Acute Crit Care.
2020 Aug;35(3):207-212. 10.4266/acc.2019.00584.
Percutaneous bicaval dual lumen cannula for extracorporeal life support
- Affiliations
-
- 1Departments of Thoracic and Cardiovascular Surgery, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Departments of Pediatrics, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2506101
- DOI: http://doi.org/10.4266/acc.2019.00584
Abstract
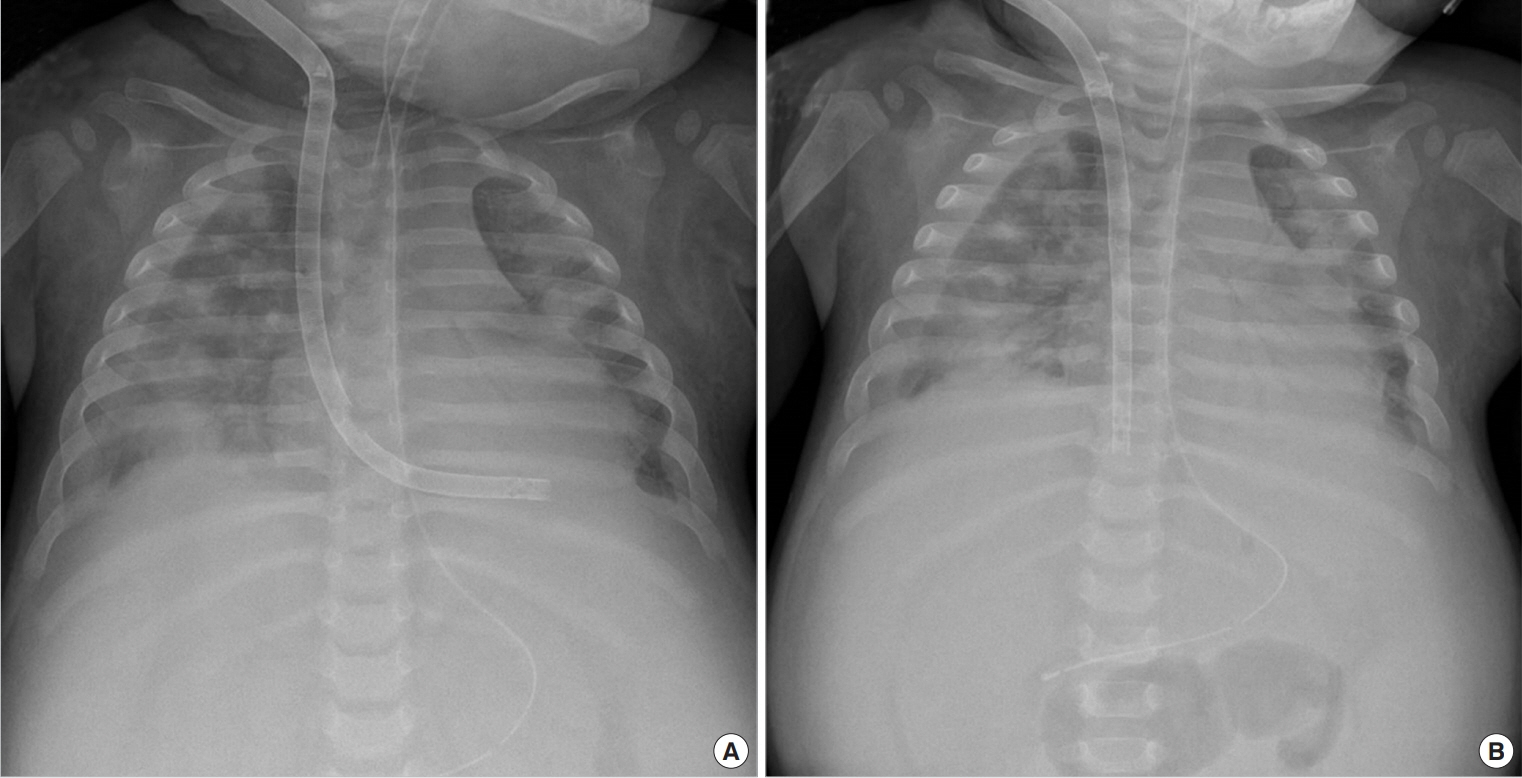
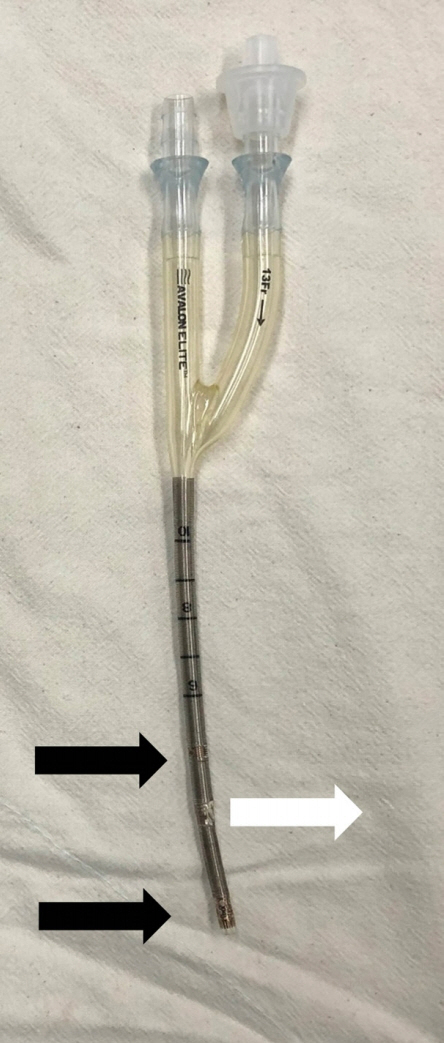
- Veno-venous extracorporeal membrane oxygenation (ECMO) is a useful mechanical device for pediatric patients with severe respiratory failure. Conventional veno-venous ECMO using double cannulation, however, is not feasible due to size limitations in pediatric patients who have small femoral vessels. Recently, percutaneous bicaval dual-lumen cannula can be inserted using single cannulation via the right internal jugular vein. Herein, we report the case of a pediatric patient with severe respiratory failure who was weaned off the ECMO successfully after treatment with bicaval dual-lumen cannulation for 5 days despite the small body size and immunocompromised condition due to chemotherapy for hemophagocytic lymphohistiocytosis.
Figure
Reference
-
1. Carpenter JL, Yu YR, Cass DL, Olutoye OO, Thomas JA, Burgman C, et al. Use of venovenous ECMO for neonatal and pediatric ECMO: a decade of experience at a tertiary children’s hospital. Pediatr Surg Int. 2018; 34:263–8.
Article2. Brogan TV, Lequier L, Lorusso R, MacLaren G, Peek G. Extracorporeal life support: the ELSO red book. Ann Arbor: Extracorporeal Life Support Organization;2017.3. Speggiorin S, Robinson SG, Harvey C, Westrope C, Faulkner GM, Kirkland P, et al. Experience with the Avalon® bicaval double-lumen veno-venous cannula for neonatal respiratory ECMO. Perfusion. 2015; 30:250–4.
Article4. Fallon SC, Shekerdemian LS, Olutoye OO, Cass DL, Zamora IJ, Nguyen T, et al. Initial experience with single-vessel cannulation for venovenous extracorporeal membrane oxygenation in pediatric respiratory failure. Pediatr Crit Care Med. 2013; 14:366–73.
Article5. Bermudez CA, Rocha RV, Sappington PL, Toyoda Y, Murray HN, Boujoukos AJ. Initial experience with single cannulation for venovenous extracorporeal oxygenation in adults. Ann Thorac Surg. 2010; 90:991–5.
Article6. Javidfar J, Brodie D, Wang D, Ibrahimiye AN, Yang J, Zwischenberger JB, et al. Use of bicaval dual-lumen catheter for adult venovenous extracorporeal membrane oxygenation. Ann Thorac Surg. 2011; 91:1763–8.
Article7. Salazar PA, Blitzer D, Dolejs SC, Parent JJ, Gray BW. Echocardiographic guidance during neonatal and pediatric jugular cannulation for ECMO. J Surg Res. 2018; 232:517–23.
Article8. Jarboe MD, Gadepalli SK, Church JT, Arnold MA, Hirschl RB, Mychaliska GB. Avalon catheters in pediatric patients requiring ECMO: placement and migration problems. J Pediatr Surg. 2018; 53:159–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extracorporeal Membrane Oxygenation Support for Dogs in Acute Respiratory Failure : Comparison of venovenous extracorporeal lung assist using a double lumen tube with venoarterial extracorporeal lung assist
- Transfromation of Percutaneous Extracorporeal Life Support to Paracorporeal Ventricular Assist Device: A Case Report
- Ventilation through a straw
- Left Atrial Decompression by Percutaneous Left Atrial Venting Cannula Insertion during Venoarterial Extracorporeal Membrane Oxygenation Support
- Percutaneous Extracorporeal Membrane Oxygenation (ECMO) for Acute Fulminant Myocarditis