J Korean Assoc Oral Maxillofac Surg.
2020 Oct;46(5):328-334. 10.5125/jkaoms.2020.46.5.328.
Development and validation of a difficulty index for mandibular third molars with extraction time
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Section of Dentistry, Armed Forces Capital Dental Hospital, Armed Forces Medical Command, Seongnam, Korea
- 2Biomedical Research Institute, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- KMID: 2508257
- DOI: http://doi.org/10.5125/jkaoms.2020.46.5.328
Abstract
Objectives
This study aimed to validate the effectiveness of a recently proposed difficulty index for removal of impacted mandibular third molars based on extraction time and suggest a modified difficulty index including the presence of pathologic conditions associated with third molars.
Materials and Methods
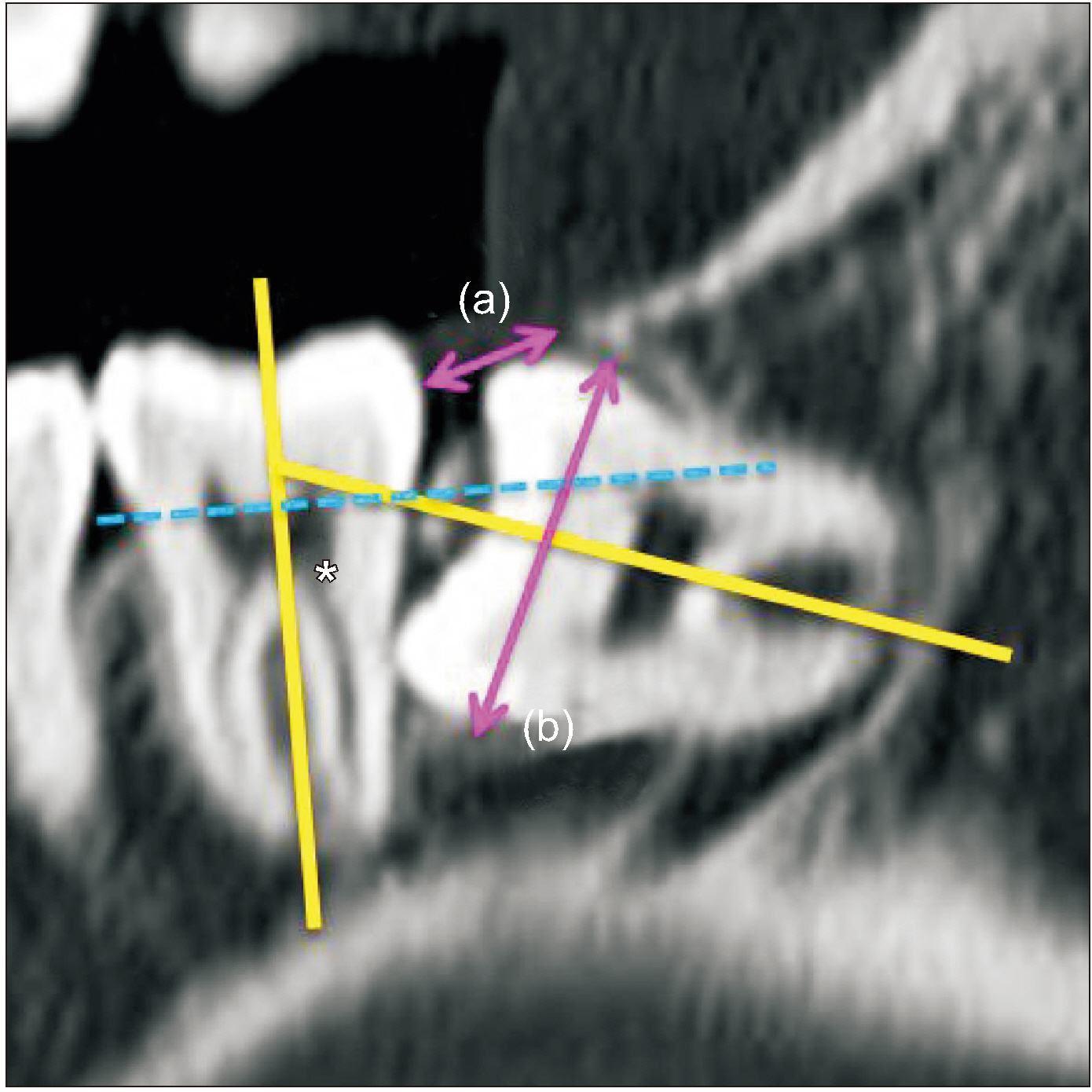
This retrospective study enrolled 65 male patients younger than 25 years with third molars. Extraction time was calculated from start of the incision to the last suture. The difficulty scores for third molars were based on spatial relationship (1-5 points), depth (1-4 points), and ramus relationship (1-3 points) using cone-beam computed tomography. The difficulty index was defined as follows: I (3-4 points), II (5-7 points), III (8-10 points), and IV (11-12 points). The modified difficulty score was calculated by adding one point to the difficulty score if the third molar was associated with a pathologic condition. Two modified difficulty indices, based on the presence of pathologic conditions, were as follows: the half-level up difficulty index (HDI) and the one-level up difficulty index (ODI) from the recently proposed difficulty index.
Results
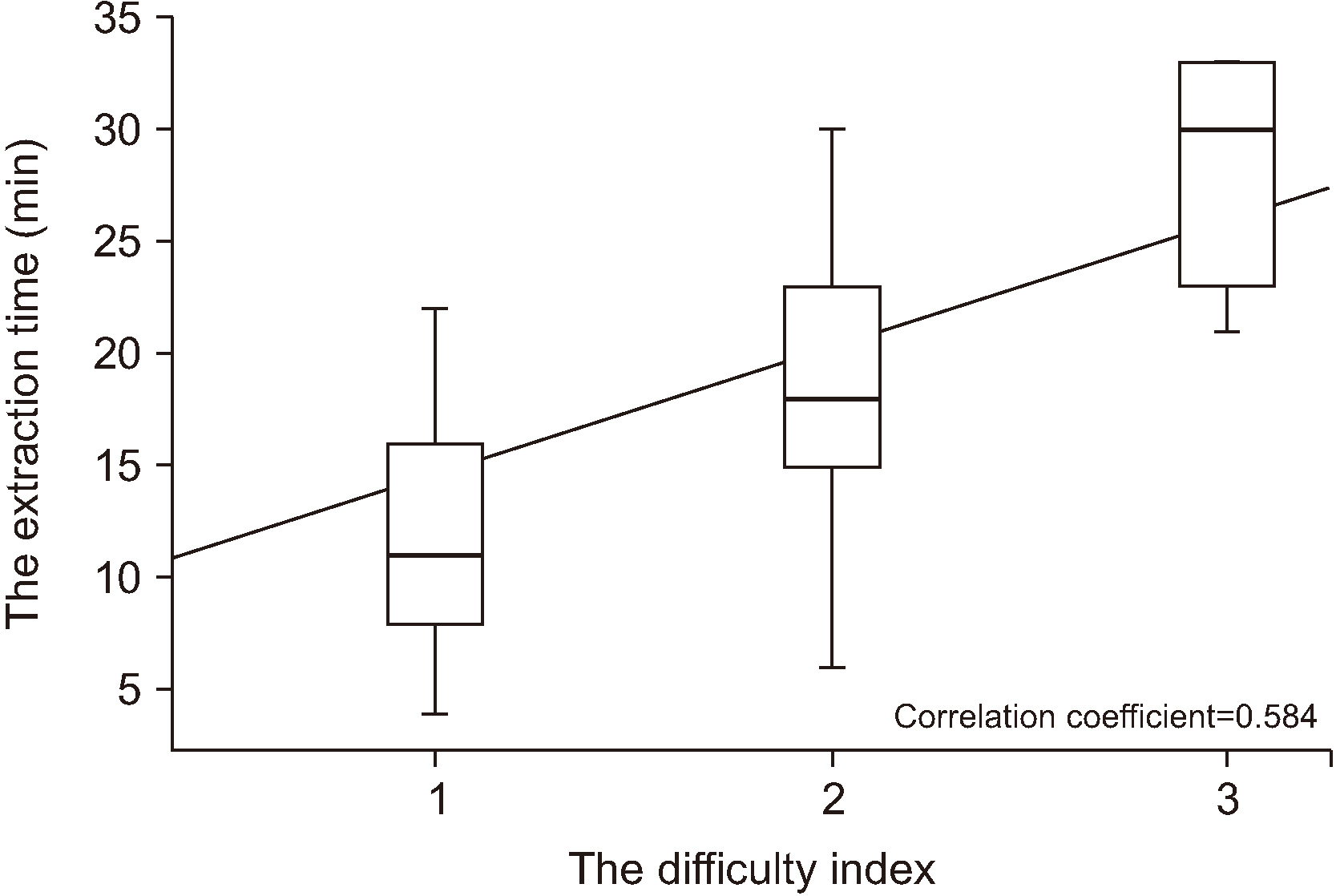
The correlations between extraction time and difficulty index and or modified difficulty indices were significant (P<0.001). The correlation coefficient between extraction time and difficulty index was 0.584. The correlation coefficients between extraction time and HDI and ODI were 0.728 and 0.764, respectively.
Conclusion
Extraction time of impacted third molars exhibited a moderate correlation with difficulty index and was strongly correlated with the modified indices. Considering the clinical implications, the difficulty index of surgical extraction should take into consideration the pathologic conditions associated with third molars.
Figure
Cited by 1 articles
-
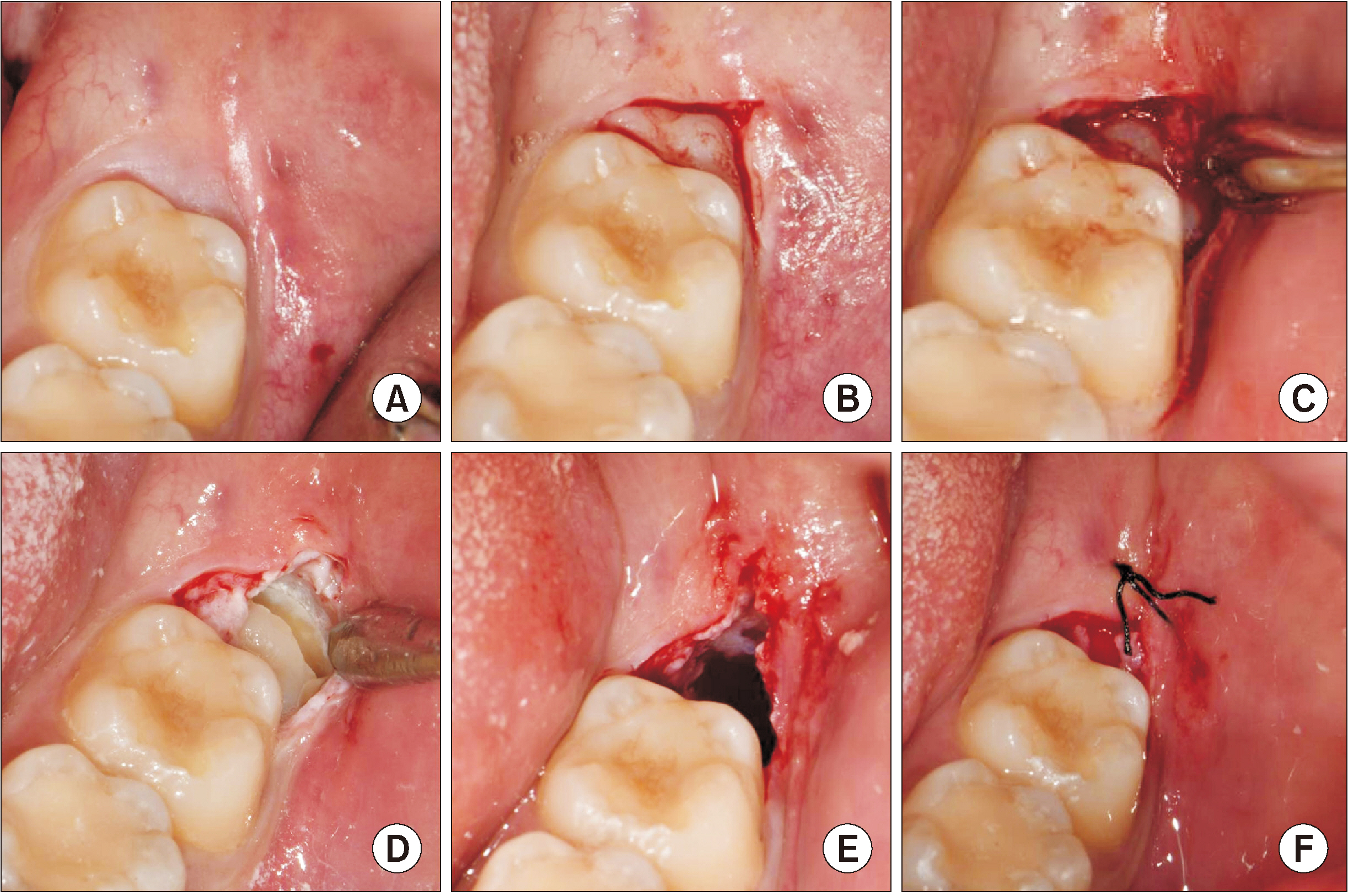
Effect of a vertical incision on postoperative swelling after an impacted mandibular third molar extraction: two cases with split-mouth designed magnetic resonance imaging analysis
Jeong-Kui Ku, Sung Hyun Baik, Jae-Young Kim, Jong-Ki Huh
J Korean Assoc Oral Maxillofac Surg. 2023;49(2):91-95. doi: 10.5125/jkaoms.2023.49.2.91.
Reference
-
References
1. Pell GJ, Gregory GT. 1933; Impacted mandibular third molars: classification and modified technique for removal. Dent Dig. 39:330–7.2. Yuasa H, Kawai T, Sugiura M. 2002; Classification of surgical difficulty in extracting impacted third molars. Br J Oral Maxillofac Surg. 40:26–31. https://doi.org/10.1054/bjom.2001.0684 . DOI: 10.1054/bjom.2001.0684. PMID: 11883966.
Article3. Gbotolorun OM, Arotiba GT, Ladeinde AL. 2007; Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J Oral Maxillofac Surg. 65:1977–83. https://doi.org/10.1016/j.joms.2006.11.030 . DOI: 10.1016/j.joms.2006.11.030. PMID: 17884525.
Article4. Sammartino G, Gasparro R, Marenzi G, Trosino O, Mariniello M, Riccitiello F. 2017; Extraction of mandibular third molars: proposal of a new scale of difficulty. Br J Oral Maxillofac Surg. 55:952–7. https://doi.org/10.1016/j.bjoms.2017.09.012 . DOI: 10.1016/j.bjoms.2017.09.012. PMID: 29054564.
Article5. Kim JY, Yong HS, Park KH, Huh JK. 2019; Modified difficult index adding extremely difficult for fully impacted mandibular third molar extraction. J Korean Assoc Oral Maxillofac Surg. 45:309–15. https://doi.org/10.5125/jkaoms.2019.45.6.309 . DOI: 10.5125/jkaoms.2019.45.6.309. PMID: 31966975. PMCID: PMC6955420.
Article6. Ishii S, Abe S, Moro A, Yokomizo N, Kobayashi Y. 2017; The horizontal inclination angle is associated with the risk of inferior alveolar nerve injury during the extraction of mandibular third molars. Int J Oral Maxillofac Surg. 46:1626–34. https://doi.org/10.1016/j.ijom.2017.07.010 . DOI: 10.1016/j.ijom.2017.07.010. PMID: 28760318.
Article7. Eshghpour M, Nejat AH. 2013; Dry socket following surgical removal of impacted third molar in an Iranian population: incidence and risk factors. Niger J Clin Pract. 16:496–500. https://doi.org/10.4103/1119-3077.116897 . DOI: 10.4103/1119-3077.116897. PMID: 23974746.
Article8. Shin YS. 2019; How to improve the national health insurance fee-for-service schedule. Health Welf Policy Forum. 272:39–52.9. Kugelberg CF, Ahlström U, Ericson S, Hugoson A. 1985; Periodontal healing after impacted lower third molar surgery. A retrospective study. Int J Oral Surg. 14:29–40. https://doi.org/10.1016/s0300-9785(85)80007-7 . DOI: 10.1016/S0300-9785(85)80007-7. PMID: 3921477.
Article10. Moloney J, Stassen LF. 2009; Pericoronitis: treatment and a clinical dilemma. J Ir Dent Assoc. 55:190–2. PMID: 19753908.11. Chaves AJ, Nascimento LR, Costa ME, Franz-Montan M, Oliveira-Júnior PA, Groppo FC. 2008; Effects of surgical removal of mandibular third molar on the periodontium of the second molar. Int J Dent Hyg. 6:123–8. https://doi.org/10.1111/j.1601-5037.2008.00297.x . DOI: 10.1111/j.1601-5037.2008.00297.x. PMID: 18412725.
Article12. Khan M, Mehmboob B, Katpar S. 2014; Extraction of wisdom teeth under general anesthesia- a study. J Khyber Coll Dent. 5:20–4.13. Savanheimo N, Sundberg SA, Virtanen JI, Vehkalahti MM. 2012; Dental care and treatments provided under general anaesthesia in the Helsinki Public Dental Service. BMC Oral Health. 12:45. https://doi.org/10.1186/1472-6831-12-45 . DOI: 10.1186/1472-6831-12-45. PMID: 23102205. PMCID: PMC3553023.
Article14. Sigron GR, Pourmand PP, Mache B, Stadlinger B, Locher MC. 2014; The most common complications after wisdom-tooth removal: part 1: a retrospective study of 1,199 cases in the mandible. Swiss Dent J. 124:1042–6. 1052–6. PMID: 25342545.15. Cevidanes LH, Styner MA, Proffit WR. 2006; Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop. 129:611–8. https://doi.org/10.1016/j.ajodo.2005.12.008 . DOI: 10.1016/j.ajodo.2005.12.008. PMID: 16679201. PMCID: PMC3586191.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Modified difficult index adding extremely difficult for fully impacted mandibular third molar extraction
- Which factors are associated with difficult surgical extraction of impacted lower third molars?
- Orthodontic Traction of the Impacted Mandibular Third Molars to Replace Severely Resorbed Mandibular Second Molars
- Impacted mandibular third molars: a comparison of orthopantomography and cone-beam computed tomography imaging in predicting surgical difficulty
- A study of distribution, prevalence and relationship of the localized periodontitis of first and second molar root fusion