Obstet Gynecol Sci.
2020 Sep;63(5):660-669. 10.5468/ogs.20063.
Effects of high-frequency, high-intensity transcutaneous electrical nerve stimulation versus intravenous opioids for pain relief after hysteroscopy: a randomized controlled study
- Affiliations
-
- 1Department of Anesthesiology and Intensive Care Medicine, Sahlgrenska University Hospital/Östra, Gothenburg, Sweden
- 2Department of Anesthesiology and Intensive Care Medicine, Institute of Clinical Sciences at the Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
- 3Multidisciplinary Pain Center Kungälv Hospital Kungälv and Institute of Medicine, Sahlgrenska Academy at the University of Gothenburg, Sahlgrenska University Hospital, Gothenburg, Sweden
- 4Department of Anaesthesiology and Intensive Care Medicine/Paincenter, Sahlgrenska University Hospital/Östra, Gothenburg, Sweden
- KMID: 2506509
- DOI: http://doi.org/10.5468/ogs.20063
Abstract
Objective
To compare the time spent in the Post-Anesthesia Care Unit (PACU) and the pain-relieving effects of treatment with high-frequency, high-intensity transcutaneous electrical nerve stimulation (TENS) or intravenous (IV) opioids after hysteroscopy.
Methods
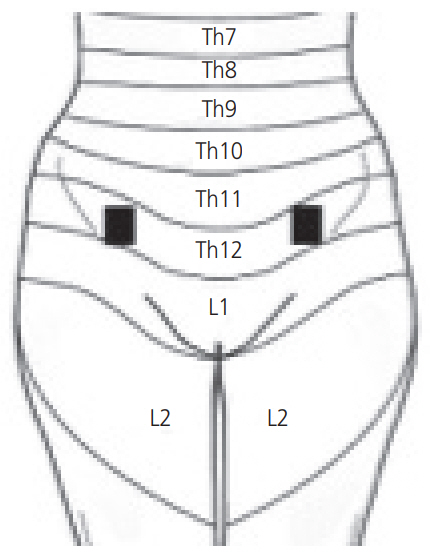
All patients who postoperatively reported a visual analogue scale (VAS) pain score of ≥3 were included in the study. TENS treatment was given with a stimulus intensity between 40 and 60 mA for 1 minute and repeated once if there was insufficient pain relief. In the opioid group, a fractionated dose of 5 mg morphine was administered. If the patient reported insufficient pain relief after the assigned treatment, the patient was reassigned to the other treatment group.
Results
Seventy-four women were randomized to TENS (n=38) or IV opioids (n=36) for treatment. Both groups reported significant pain relief after discharge from the PACU, with a decrease of VAS scores from 5.6 to 1.4 in the TENS group (P<0.001) and 5.1 to 1.3 in the opioid group (P<0.001). There were no significant differences between the groups. When only the responders in both groups, i.e., patients with VAS scores of <3 on respectively assigned treatments, were compared, the TENS responders (n=22) were found to have spent a significantly shorter time in the PACU (91 vs. 69 minutes, P=0.013) compared to the opioid responders (n=20).
Conclusion
Using TENS as first line of pain relief may reduce the need for postoperative opioids. In addition, TENS appears preferable as the first line of treatment due to its association with a shorter time spent in the PACU if the patient responds to the treatment. Trial Registration Västra Götalandsregionen Identifier: 211261
Keyword
Figure
Reference
-
References
1. Zacharias F. Årsrapport hysteroskopi 2015. Från gynopregistret delregister: hysteroskopi [Internet]. Umeå: Nationella Kvalitetsregistret inom Gynekologisk Kirurgi;2016. [cited 2018 May 15]. Available from: http://www.gynop.se/wp-content/uploads/2017/07/Gynop_Hysteroskopi_%C3%85rsrapport2015.pdf. Swedish.2. Paulo AA, Solheiro MH, Paulo CO, Afreixo VM. What proportion of women refers moderate to severe pain during office hysteroscopy with a mini-hysteroscope? A systematic review and meta-analysis. Arch Gynecol Obstet. 2016; 293:37–46.
Article3. Hassan A, Haggag H. Role of oral tramadol 50 mg in reducing pain associated with outpatient hysteroscopy: a randomised double-blind placebo-controlled trial. Aust N Z J Obstet Gynaecol. 2016; 56:102–6.
Article4. Borgbjerg FM, Nielsen K, Franks J. Experimental pain stimulates respiration and attenuates morphine-induced respiratory depression: a controlled study in human volunteers. Pain. 1996; 64:123–8.
Article5. Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017; 125:1733–40.6. Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017; 152:e170504.
Article7. Jafra A, Mitra S. Pain relief after ambulatory surgery: progress over the last decade. Saudi J Anaesth. 2018; 12:618–25.8. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965; 150:971–9.
Article9. Facchinetti F, Sandrini G, Petraglia F, Alfonsi E, Nappi G, Genazzani AR. Concomitant increase in nociceptive flexion reflex threshold and plasma opioids following transcutaneous nerve stimulation. Pain. 1984; 19:295–303.
Article10. Leonard G, Goffaux P, Marchand S. Deciphering the role of endogenous opioids in high-frequency TENS using low and high doses of naloxone. Pain. 2010; 151:215–9.
Article11. Le Bars D, Dickenson AH, Besson JM. Diffuse noxious inhibitory controls (DNIC). II. Lack of effect on non-convergent neurones, supraspinal involvement and theoretical implications. Pain. 1979; 6:305–27.
Article12. Proctor ML, Smith CA, Farquhar CM, Stones RW. Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev. 2002; (2):CD002123.13. Milsom I, Hedner N, Mannheimer C. A comparative study of the effect of high-intensity transcutaneous nerve stimulation and oral naproxen on intrauterine pressure and menstrual pain in patients with primary dysmenorrhea. Am J Obstet Gynecol. 1994; 170:123–9.
Article14. Yilmazer M, Kose S, Arioz DT, Koken G, Ozbulut O. Efficacy of transcutaneous electrical nerve stimulation for pain relief in women undergoing office endometrial biopsy. Arch Gynecol Obstet. 2012; 285:1059–64.
Article15. Kaplan B, Rabinerson D, Lurie S, Bar J, Krieser UR, Neri A. Transcutaneous electrical nerve stimulation (TENS) for adjuvant pain-relief during labor and delivery. Int J Gynaecol Obstet. 1998; 60:251–5.
Article16. Platon B, Andréll P, Raner C, Rudolph M, Dvoretsky A, Mannheimer C. High-frequency, high-intensity transcutaneous electrical nerve stimulation as treatment of pain after surgical abortion. Pain. 2010; 148:114–9.
Article17. Platon B, Mannheimer C, Andréll P. Effects of highfrequency, high-intensity transcutaneous electrical nerve stimulation versus intravenous opioids for pain relief after gynecologic laparoscopic surgery: a randomized controlled study. Korean J Anesthesiol. 2018; 71:149–56.
Article18. De Angelis C, Perrone G, Santoro G, Nofroni I, Zichella L. Suppression of pelvic pain during hysteroscopy with a transcutaneous electrical nerve stimulation device. Fertil Steril. 2003; 79:1422–7.
Article19. Lisón JF, Amer-Cuenca JJ, Piquer-Martí S, Benavent-Caballer V, Biviá-Roig G, Marín-Buck A. Transcutaneous nerve stimulation for pain relief during office hysteroscopy: a randomized controlled trial. Obstet Gynecol. 2017; 129:363–70.20. Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995; 61:277–84.
Article21. De Jonghe B, Cook D, Appere-De-Vecchi C, Guyatt G, Meade M, Outin H. Using and understanding sedation scoring systems: a systematic review. Intensive Care Med. 2000; 26:275–85.
Article22. Aubrun F, Mazoit JX, Riou B. Postoperative intravenous morphine titration. Br J Anaesth. 2012; 108:193–201.
Article23. Brandsborg B, Nikolajsen L. Chronic pain after hysterectomy. Curr Opin Anaesthesiol. 2018; 31:268–73.
Article24. Tangsiriwatthana T, Sangkomkamhang US, Lumbiganon P, Laopaiboon M. Paracervical local anaesthesia for cervical dilatation and uterine intervention. Cochrane Database Syst Rev. 2013; (9):CD005056.
Article25. Lau WC, Lo WK, Tam WH, Yuen PM. Paracervical anaesthesia in outpatient hysteroscopy: a randomised double-blind placebo-controlled trial. Br J Obstet Gynaecol. 1999; 106:356–9.
Article26. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006; 367:1618–25.
Article27. Mannheimer C, Carlsson CA, Vedin A, Wilhelmsson C. Transcutaneous electrical nerve stimulation (TENS) in angina pectoris. Pain. 1986; 26:291–300.
Article28. Moran F, Leonard T, Hawthorne S, Hughes CM, McCrum-Gardner E, Johnson MI, et al. Hypoalgesia in response to transcutaneous electrical nerve stimulation (TENS) depends on stimulation intensity. J Pain. 2011; 12:929–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of high-frequency, high-intensity transcutaneous electrical nerve stimulation versus intravenous opioids for pain relief after gynecologic laparoscopic surgery: a randomized controlled study
- Influence of Transcutaneous Electrical Nerve Stimulation on Cutaneous Silent Period
- Effects of Low and High Frequency Needle Transcutaneous Electrical Nerve Stimulation on Pain Threshold in Normal Adults
- Transcutaneous Electric Stimulation in Chronic Pain Patients
- Transcutaneous electrical nerve stimulation for pain during propofol injection: a randomized clinical trial