Acute Crit Care.
2020 Aug;35(3):156-163. 10.4266/acc.2020.00199.
Clinical outcomes of difficult-to-wean patients with ventilator dependency at intensive care unit discharge
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Institute of Chest Diseases, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2506094
- DOI: http://doi.org/10.4266/acc.2020.00199
Abstract
- Background
Ventilator-dependent patients in the intensive care unit (ICU) who are difficult to wean from invasive mechanical ventilation (IMV) have been increasing in number. However, data on the clinical outcomes of difficult-to-wean patients are lacking. We aimed to evaluate clinical outcomes in patients discharged from the ICU with tracheostomy and ventilator dependency.
Methods
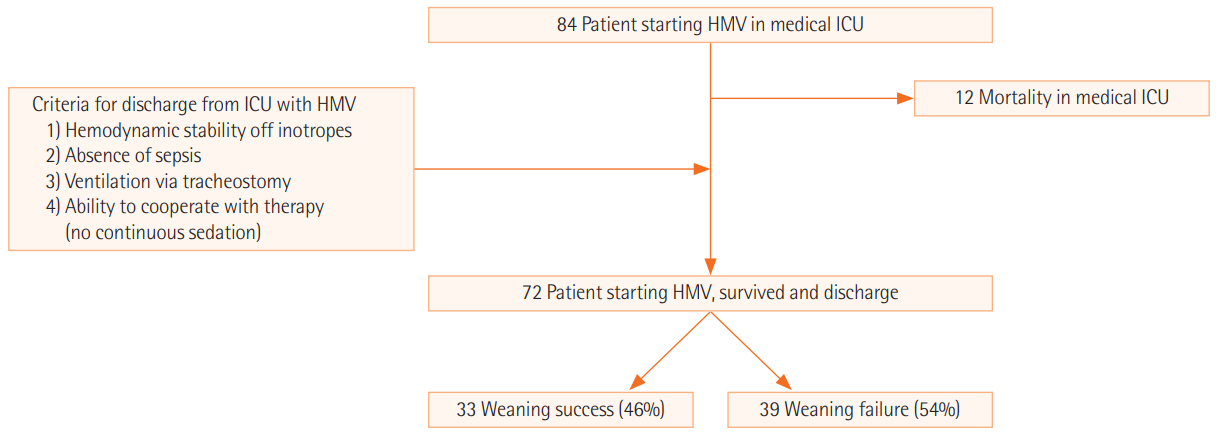
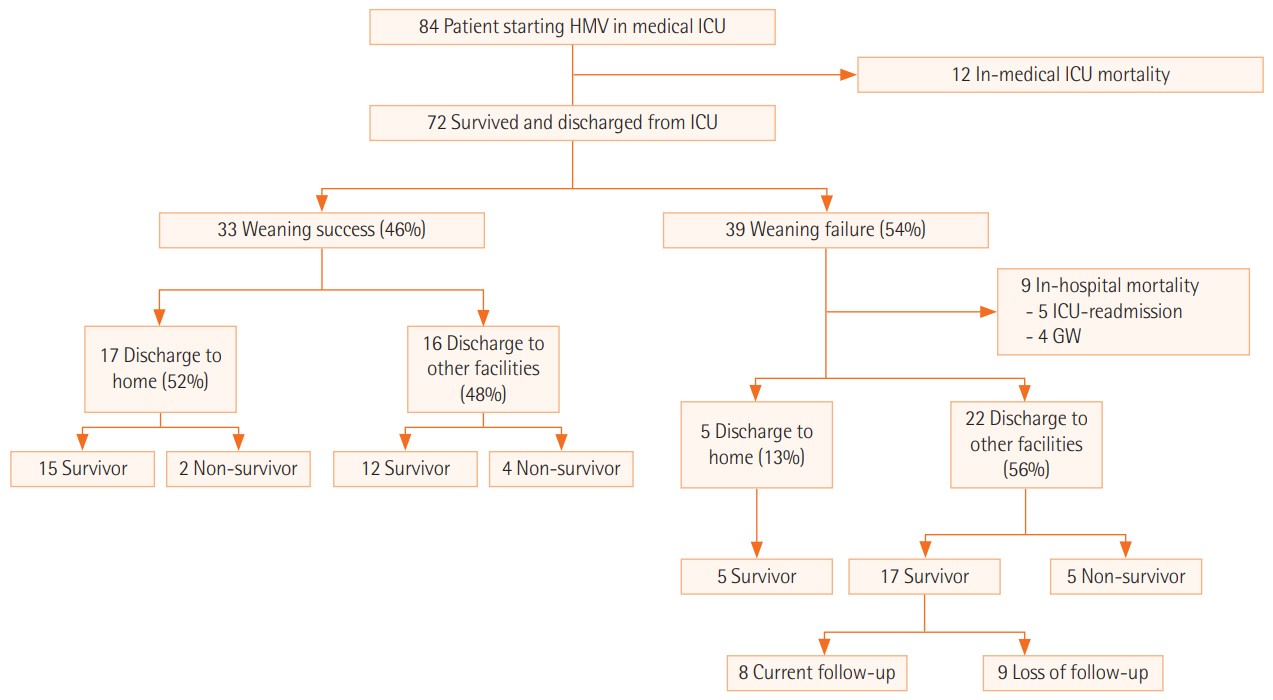
We retrospectively investigated clinical course and survival in patients requiring home mechanical ventilation (HMV) with a tracheostomy and difficulty weaning from IMV during medical ICU admission from September 2013 through August 2016 at Severance Hospital, Yonsei University, Seoul, Korea.
Results
Of 84 difficult-to-wean patients who were started on HMV in the medical ICU, 72 survived, were discharged from the ICU, and were included in this analysis. HMV was initiated after a median of 23 days of IMV, and the successful weaning rate was 46% (n = 33). In-hospital mortality rate was significantly lower in the successfully weaned group than the unsuccessfully weaned group (0% vs. 23.1%, respectively; P = 0.010). Weaning rates were similar according to primary diagnosis, but high body mass index (BMI), low Acute Physiologic Assessment and Chronic Health Evaluation (APACHE) II score at ICU admission, and absence of neuromuscular disease were associated with weaning success. After a median follow-up of 4.6 months (range, 1–27 months) for survivors, 3-month (n = 64) and 6-month (n = 59) survival rates were 82.5% and 72.2%, respectively. Survival rates were higher in the successfully weaned group than the unsuccessfully weaned group at 3 months (96.4% vs. 69.0%; P = 0.017) and 6 months (84.0% vs. 62.1%; P = 0.136) following ICU discharge.
Conclusions
In summary, 46% of patients who started HMV were successfully weaned from the ventilator in general wards. High BMI, low APACHE II score, and absence of neuromuscular disease were factors associated with weaning success.
Figure
Reference
-
1. Ambrosino N, Gabbrielli L. The difficult-to-wean patient. Expert Rev Respir Med. 2010; 4:685–92.
Article2. Esteban A, Anzueto A, Alía I, Gordo F, Apezteguía C, Pálizas F, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med. 2000; 161:1450–8.3. Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007; 29:1033–56.
Article4. MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner JE, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. 2001; 120(6 Suppl):375S–395S.5. Kahn JM, Carson SS, Angus DC, Linde-Zwirble WT, Iwashyna TJ. Development and validation of an algorithm for identifying prolonged mechanical ventilation in administrative data. Health Serv Outcomes Res Methodol. 2009; 9:117–32.
Article6. Carpenè N, Vagheggini G, Panait E, Gabbrielli L, Ambrosino N. A proposal of a new model for long-term weaning: respiratory intensive care unit and weaning center. Respir Med. 2010; 104:1505–11.
Article7. Bigatello LM, Stelfox HT, Berra L, Schmidt U, Gettings EM. Outcome of patients undergoing prolonged mechanical ventilation after critical illness. Crit Care Med. 2007; 35:2491–7.
Article8. Shin HJ, Chang JS, Ahn S, Kim TO, Park CK, Lim JH, et al. Clinical factors associated with weaning failure in patients requiring prolonged mechanical ventilation. J Thorac Dis. 2017; 9:143–50.
Article9. Lee SH, Kim MJ, Jeong ES, Jo EJ, Eom JS, Mok JH, et al. Outcomes and prognostic factors in patients with prolonged acute mechanical ventilation: a single-center study in Korea. J Crit Care. 2015; 30:1016–20.
Article10. Lee K, Hong SB, Lim CM, Koh Y. Sequential organ failure assessment score and comorbidity: valuable prognostic indicators in chronically critically ill patients. Anaesth Intensive Care. 2008; 36:528–34.
Article11. Kim MH, Cho WH, Lee K, Kim KU, Jeon DS, Park HK, et al. Prognostic factors of patients requiring prolonged mechanical ventilation in a medical intensive care unit of Korea. Tuberc Respir Dis (Seoul). 2012; 73:224–30.
Article12. Mok JH, Kim YH, Jeong ES, Eom JS, Kim MH, Kim KU, et al. Clinical application of the ProVent score in Korean patients requiring prolonged mechanical ventilation: a 10-year experience in a university-affiliated tertiary hospital. J Crit Care. 2016; 33:158–62.
Article13. Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med. 2010; 182:446–54.
Article14. Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M, LaBree LD, Heltsley DJ. Post-ICU mechanical ventilation: treatment of 1,123 patients at a regional weaning center. Chest. 1997; 111:1654–9.15. Slomka J, Hoffman-Hogg L, Mion LC, Bair N, Bobek MB, Arroliga AC. Influence of clinicians’ values and perceptions on use of clinical practice guidelines for sedation and neuromuscular blockade in patients receiving mechanical ventilation. Am J Crit Care. 2000; 9:412–8.
Article16. dos Santos CC, Slutsky AS. Protective ventilation of patients with acute respiratory distress syndrome. Crit Care. 2004; 8:145–7.17. Gillette MA, Hess DR. Ventilator-induced lung injury and the evolution of lung-protective strategies in acute respiratory distress syndrome. Respir Care. 2001; 46:130–48.18. Epstein SK. Decision to extubate. Intensive Care Med. 2002; 28:535–46.
Article19. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article20. Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015; 3:544–53.
Article21. Lai YC, Ruan SY, Huang CT, Kuo PH, Yu CJ. Hemoglobin levels and weaning outcome of mechanical ventilation in difficult-to-wean patients: a retrospective cohort study. PLoS One. 2013; 8:e73743.
Article22. Clochesy JM, Daly BJ, Montenegro HD. Weaning chronically critically ill adults from mechanical ventilatory support: a descriptive study. Am J Crit Care. 1995; 4:93–9.
Article23. Lim SY, Choi WI, Jeon K, Guallar E, Koh Y, Lim CM, et al. Body mass index and mortality in Korean intensive care units: a prospective multicenter cohort study. PLoS One. 2014; 9:e90039.
Article24. Kim H, Kim J, Seo C, Lee M, Cha MU, Jung SY, et al. Body mass index is inversely associated with mortality in patients with acute kidney injury undergoing continuous renal replacement therapy. Kidney Res Clin Pract. 2017; 36:39–47.
Article25. Pickkers P, de Keizer N, Dusseljee J, Weerheijm D, van der Hoeven JG, Peek N. Body mass index is associated with hospital mortality in critically ill patients: an observational cohort study. Crit Care Med. 2013; 41:1878–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concept of care shock during intensive care unit discharge process
- Clinical Features and Outcomes of Ventilator-Associated Pneumonia in Neonatal Intensive Care Unit Patients
- Clinical Application of Modified Burns Wean Assessment Program Scores at First Spontaneous Breathing Trial in Weaning Patients from Mechanical Ventilation
- Effect of a Clinical Nursing Practice Guideline of Enteral Nutrition Care on the Duration of Mechanical Ventilator for Critically Ill Patients
- Can the intensivists predict the outcomes of critically ill patients on the appropriateness of intensive care unit admission for limited intensive care unit resources ?