Clin Endosc.
2020 Sep;53(5):594-599. 10.5946/ce.2019.175.
Endoscopic Ultrasound-Guided Random Omental Fine Needle Aspiration: A Novel Technique for the Diagnosis of Peritoneal Carcinomatosis
- Affiliations
-
- 1Department of Gastroenterology, Sri Balaji Action Medical Institute, New Delhi, India
- 2Department of Pathology, Action Cancer Hospital, New Delhi, India
- KMID: 2507594
- DOI: http://doi.org/10.5946/ce.2019.175
Abstract
- Background/Aims
Diagnostic abdominal paracentesis has been described in literature to have variable sensitivity of 50%–75% for the detection of peritoneal carcinomatosis (PC). We believe that random needle aspirates from the omentum, even in the absence of obvious deposits by endoscopic ultrasound (EUS), could prove malignancy in patients with PC.
Methods
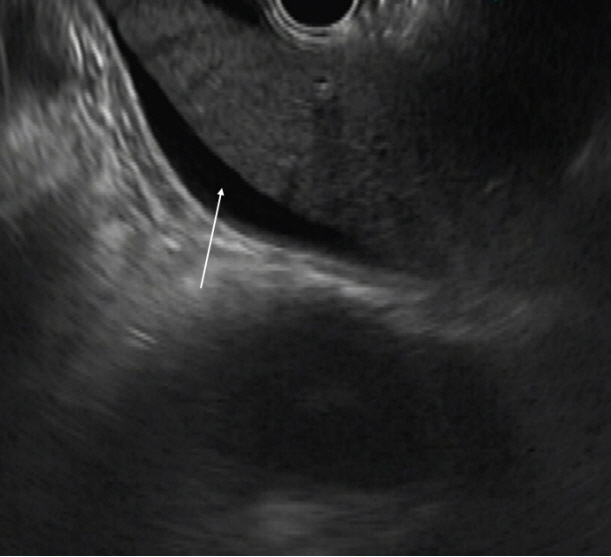
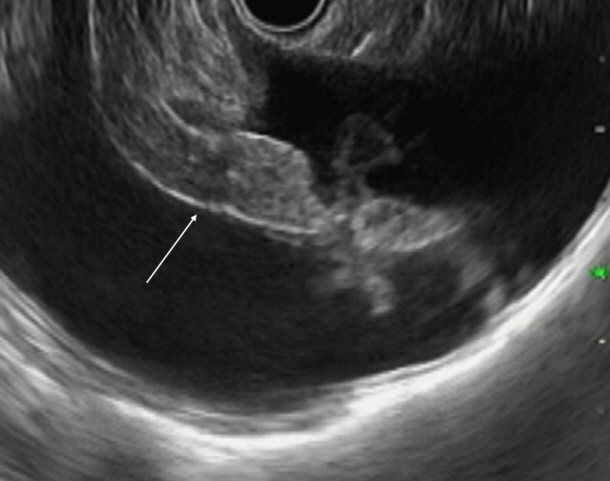
Consecutive patients who underwent EUS for diagnosis and staging of cancer and found to have ascites were included after obtaining informed consent. EUS-guided fine needle aspiration (EUS-FNA) from random sites in the omentum was performed through the transgastric route using a linear echoendoscope.
Results
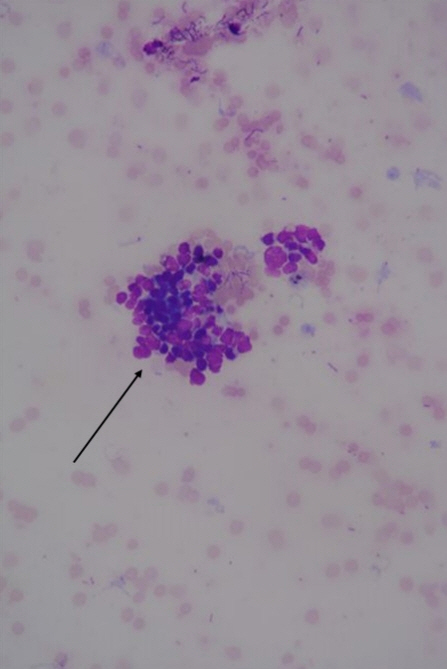
Fifty-four patients underwent EUS during October 2015 to April 2017 for detection, staging, or FNA of a suspected malignant lesion. Ascites was seen in 17 patients and 15 patients who fulfilled the criteria were included. The procedure was successful in all patients. Cytology was suggestive of malignancy in 12 (80%) but not suggestive of malignancy in 3 (20%) patients. Three patients who tested negative had hyperbilirubinemia with biliary obstruction. Their ascitic fluid analysis result was also negative.
Conclusions
Random FNA of the omentum in patients with malignancy-related ascites is highly effective in the diagnosis of PC and could be employed during EUS evaluation of malignancies.
Keyword
Figure
Reference
-
1. Allen VA, Takashima Y, Nayak S, Manahan KJ, Geisler JP. Assessment of false-negative ascites cytology in epithelial ovarian carcinoma: a study of 313 patients. Am J Clin Oncol. 2017; 40:175–177.2. Decker D, Stratmann H, Springer W, Schwering H, Varnai N, Bollmann R. Benign and malignant cells in effusions: diagnostic value of image DNA cytometry in comparison to cytological analysis. Pathol Res Pract. 1998; 194:791–795.
Article3. Kielhorn E, Schofield K, Rimm DL. Use of magnetic enrichment for detection of carcinoma cells in fluid specimens. Cancer. 2002; 94:205–211.
Article4. Rana SS, Bhasin DK, Srinivasan R, Singh K. Endoscopic ultrasound-guided fine needle aspiration of peritoneal nodules in patients with ascites of unknown cause. Endoscopy. 2011; 43:1010–1013.
Article5. Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992; 117:215–220.
Article6. Nguyen PT, Chang KJ. EUS in the detection of ascites and EUS-guided paracentesis. Gastrointest Endosc. 2001; 54:336–339.
Article7. Kaushik N, Khalid A, Brody D, McGrath K. EUS-guided paracentesis for the diagnosis of malignant ascites. Gastrointest Endosc. 2006; 64:908–913.
Article8. Peter S, Eltoum I, Eloubeidi MA. EUS-guided FNA of peritoneal carcinomatosis in patients with unknown primary malignancy. Gastrointest Endosc. 2009; 70:1266–1270.
Article9. Wardeh R, Lee JG, Gu M. Endoscopic ultrasound-guided paracentesis of ascitic fluid: a morphologic study with ultrasonographic correlation. Cancer Cytopathol. 2011; 119:27–36.10. Levy MJ, Abu Dayyeh BK, Fujii LL, et al. Detection of peritoneal carcinomatosis by EUS fine-needle aspiration: impact on staging and resectability (with videos). Gastrointest Endosc. 2015; 81:1215–1224.
Article11. DeWitt J, LeBlanc J, McHenry L, McGreevy K, Sherman S. Endoscopic ultrasound-guided fine-needle aspiration of ascites. Clin Gastroenterol Hepatol. 2007; 5:609–615.
Article12. Wani S, Coté GA, Keswani R, et al. Learning curves for EUS by using cumulative sum analysis: implications for American Society for Gastrointestinal Endoscopy recommendations for training. Gastrointest Endosc. 2013; 77:558–565.
Article13. Lee JY, Kim HS, Chung HH, Kim JW, Park NH, Song YS. The role of omentectomy and random peritoneal biopsies as part of comprehensive surgical staging in apparent early-stage epithelial ovarian cancer. Ann Surg Oncol. 2014; 21:2762–2766.
Article14. Franco D, Gigou M, Szekely AM, Bismuth H. Portal hypertension after bile duct obstruction: effect of bile diversion on portal pressure in the rat. Arch Surg. 1979; 114:1064–1067.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- Endoscopic Ultrasound-Fine Needle Aspiration versus Core Biopsy for the Diagnosis of Subepithelial Tumors
- A Case of Intra-abdominal Paragonimiasis Mimicking Metastasis of Lung Cancer Diagnosed by Endoscopic Ultrasound-guided Fine Needle Aspiration
- How to optimize the diagnostic yield of endoscopic ultrasoundguided fine-needle sampling in solid pancreatic lesions from a technical perspective
- How Can We Get the Best Results with Endoscopic Ultrasound-Guided Fine Needle Aspiration?