Int J Cardiol. 2016; 217:128–134. PMID: 27179902.
Article20. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619. PMID: 22922416.21. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 61:e78–e140. PMID: 23256914.22. Hara M, Sakata Y, Nakatani D, et al. Comparison of 5-year survival after acute myocardial infarction using angiotensin-converting enzyme inhibitor versus angiotensin II receptor blocker. Am J Cardiol. 2014; 114:1–8. PMID: 24819900.
Article23. Ann SH, Strauss MH, Park GM, et al. Comparison between angiotensin-converting enzyme inhibitor and angiotensin receptor blocker after percutaneous coronary intervention. Int J Cardiol. 2020; 306:35–41. PMID: 31727411.
Article24. Choi IS, Park IB, Lee K, et al. Angiotensin-converting enzyme inhibitors provide better long-term survival benefits to patients with AMI than angiotensin II receptor blockers after survival hospital discharge. J Cardiovasc Pharmacol Ther. 2019; 24:120–129.
Article25. Lee JH, Bae MH, Yang DH, et al. Angiotensin II type 1 receptor blockers as a first choice in patients with acute myocardial infarction. Korean J Intern Med. 2016; 31:267–276. PMID: 26701233.
Article26. Yang JH, Hahn JY, Song YB, et al. Angiotensin receptor blocker in patients with ST segment elevation myocardial infarction with preserved left ventricular systolic function: prospective cohort study. BMJ. 2014; 349:g6650. PMID: 25398372.
Article27. Savarese G, Costanzo P, Cleland JG, et al. A meta-analysis reporting effects of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in patients without heart failure. J Am Coll Cardiol. 2013; 61:131–142. PMID: 23219304.
Article28. Strauss MH, Hall AS. Angiotensin receptor blockers may increase risk of myocardial infarction: unraveling the ARB-MI paradox. Circulation. 2006; 114:838–854. PMID: 16923768.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prognostic Impact of Hypertriglyceridemia and Abdominal Obesity in Acute Myocardial Infarction Patients Underwent Percutaneous Coronary Intervention
- Angiotensin Receptor Blockers as an Alternative to Angiotensin-Converting Enzyme Inhibitors in Patients with Acute Myocardial Infarction Undergoing Percutaneous Coronary Intervention
- Pharmacotherapy for acute myocardial infarction
- Clinical outcome in elderly patients older than 70 years with acute myocardial infarction after use of platelet glycoprotein IIb/IIIa receptor blocker during percutaneous coronary intervention: Comparison with those younger than 70 years
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction