Increasing Incidence of B-Cell Non-Hodgkin Lymphoma and Occurrence of Second Primary Malignancies in South Korea: 10-Year Follow-up Using the Korean National Health Information Database
- Affiliations
-
- 1Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Janssen Research & Development, Global Epidemiology, Singapore
- 3Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
- 4Janssen Research & Development, Global Epidemiology, Titusville, NJ, USA
- 5Janssen Medical Affairs, Macquarie Park, Australia
- 6Department of Preventative Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2507951
- DOI: http://doi.org/10.4143/crt.2020.089
Abstract
- Purpose
The epidemiology of B-cell non-Hodgkin lymphoma (BNHL) in Asia is not well described, and rates of second primary malignancies (SPM) in these patients are not known. We aimed to describe temporal changes in BNHL epidemiology and SPM incidence in Korea.
Materials and Methods
A retrospective cohort study used claims data from the National Health Insurance Service that provides universal healthcare coverage in Korea. Newly diagnosed patients aged at least 19 years with a confirmed diagnosis of one of six BNHL subtypes (diffuse large cell B-cell lymphoma [DLBCL], small lymphocytic and chronic lymphocytic [CLL/SLL], follicular lymphoma [FL], mantle cell lymphoma [MCL], marginal zone lymphoma [MZL], and lymphoplasmacytic lymphoma/Waldenström’s macroglobulinemia [WM]) during the period 2006-2015 were enrolled and followed up until death, dis-enrolment, or study end, whichever occurred first. Patients with pre-existing primary cancers prior to the diagnosis of BNHL were excluded.
Results
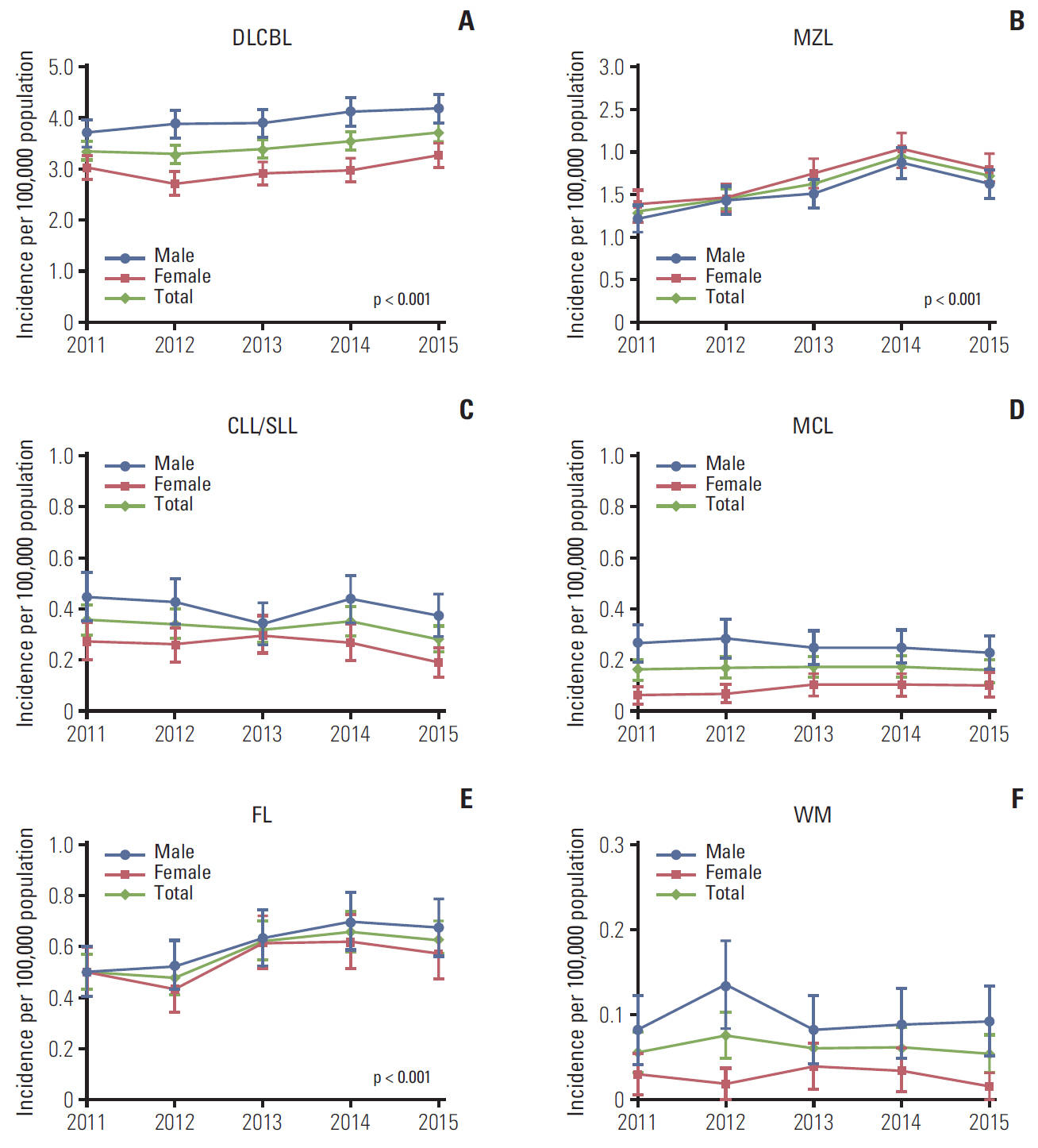
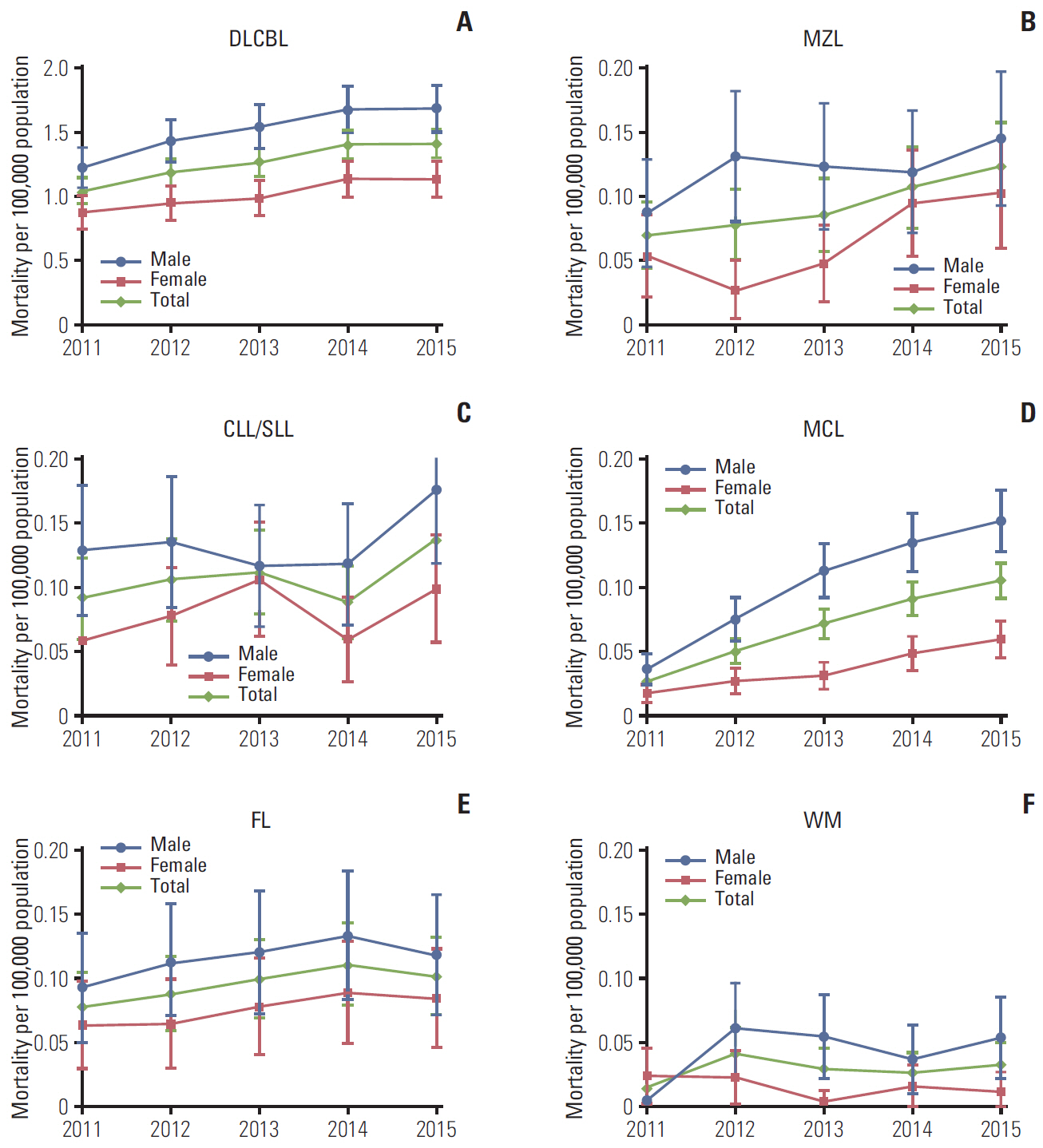
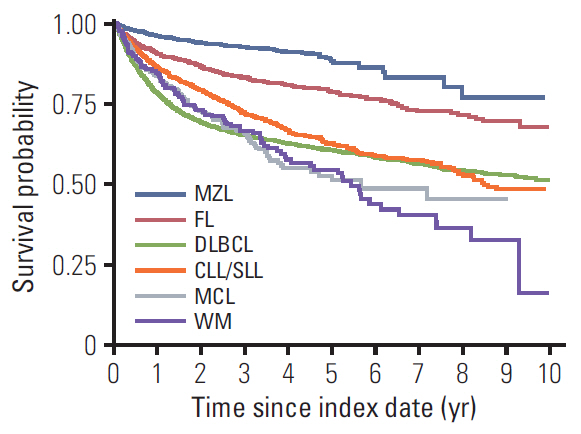
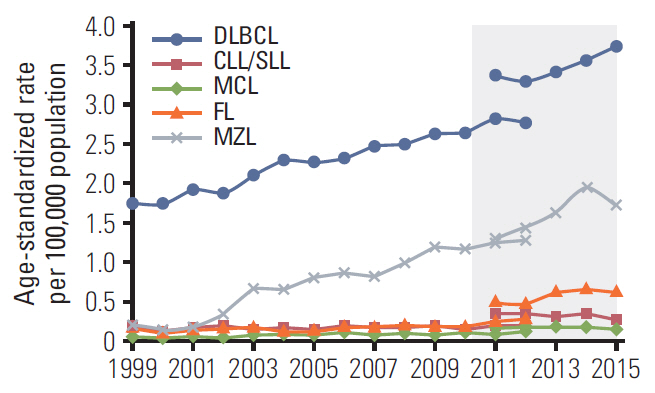
A total of 19,500 patients with newly diagnosed BNHL were identified out of 27,866 with non-Hodgkin lymphoma (NHL). DLBCL was the most frequently diagnosed subtype (41.9%-48.4% of NHL patients annually, 2011-2015). Standardized incidence of the six subtypes studied per 100,000 population increased from 5.74 in 2011 to 6.96 in 2015, with most increases in DLBCL, FL, and MZL. The incidence (95% confidence interval) of SPM per 100 person-years was 2.74 (2.26-3.29) for CLL/SLL, 2.43 (1.57-3.58) for MCL, 2.41 (2.10-2.76) for MZL, 2.23 (2.07-2.40) for DLBCL, 1.97 (1.61-2.38) for FL, and 1.41 (0.69-2.59) for WM.
Conclusion
BNHL has been increasingly diagnosed in Korea. High rates of SPM highlight the need for continued close monitoring to ensure early diagnosis and treatment.
Figure
Cited by 3 articles
-
Multicenter retrospective analysis of patients with chronic lymphocytic leukemia in Korea
Jun Ho Yi, Gyeong-Won Lee, Ji Hyun Lee, Kwai Han Yoo, Chul Won Jung, Dae Sik Kim, Jeong-Ok Lee, Hyeon Seok Eom, Ja Min Byun, Youngil Koh, Sung Soo Yoon, Jin Seok Kim, Jee Hyun Kong, Ho-Young Yhim, Deok-Hwan Yang, Dok Hyun Yoon, Do Hyoung Lim, Won-Sik Lee, Ho-Jin Shin
Blood Res. 2021;56(4):243-251. doi: 10.5045/br.2021.2021102.Upward trend in follicular lymphoma among the Korean population: 10-year experience at a large tertiary institution
Meejeong Kim, Hee Sang Hwang, Hyungwoo Cho, Dok Hyun Yoon, Cheolwon Suh, Chan Sik Park, Heounjeong Go, Jooryung Huh
J Pathol Transl Med. 2021;55(5):330-337. doi: 10.4132/jptm.2021.07.25.Treatment of indolent lymphoma
Seong Hyun Jeong
Blood Res. 2022;57(S1):120-129. doi: 10.5045/br.2022.2022054.
Reference
-
References
1. Armitage JO, Gascoyne RD, Lunning MA, Cavalli F. Non-Hodgkin lymphoma. Lancet. 2017; 390:298–310.
Article2. Lee H, Park HJ, Park EH, Ju HY, Oh CM, Kong HJ, et al. Nationwide statistical analysis of lymphoid malignancies in Korea. Cancer Res Treat. 2018; 50:222–38.
Article3. Morton LM, Slager SL, Cerhan JR, Wang SS, Vajdic CM, Skibola CF, et al. Etiologic heterogeneity among non-Hodgkin lymphoma subtypes: the InterLymph Non-Hodgkin Lymphoma Subtypes Project. J Natl Cancer Inst Monogr. 2014; 2014:130–44.4. Feugier P. A review of rituximab, the first anti-CD20 monoclonal antibody used in the treatment of B non-Hodgkin’s lymphomas. Future Oncol. 2015; 11:1327–42.
Article5. Pirani M, Marcheselli R, Marcheselli L, Bari A, Federico M, Sacchi S. Risk for second malignancies in non-Hodgkin’s lymphoma survivors: a meta-analysis. Ann Oncol. 2011; 22:1845–58.
Article6. Tward JD, Wendland MM, Shrieve DC, Szabo A, Gaffney DK. The risk of secondary malignancies over 30 years after the treatment of non-Hodgkin lymphoma. Cancer. 2006; 107:108–15.
Article7. Perry AM, Diebold J, Nathwani BN, MacLennan KA, Muller-Hermelink HK, Bast M, et al. Non-Hodgkin lymphoma in the developing world: review of 4539 cases from the International Non-Hodgkin Lymphoma Classification Project. Haematologica. 2016; 101:1244–50.
Article8. Yoon SO, Suh C, Lee DH, Chi HS, Park CJ, Jang SS, et al. Distribution of lymphoid neoplasms in the Republic of Korea: analysis of 5318 cases according to the World Health Organization classification. Am J Hematol. 2010; 85:760–4.
Article9. Chuang SS, Chen SW, Chang ST, Kuo YT. Lymphoma in Taiwan: review of 1347 neoplasms from a single institution according to the 2016 Revision of the World Health Organization Classification. J Formos Med Assoc. 2017; 116:620–5.
Article10. Bassig BA, Cerhan JR, Au WY, Kim HN, Sangrajrang S, Hu W, et al. Genetic susceptibility to diffuse large B-cell lymphoma in a pooled study of three Eastern Asian populations. Eur J Haematol. 2015; 95:442–8.
Article11. Cerhan JR, Slager SL. Familial predisposition and genetic risk factors for lymphoma. Blood. 2015; 126:2265–73.
Article12. Biagi JJ, Seymour JF. Insights into the molecular pathogenesis of follicular lymphoma arising from analysis of geographic variation. Blood. 2002; 99:4265–75.
Article13. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–28.
Article14. Seong SC, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.15. Moertel CG, Dockerty MB, Baggenstoss AH. Multiple primary malignant neoplasms. I. Introduction and presentation of data. Cancer. 1961; 14:221–30.16. LeMieux MH, Solanki AA, Mahmood U, Chmura SJ, Koshy M. Risk of second malignancies in patients with early-stage classical Hodgkin’s lymphoma treated in a modern era. Cancer Med. 2015; 4:513–8.
Article17. Engelhardt M, Ihorst G, Landgren O, Pantic M, Reinhardt H, Waldschmidt J, et al. Large registry analysis to accurately define second malignancy rates and risks in a well-characterized cohort of 744 consecutive multiple myeloma patients followed-up for 25 years. Haematologica. 2015; 100:1340–9.
Article18. Castillo JJ, Gertz MA. Secondary malignancies in patients with multiple myeloma, Waldenstrom macroglobulinemia and monoclonal gammopathy of undetermined significance. Leuk Lymphoma. 2017; 58:773–80.19. Giri S, Bhatt VR, Verma V, Pathak R, Bociek RG, Vose JM, et al. Risk of second primary malignancies in patients with follicular lymphoma: a United States population-based study. Clin Lymphoma Myeloma Leuk. 2017; 17:569–74.
Article20. Shah BK, Khanal A. Second primary malignancies in mantle cell lymphoma: a US population-based study. Anticancer Res. 2015; 35:3437–40.21. Tao L, Clarke CA, Rosenberg AS, Advani RH, Jonas BA, Flowers CR, et al. Subsequent primary malignancies after diffuse large B-cell lymphoma in the modern treatment era. Br J Haematol. 2017; 178:72–80.
Article22. Jung KW, Won YJ, Kong HJ, Lee ES; Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018; 50:303–16.
Article23. IACR International Association of Cancer Registries. Korea Central Cancer Registry profile page [Internet]. Lyon: IACR Official Website;2020. [cited 2018 Nov 1]. Available from: http://www.iacr.com.fr/index.php?option=com_comprofiler&task=userprofile&user=973&Itemid=498.24. Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 2010; 116:3724–34.
Article25. Ye X, Mahmud S, Skrabek P, Lix L, Johnston JB. Long-term time trends in incidence, survival and mortality of lymphomas by subtype among adults in Manitoba, Canada: a population-based study using cancer registry data. BMJ Open. 2017; 7:e015106.
Article26. Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006; 107:265–76.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three cases of primary non-Hodgkin's lymphoma of the pelvis
- Primary Malignant Lymphoma of The Bilateral Orbit
- Relationships among Hepatitis C Virus, Hepatocellular Carcinoma, and Diffuse Large B Cell Lymphoma: A Case Report
- A Case of Primary Non-Hodgkin's Lymphoma of the Ovary
- Primary Cutaneous T-cell/histiocyte-rich B-cell Lymphoma