J Korean Med Sci.
2020 Sep;35(38):e315. 10.3346/jkms.2020.35.e315.
Recent Trends in Transurethral Surgeries and Urological Outpatient Procedures: a Nationwide Populationbased Cohort Study
- Affiliations
-
- 1Department of Urology, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea
- 2Department of Urology, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- KMID: 2507080
- DOI: http://doi.org/10.3346/jkms.2020.35.e315
Abstract
- Background
Demographic change and advances in technology affect transurethral surgery and outpatient procedures in the urologic field. There are few population-based studies that accurately assess the trend of transurethral surgery and outpatient procedures including diagnostic tests. We investigated the recent epidemiologic trends in transurethral surgeries and urological outpatient procedures from 2009 to 2016 in Korea using the entire populationbased cohort.
Methods
We analyzed medical service claim data of transurethral surgery, urological outpatient procedures submitted by medical service providers from the Health Insurance Review and Assessment Service from 2009 to 2016.
Results
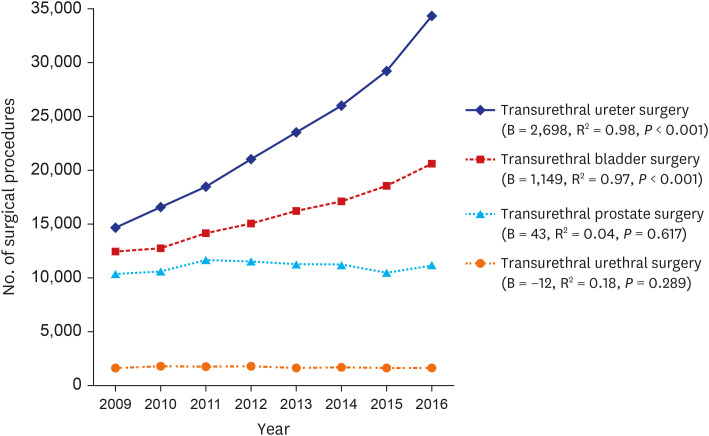
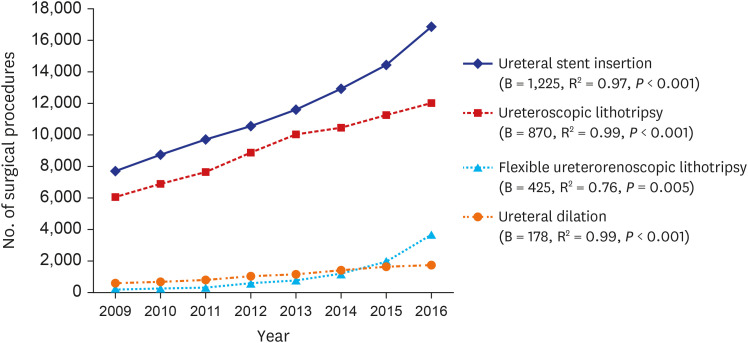
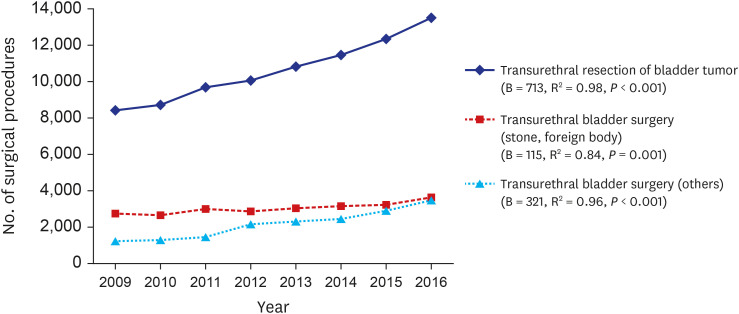
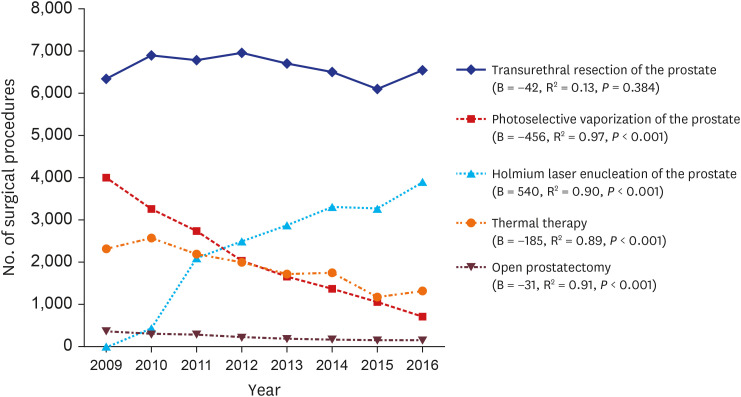
Transurethral ureter surgery increased by 134.9% from 14,635 in 2009 to 34,382 in 2016 (B = 2,698; R 2 = 0.98; P < 0.001). The transurethral bladder surgery increased by 65.5% from 12,482 in 2009 to 20,658 in 2016 (B = 1,149; R 2 = 0.97; P < 0.001). Over the 8-years period, there were not significant changes in transurethral prostate (B = 43; R 2 = 0.04; P = 0.617) and urethral surgery (B = −12; R 2 = 0.18; P = 0.289). The significantly increasing trends in cystoscopy (B = 5,260; R 2 = 0.95; P < 0.001) and uroflowmetry (B = 53,942; R2 = 0.99; P < 0.001) were observed during the 8-year period. There was no difference in bladder catheterization during the 8-year period. Urodynamic study (UDS: B = −2,156; R 2 = 0.77; P = 0.003) and electrical stimulation treatment (EST: B = −1,034; R 2= 0.87; P < 0.001) significantly decreased.
Conclusion
In Korea, transurethral ureter surgery and transurethral bladder surgery have been continuously increasing. Transurethral prostate surgery and transurethral urethral surgery remained constant with no increase or decrease. Cystoscopy and uroflowmetry continue to increase, while UDS and EST continue to decrease.
Keyword
Figure
Reference
-
1. Patel RM, Bariol S. National trends in surgical therapy for benign prostatic hyperplasia in Australia. ANZ J Surg. 2019; 89(4):345–349. PMID: 30706655.
Article2. Welliver C, Feinstein L, Ward JB, Fwu CW, Kirkali Z, Bavendam T, et al. Trends in lower urinary tract symptoms associated with benign prostatic hyperplasia, 2004 to 2013: the Urologic Diseases in America Project. J Urol. 2020; 203(1):171–178. PMID: 31430232.
Article3. Kim JK, Cho YS, Park SY, Joo KJ, Min SK, Lee YG, et al. Recent surgical treatments for urinary stone disease in a Korean population: national population-based study. Int J Urol. 2019; 26(5):558–564. PMID: 30803067.
Article4. Jeon BJ, Chung H, Bae JH, Jung H, Lee JG, Choi H. Analysis of present status for surgery of benign prostatic hyperplasia in Korea using nationwide healthcare system data. Int Neurourol J. 2019; 23(1):22–29. PMID: 30943691.
Article5. Park J, Lee YJ, Lee JW, Yoo TK, Chung JI, Yun SJ, et al. Comparative analysis of benign prostatic hyperplasia management by urologists and nonurologists: a Korean nationwide health insurance database study. Korean J Urol. 2015; 56(3):233–239. PMID: 25763128.
Article6. Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998; 33(1):17–21. PMID: 9471036.
Article7. Lee SH, Kang JS, Kim JW, Lee SJ. Incontinence pad usage in medical welfare facilities in Korea. Int Neurourol J. 2013; 17(4):186–190. PMID: 24466466.
Article8. McDonnell J, Busschbach JJ, Kok E, van Exel J, Stolk E, Koopmanschap M, et al. Lower urinary tract symptoms suggestive of benign prostatic obstruction--Triumph: health-economical analysis. Eur Urol. 2001; 39 Suppl 3:37–41.9. Al-Husseini MJ, Kunbaz A, Saad AM, Santos JV, Salahia S, Iqbal M, et al. Trends in the incidence and mortality of transitional cell carcinoma of the bladder for the last four decades in the USA: a SEER-based analysis. BMC Cancer. 2019; 19(1):46. PMID: 30630456.
Article10. Abdollah F, Gandaglia G, Thuret R, Schmitges J, Tian Z, Jeldres C, et al. Incidence, survival and mortality rates of stage-specific bladder cancer in United States: a trend analysis. Cancer Epidemiol. 2013; 37(3):219–225. PMID: 23485480.
Article11. Song W, Jeon HG. Incidence of kidney, bladder, and prostate cancers in Korea: an update. Korean J Urol. 2015; 56(6):422–428. PMID: 26078838.
Article12. Gilling PJ, Wilson LC, King CJ, Westenberg AM, Frampton CM, Fraundorfer MR. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. 2012; 109(3):408–411. PMID: 21883820.
Article13. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU Guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67(6):1099–1109. PMID: 25613154.
Article14. de la Rosette JJ, Hubregtse MR, Karthaus HF, Debruyne FM. Results of a questionnaire among Dutch urologists and general practitioners concerning diagnostics and treatment of patients with prostatitis syndromes. Eur Urol. 1992; 22(1):14–19. PMID: 1425844.
Article15. Ku JH, Paick JS, Kim SW. Factors influencing practices for chronic prostatitis: a nationwide survey of urologists in South Korea. Int J Urol. 2005; 12(11):976–983. PMID: 16351654.
Article16. Reynolds WS, Dmochowski RR, Lai J, Saigal C, Penson DF. Urologic Diseases in America Project. Patterns and predictors of urodynamics use in the United States. J Urol. 2013; 189(5):1791–1796. PMID: 23159270.
Article17. Choi JB, Han KD, Ha US, Hong SH. Efficacy and safety of incontinence surgery according to the surgeon's specialty and performance of a preoperative urodynamic study. Int Neurourol J. 2018; 22(4):305–312. PMID: 30599502.
Article18. Ohlsson BL. Effects of some different pulse parameters on the perception of intravaginal and intra-anal electrical stimulation. Med Biol Eng Comput. 1988; 26(5):503–508. PMID: 3267193.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Exploring National Trends in Bladder-Related Urological Procedures: A Nationwide Population-Based Cohort Study
- Analysis of Trends of 3 Major Benign Prostatic Hyperplasia Surgery in the Last 5 Years
- Laparoscopic Surgery for Colorectal Cancer in Korea: Nationwide Data from 2008~2013
- Analysis of Present Status for Surgery of Benign Prostatic Hyperplasia in Korea Using Nationwide Healthcare System Data
- Life-Sustaining Procedures, Palliative Care, and Cost Trends in Dying COPD Patients in U.S. Hospitals: 2005~2014