J Cerebrovasc Endovasc Neurosurg.
2020 Sep;22(3):176-181. 10.7461/jcen.2020.22.3.176.
Clinical challenges associated with the endovascular treatment of acute stroke in a patient with infective endocarditis
- Affiliations
-
- 1Department of Radiology, Hacettepe University Faculty of Medicine, Ankara, Turkey
- 2Department of Neurology, Hacettepe University Faculty of Medicine, Ankara, Turkey
- 3Department of Cardiovascular Surgery, Hacettepe University Faculty of Medicine, Ankara, Turkey
- KMID: 2506764
- DOI: http://doi.org/10.7461/jcen.2020.22.3.176
Abstract
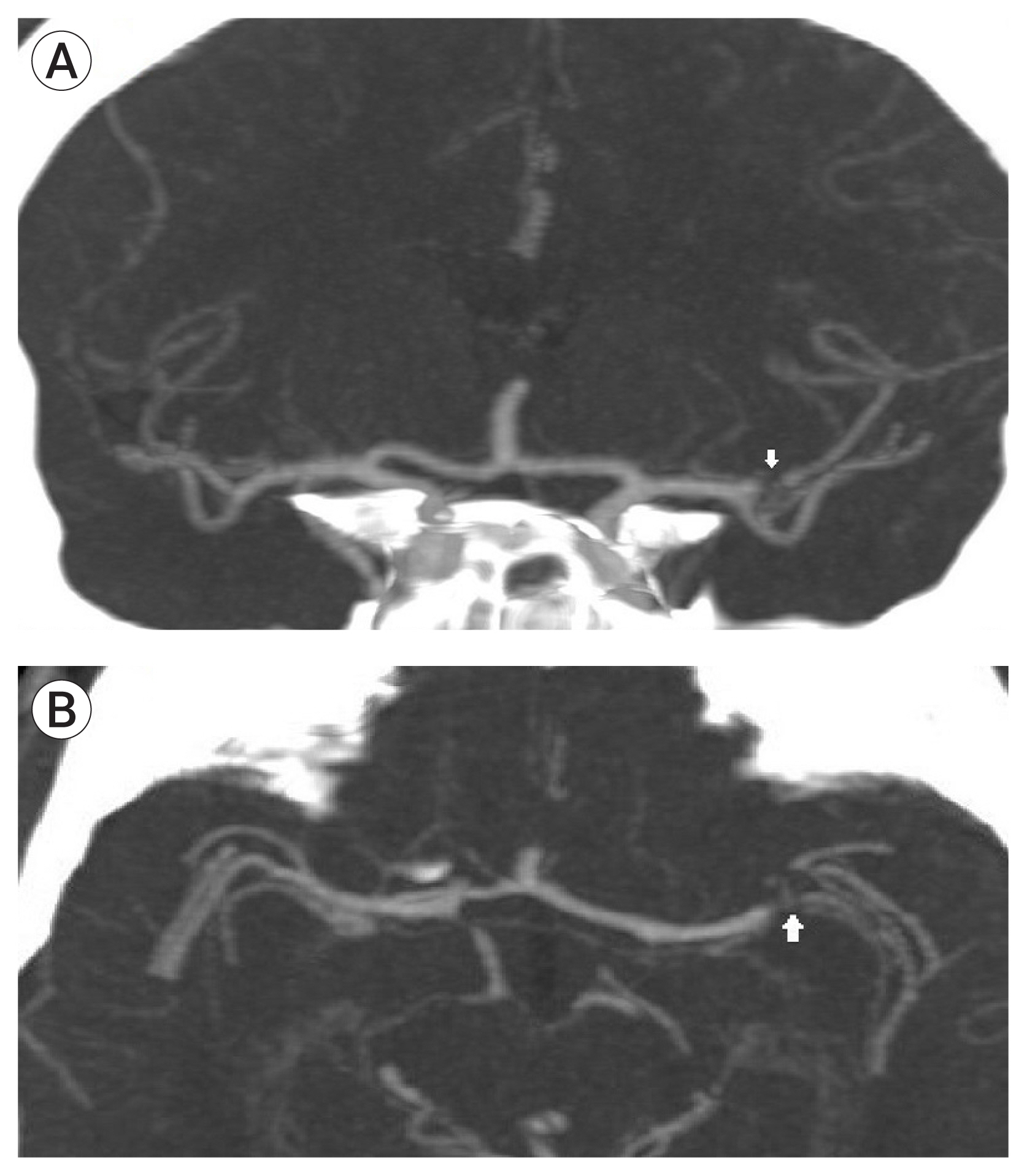
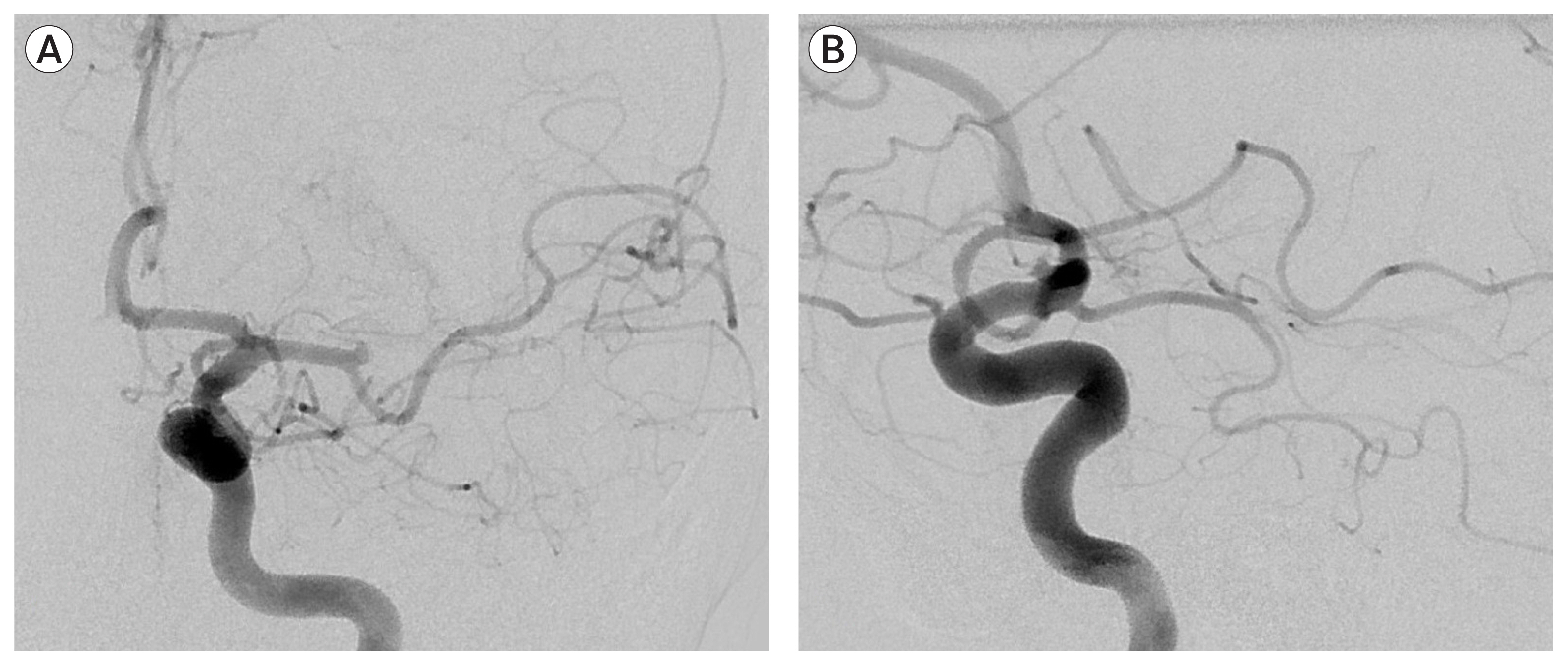
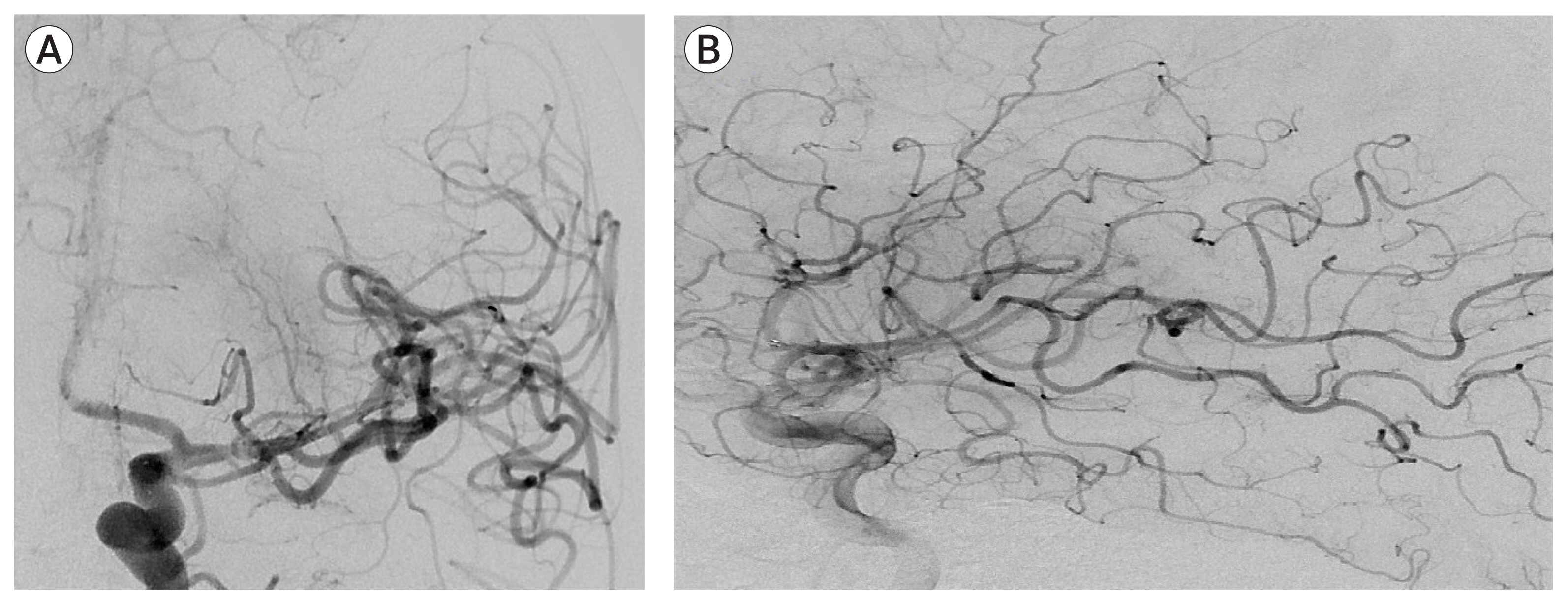
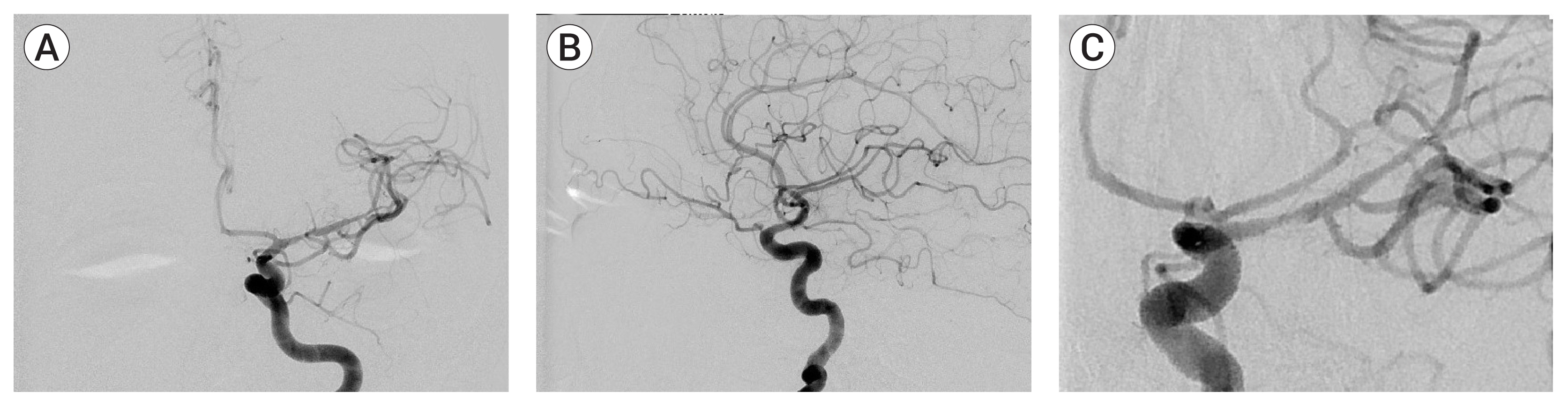
- Although stroke is common in infective endocarditis (IE), only 26 cases of thrombectomy have been reported to date for IE-related acute stroke. We report a 40-year-old man who presented with left middle cerebral artery occlusion of unknown cause. Multiple attempts of mechanical aspiration thrombectomy and stentrievers failed to recanalize the artery. Effective revascularization was eventually achieved by placing a self-expanding intracranial stent. Post-procedurally the patient was diagnosed with IE with mitral valve insufficiency, mandating emergent valvular replacement while the patient was still on tirofiban infusion. On follow-up, the patient had a modified Rankin’s score of 0, had no recurrent stroke, and the intracranial stent remained patent yet stenosed. Based on the use of a self-expanding intracranial stent in the setting of IE, we discuss the consequences of the fibrotic and inflammatory content of the embolus and the associated high risk of intracranial hemorrhage which complicates clinical decision making.
Figure
Reference
-
1. Ambrosioni J, Urra X, Hernandez-Meneses M, Almela M, Falces C, Tellez A, et al. Mechanical Thrombectomy for Acute Ischemic Stroke Secondary to Infective Endocarditis. Clin Infect Dis. 2018; Apr. 66(8):1286–9.
Article2. Bain MD, Hussain MS, Gonugunta V, Katzan I, Gupta R. Successful recanalization of a septic embolus with a balloon mounted stent after failed mechanical thrombectomy. J Neuroimaging. 2011; Apr. 21(2):170–2.
Article3. Bhuva P, Kuo SH, Claude Hemphill J, Lopez GA. Intracranial hemorrhage following thrombolytic use for stroke caused by infective endocarditis. Neurocrit Care. 2010; Feb. 12(1):79–82.
Article4. Bukow SC, Daffertshofer M, Hennerici MG. Tirofiban for the treatment of ischaemic stroke. Expert Opin Pharmacother. 2006; Jan. 7(1):73–9.
Article5. Hernandez-Fernandez F, Rojas-Bartolome L, Garcia-Garcia J, Ayo-Martin O, Molina-Nuevo JD, Barbella-Aponte RA, et al. Histopathological and bacteriological analysis of thrombus material extracted during mechanical thrombectomy in acute stroke patients. Cardiovasc Intervent Radiol. 2017; Dec. 40(12):1851–60.
Article6. Junna M, Lin CC, Espinosa RE, Rabinstein AA. Successful intravenous thrombolysis in ischemic stroke caused by infective endocarditis. Neurocrit Care. 2007; 6(2):117–20.
Article7. Kellert L, Hametner C, Rohde S, Bendszus M, Hacke W, Ringleb P, et al. Endovascular stroke therapy: tirofiban is associated with risk of fatal intracerebral hemorrhage and poor outcome. Stroke. 2013; May. 44(5):1453–5.
Article8. Kim JM, Jeon JS, Kim YW, Kang DH, Hwang YH, Kim YS. Forced arterial suction thrombectomy of septic embolic middle cerebral artery occlusion due to infective endocarditis: an illustrative case and review of the literature. Neurointervention. 2014; Sep. 9(2):101–5.
Article9. Ladner TR, Davis BJ, He L, Kirshner HS, Froehler MT, Mocco J. Complex decision-making in stroke: preoperative mechanical thrombectomy of septic embolus for emergency cardiac valve surgery. J Neurointerv Surg. 2015; Dec. 7(12):e41.
Article10. Scharf EL, Chakraborty T, Rabinstein A, Miranpuri AS. Endovascular management of cerebral septic embolism: three recent cases and review of the literature. J Neurointerv Surg. 2017; May. 9(5):463–5.
Article11. Sloane KL, Raymond SB, Rabinov JD, Singhal AB. Mechanical thrombectomy in stroke from infective endocarditis: case report and review. J Stroke Cerebrovasc Dis. 2019; Jan. 29(1):104501.
Article12. Sveinsson O, Herrman L, Holmin S. Intra-arterial mechanical thrombectomy: an effective treatment for ischemic stroke caused by endocarditis. Case Rep Neurol. 2016; Oct. 8(3):229–33.
Article13. Walker KA, Sampson JB, Skalabrin EJ, Majersik JJ. Clinical characteristics and thrombolytic outcomes of infective endocarditis-associated stroke. Neurohospitalist. 2012; Jul. 2(3):87–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of Mechanical Embolectomy for Septic Embolus in the Cerebral Artery Complicated with Infective Endocarditis
- A case of Libman-Sacks endocarditis confused with infective endocarditis
- Forced Arterial Suction Thrombectomy of Septic Embolic Middle Cerebral Artery Occlusion Due to Infective Endocarditis: an Illustrative Case and Review of the Literature
- A Case of Infective Endocarditis Complicated with Multiple Myocotic Aneurysm and Mitral Valve Perforation
- Multiple Embolic Infarcts Caused by Infective Endocarditis Associated with Atrioesophageal Fistula after Percutaneous Radiofrequency Catheter Ablation for Atrial Fibrillation