J Korean Med Sci.
2020 Sep;35(36):e294. 10.3346/jkms.2020.35.e294.
Trends of Incidence and Survival Rates of Mucosa-associated Lymphoid Tissue Lymphoma in the Korean Population: Analysis of the Korea Central Cancer Registry Database
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Catholic Kwandong University International St. Mary's Hospital, Incheon, Korea
- 2Division of Hematology and Oncology, Yonsei University Wonju College of Medicine, Wonju, Korea
- 3Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2506538
- DOI: http://doi.org/10.3346/jkms.2020.35.e294
Abstract
- Background
Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT-lymphoma) is an extranodal lymphoma that occurs at various sites in the body. There is a limited understanding of the incidence and survival rates of MALTlymphoma. To investigate the nation-wide incidence and survival rates of MALT-lymphoma in Korea during 1999–2017, the data on MALT-lymphoma were retrieved from the Korea Central Cancer Registry.
Methods
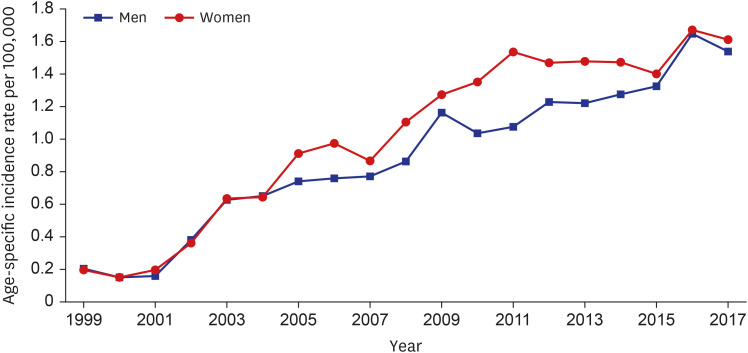
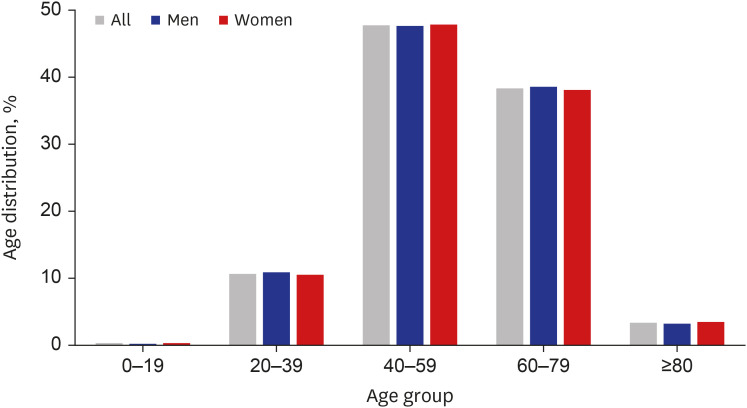
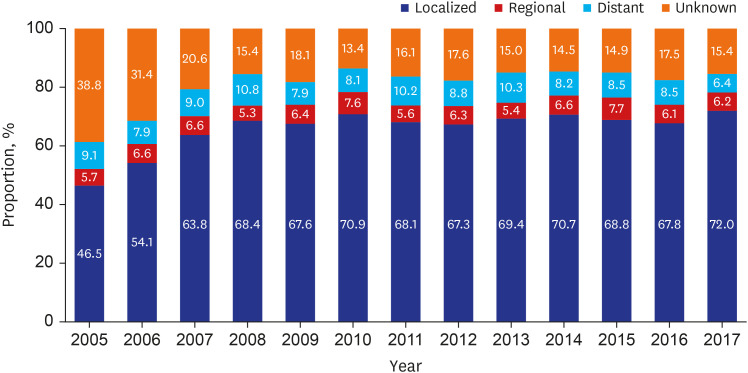
During the time period of 1999–2017, 11,128 patients were diagnosed with MALTlymphoma. The age and sex of the patients and the Surveillance, Epidemiology, and End Results (SEER) summary stage of the tumor were analyzed, and the relative survival rates (RSRs) were calculated.
Results
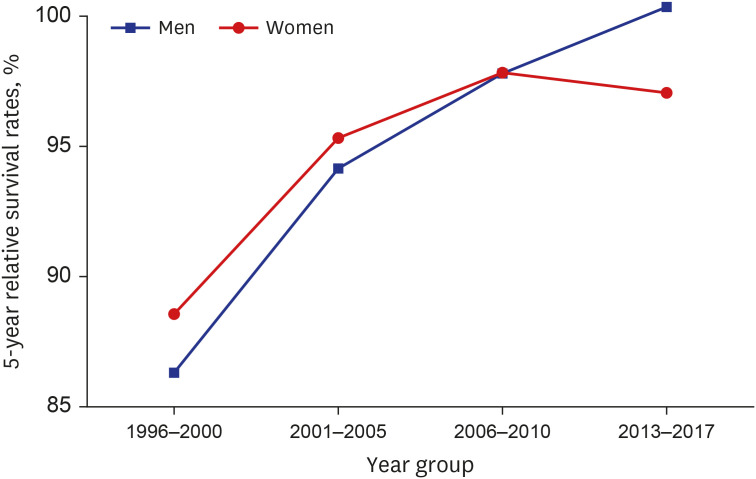
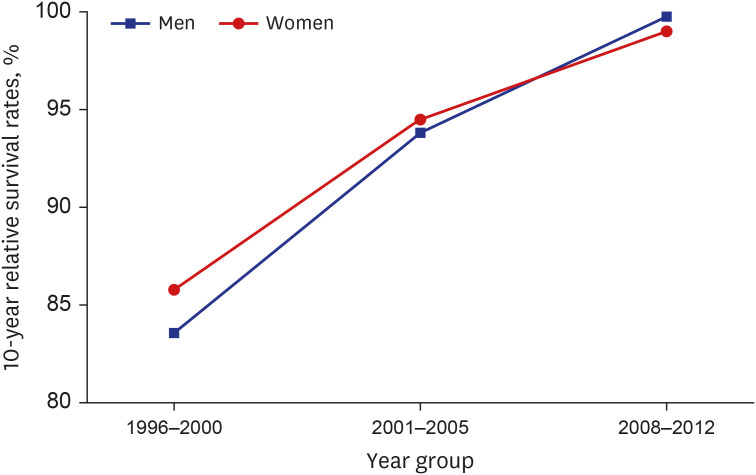
The age-standardized incidence rates of MALT-lymphoma in 2017 among males and females were 1.53 and 1.61 per 100,000 individuals, respectively, whereas those in 1999 among males and females were 0.21 and 0.20, respectively in Korea. The RSRs were more than 97% at 10 years post-diagnosis between 1993 and 2017. The 5-year RSRs were 87.4%, 94.8%, 97.8%, and 98.6% during 1996–2000, 2001–2005, 2006–2010, and 2013–2017, respectively. Based on SEER summary staging, the 5-year RSRs during 2013–2017 were 100.3%, 90.8%, 91.3%, and 97.9% for patients with localized, regional, distant, and unknown stages of MALT-lymphoma, respectively.
Conclusion
Although the incidence of MALT-lymphoma is low in Korea, it has been increasing in recent years. The prognosis of MALT-lymphoma is good even at advanced stages. These findings provide useful insights to clinicians about MALT-lymphoma and inform patients about the survival rate.
Keyword
Figure
Reference
-
1. Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983; 52(8):1410–1416. PMID: 6193858.
Article2. Zucca E, Cavalli F. Extranodal lymphomas. Ann Oncol. 2000; 11 Suppl 3:219–222. PMID: 11079144.
Article3. Brandtzaeg P, Farstad IN, Haraldsen G. Regional specialization in the mucosal immune system: primed cells do not always home along the same track. Immunol Today. 1999; 20(6):267–277. PMID: 10354552.
Article4. Isaacson PG. Extranodal lymphomas: the MALT concept. Verh Dtsch Ges Pathol. 1992; 76:14–23. PMID: 1283245.5. Suarez F, Lortholary O, Hermine O, Lecuit M. Infection-associated lymphomas derived from marginal zone B cells: a model of antigen-driven lymphoproliferation. Blood. 2006; 107(8):3034–3044. PMID: 16397126.
Article6. Bende RJ, van Maldegem F, van Noesel CJ. Chronic inflammatory disease, lymphoid tissue neogenesis and extranodal marginal zone B-cell lymphomas. Haematologica. 2009; 94(8):1109–1123. PMID: 19608670.
Article7. Wotherspoon AC, Doglioni C, Diss TC, Pan L, Moschini A, de Boni M, et al. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993; 342(8871):575–577. PMID: 8102719.8. Khalil MO, Morton LM, Devesa SS, Check DP, Curtis RE, Weisenburger DD, et al. Incidence of marginal zone lymphoma in the United States, 2001–2009 with a focus on primary anatomic site. Br J Haematol. 2014; 165(1):67–77. PMID: 24417667.
Article9. Zucca E, Bertoni F, Vannata B, Cavalli F. Emerging role of infectious etiologies in the pathogenesis of marginal zone B-cell lymphomas. Clin Cancer Res. 2014; 20(20):5207–5216. PMID: 25320370.
Article10. Thieblemont C, Berger F, Dumontet C, Moullet I, Bouafia F, Felman P, et al. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed. Blood. 2000; 95(3):802–806. PMID: 10648389.
Article11. Armitage JO, Weisenburger DD. New approach to classifying non-Hodgkin's lymphomas: clinical features of the major histologic subtypes. Non-Hodgkin's Lymphoma Classification Project. J Clin Oncol. 1998; 16(8):2780–2795. PMID: 9704731.
Article12. Hwang YC, Kim TY, Kim WB, Shong YK, Yi KH, Shong M, et al. Clinical characteristics of primary thyroid lymphoma in Koreans. Endocr J. 2009; 56(3):399–405. PMID: 19225216.
Article13. Wu XC, Andrews P, Chen VW, Groves FD. Incidence of extranodal non-Hodgkin lymphomas among whites, blacks, and Asians/Pacific Islanders in the United States: anatomic site and histology differences. Cancer Epidemiol. 2009; 33(5):337–346. PMID: 19853554.
Article14. Luminari S, Cesaretti M, Marcheselli L, Rashid I, Madrigali S, Maiorana A, et al. Decreasing incidence of gastric MALT lymphomas in the era of anti-Helicobacter pylori interventions: results from a population-based study on extranodal marginal zone lymphomas. Ann Oncol. 2010; 21(4):855–859. PMID: 19850642.15. Rasmussen P, Ralfkiaer E, Prause JU, Sjö LD, Siersma VD, Heegaard S. Malignant lymphoma of the lacrimal gland: a nation-based study. Arch Ophthalmol. 2011; 129(10):1275–1280. PMID: 21987669.16. Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999~2001; first result using the national cancer incidence database. Cancer Res Treat. 2005; 37(6):325–331. PMID: 19956367.
Article17. World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th rev. ed. Geneva, Switzerland: World Health Organization;1994.18. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52(2):335–350. PMID: 32178489.
Article19. Bray F, Ferlay J. Chapter 7: Age standardization. In : Forman D, Bray F, Brewster DH, Gombe Mbalawa C, Kohler B, Piñeros M, editors. IARC Scientific Publications No. 167. Cancer Incidence in Five Continents, Vol. X. Lyon, France: International Agency for Research on Cancer;2014. p. 112–115.20. Ederer F, Heise H. Instructions to IBM 650 Programmers in Processing Survival Computations. Methodological Note No. 10. End Results Evaluation Section. Bethesda, MD: National Cancer Institute;1959.21. Bassig BA, Au WY, Mang O, Ngan R, Morton LM, Ip DK, et al. Subtype-specific incidence rates of lymphoid malignancies in Hong Kong compared to the United States, 2001–2010. Cancer Epidemiol. 2016; 42:15–23. PMID: 26991956.
Article22. Chihara D, Ito H, Matsuda T, Shibata A, Katsumi A, Nakamura S, et al. Differences in incidence and trends of haematological malignancies in Japan and the United States. Br J Haematol. 2014; 164(4):536–545. PMID: 24245986.23. Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 2010; 116(19):3724–3734. PMID: 20664057.
Article24. Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, et al. SEER cancer statistics review, 1975–2013. Updated 2015. Accessed April 1, 2016. http://seer.cancer.gov/csr/1975_2013/.25. Lee H, Park HJ, Park EH, Ju HY, Oh CM, Kong HJ, et al. Nationwide statistical analysis of lymphoid malignancies in Korea. Cancer Res Treat. 2018; 50(1):222–238. PMID: 28361523.
Article26. Thieblemont C, Cascione L, Conconi A, Kiesewetter B, Raderer M, Gaidano G, et al. A MALT lymphoma prognostic index. Blood. 2017; 130(12):1409–1417. PMID: 28720586.
Article27. Thieblemont C, Bastion Y, Berger F, Rieux C, Salles G, Dumontet C, et al. Mucosa-associated lymphoid tissue gastrointestinal and nongastrointestinal lymphoma behavior: analysis of 108 patients. J Clin Oncol. 1997; 15(4):1624–1630. PMID: 9193362.
Article28. Zucca E, Conconi A, Pedrinis E, Cortelazzo S, Motta T, Gospodarowicz MK, et al. Nongastric marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Blood. 2003; 101(7):2489–2495. PMID: 12456507.
Article29. Papaxoinis G, Fountzilas G, Rontogianni D, Dimopoulos MA, Pavlidis N, Tsatalas C, et al. Low-grade mucosa-associated lymphoid tissue lymphoma: a retrospective analysis of 97 patients by the Hellenic Cooperative Oncology Group (HeCOG). Ann Oncol. 2008; 19(4):780–786. PMID: 18156143.
Article30. Arcaini L, Burcheri S, Rossi A, Passamonti F, Paulli M, Boveri E, et al. Nongastric marginal-zone B-cell MALT lymphoma: prognostic value of disease dissemination. Oncologist. 2006; 11(3):285–291. PMID: 16549813.
Article31. Pinotti G, Zucca E, Roggero E, Pascarella A, Bertoni F, Savio A, et al. Clinical features, treatment and outcome in a series of 93 patients with low-grade gastric MALT lymphoma. Leuk Lymphoma. 1997; 26(5-6):527–537. PMID: 9389360.
Article32. Kiesewetter B, Lukas J, Dolak W, Simonitsch-Klupp I, Mayerhoefer ME, Raderer M. Gender aspects in extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue: does sex matter? Oncology. 2016; 91(5):243–250. PMID: 27548082.
Article33. Ko YH, Kim CW, Park CS, Jang HK, Lee SS, Kim SH, et al. REAL classification of malignant lymphomas in the Republic of Korea: incidence of recently recognized entities and changes in clinicopathologic features. Hematolymphoreticular Study Group of the Korean Society of Pathologists. Revised European-American lymphoma. Cancer. 1998; 83(4):806–812. PMID: 9708949.34. Alderuccio JP, Zhao W, Desai A, Ramdial J, Gallastegui N, Kimble E, et al. Short survival and frequent transformation in extranodal marginal zone lymphoma with multiple mucosal sites presentation. Am J Hematol. 2019; 94(5):585–596. PMID: 30784098.
Article35. Oh SY, Suh C. Non-gastric marginal zone B-cell lymphoma in Korea: clinical features, treatment, and prognostic factors. Korean J Intern Med. 2010; 25(3):227–236. PMID: 20830217.
Article36. Nakamura S, Matsumoto T, Iida M, Yao T, Tsuneyoshi M. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer. 2003; 97(10):2462–2473. PMID: 12733145.37. Kim SW, Lim DH, Ahn YC, Kim WS, Kim SJ, Ko YH, et al. Clinical outcomes of radiation therapy for early-stage gastric mucosa-associated lymphoid tissue lymphoma. World J Gastroenterol. 2013; 19(36):6062–6068. PMID: 24106407.
Article38. Chung SJ, Kim JS, Kim H, Kim SG, Kim CW, Jung HC, et al. Long-term clinical outcome of Helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphoma is comparable to that of h. pylori-positive lymphoma. J Clin Gastroenterol. 2009; 43(4):312–317. PMID: 18936712.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nationwide Statistical Analysis of Lymphoid Malignancies in Korea
- A case report of the Pulmonary Malignant Lymphomaof the mucosa-associated lymphoid tissue(MALT)
- Mucosa-Associated Lymphoid Tissue Lymphoma of the Esophagus Coexistent with Bronchus-Associated Lymphoid Tissue Lymphoma of the Lung
- Annual report of gynecologic cancer registry program in Korea: 1991~2004
- Two Cases of Bone Marrow Permeated Primary Gastric Mucosa-Associated Lymphoid Tissue Lymphoma