Acute Crit Care.
2020 Aug;35(3):142-148. 10.4266/acc.2020.00318.
Effectiveness of a multidisciplinary team for nutrition support in a trauma intensive care unit
- Affiliations
-
- 1Nutrition Support Team, Wonju Severance Christian Hospital, Wonju, Korea
- 2Dapartment of Pharmacy, Wonju Severance Christian Hospital, Wonju, Korea
- 3Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Trauma Center, Wonju Severance Christian Hospital, Wonju, Korea
- 5Department of Nutrition Services, Wonju Severance Christian Hospital, Wonju, Korea
- 6Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 7Department of Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2506092
- DOI: http://doi.org/10.4266/acc.2020.00318
Abstract
- Background
We evaluated clinical and nutritional outcomes according to multidisciplinary team involvement in nutrition support in a regional trauma intensive care unit (TICU).
Methods
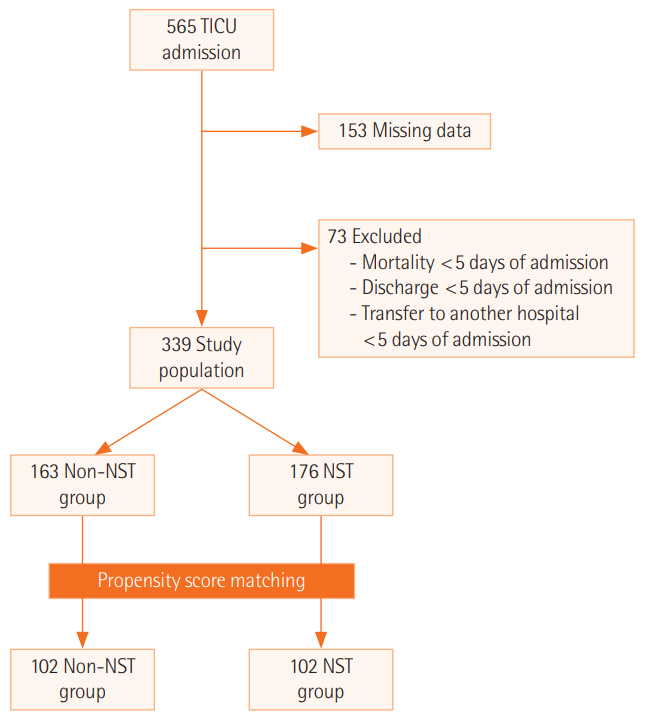
We retrospectively compared the outcomes for 339 patients admitted to the TICU for > 5 days depending on nutrition support team (NST) involvement (n = 176) and non-NST involvement (n = 163).
Results
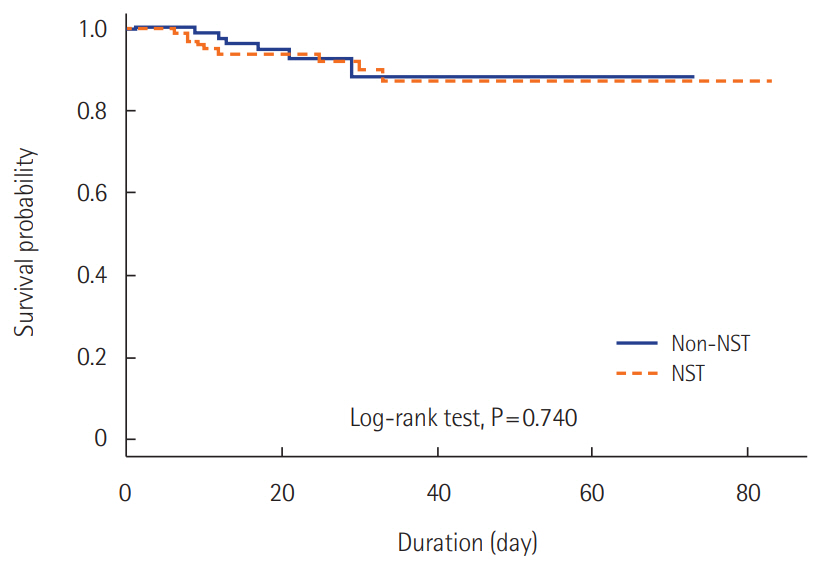
The mean age and injury severity score (ISS) were 57.3 ± 16.7 years and 18.6 ± 9.7, respectively. Fifty-three patients (15.6%) had shock on admission and 182 (53.7%) underwent surgery during TICU admission. Some patients were admitted to neurosurgery (46%), general surgery (35.4%), and other (18.6%) departments. There were significant differences in the ISS, Acute Physiology and Chronic Health Evaluation (APACHE) II score, shock on TICU admission, and initial laboratory results. After propensity score matching, the total delivered/required caloric ratio and total delivered/required protein ratio were significantly higher in the NST group than in the non-NST group (calorie: 80.4% vs. 66.7%, P = 0.007; protein: 93.1% vs.68.3%, P < 0.001). The NST group had an adequate protein supply more frequently than the non-NST group (protein: 48.0% vs. 25.8%, P = 0.002). There was no significant difference in survival, even after adjustment for risk factors using Cox proportional hazard analysis.
Conclusions
The results of our study suggest that multidisciplinary team involvement in nutrition support in TICU patients may improve nutritional, but not clinical, outcomes.
Figure
Cited by 1 articles
-
Lack of evidence for a nutritional support team in a trauma intensive care unit?
Jae Hwa Cho
Acute Crit Care. 2020;35(3):205-206. doi: 10.4266/acc.2020.00647.
Reference
-
1. Edington J, Boorman J, Durrant ER, Perkins A, Giffin CV, James R, et al. Prevalence of malnutrition on admission to four hospitals in England. The Malnutrition Prevalence Group. Clin Nutr. 2000; 19:191–5.2. Bruun LI, Bosaeus I, Bergstad I, Nygaard K. Prevalence of malnutrition in surgical patients: evaluation of nutritional support and documentation. Clin Nutr. 1999; 18:141–7.
Article3. Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003; 22:235–9.4. Mogensen KM, Robinson MK, Casey JD, Gunasekera NS, Moromizato T, Rawn JD, et al. Nutritional Status and mortality in the critically ill. Crit Care Med. 2015; 43:2605–15.
Article5. Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. 2009; 35:1728–37.
Article6. Lee JS, Kang JE, Park SH, Jin HK, Jang SM, Kim SA, et al. Nutrition and clinical outcomes of nutrition support in multidisciplinary team for critically ill patients. Nutr Clin Pract. 2018; 33:633–9.
Article7. Doig GS, Heighes PT, Simpson F, Sweetman EA. Early enteral nutrition reduces mortality in trauma patients requiring intensive care: a meta-analysis of randomised controlled trials. Injury. 2011; 42:50–6.
Article8. Dissanaike S, Pham T, Shalhub S, Warner K, Hennessy L, Moore EE, et al. Effect of immediate enteral feeding on trauma patients with an open abdomen: protection from nosocomial infections. J Am Coll Surg. 2008; 207:690–7.
Article9. Wang X, Dong Y, Han X, Qi XQ, Huang CG, Hou LJ. Nutritional support for patients sustaining traumatic brain injury: a systematic review and meta-analysis of prospective studies. PLoS One. 2013; 8:e58838.
Article10. Wasiak J, Cleland H, Jeffery R. Early versus delayed enteral nutrition support for burn injuries. Cochrane Database Syst Rev. 2006; (3):CD005489.
Article11. Wade CE, Kozar RA, Dyer CB, Bulger EM, Mourtzakis M, Heyland DK. Evaluation of nutrition deficits in adult and elderly trauma patients. JPEN J Parenter Enteral Nutr. 2015; 39:449–55.
Article12. Jang JY, Shim H, Kwon HY, Chung H, Jung PY, Kim S, et al. Improvement of outcomes in patients with pelvic fractures and hemodynamic instability after the establishment of a Korean regional trauma center. Eur J Trauma Emerg Surg. 2019; 45:107–13.
Article13. Kudsk KA, Croce MA, Fabian TC, Minard G, Tolley EA, Poret HA, et al. Enteral versus parenteral feeding. Effects on septic morbidity after blunt and penetrating abdominal trauma. Ann Surg. 1992; 215:503–11.
Article14. Moore FA, Feliciano DV, Andrassy RJ, McArdle AH, Booth FV, Morgenstein-Wagner TB, et al. Early enteral feeding, compared with parenteral, reduces postoperative septic complications: the results of a meta-analysis. Ann Surg. 1992; 216:172–83.
Article15. Rhee P, Hadjizacharia P, Trankiem C, Chan L, Salim A, Brown C, et al. What happened to total parenteral nutrition? The disappearance of its use in a trauma intensive care unit. J Trauma. 2007; 63:1215–22.
Article16. Plurad D, Green D, Inaba K, Belzberg H, Demetriades D, Rhee P. A 6-year review of total parenteral nutrition use and association with late-onset acute respiratory distress syndrome among ventilated trauma victims. Injury. 2009; 40:511–5.
Article17. Lee SH, Jang JY, Kim HW, Jung MJ, Lee JG. Effects of early enteral nutrition on patients after emergency gastrointestinal surgery: a propensity score matching analysis. Medicine (Baltimore). 2014; 93:e323.18. Jeong HS, Teong CH, Kim WJ, Lee AR. Attitudes of medical staff and factors related to nutritional support for patient care in a university hospital. J Clin Nutr. 2014; 6:37–41.
Article19. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017; 126:376–93.20. Smith I, Kranke P, Murat I, Smith A, O’Sullivan G, Søreide E, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011; 28:556–69.21. DeChicco R, Neal T, Guardino JM. Developing an education program for nutrition support teams. Nutr Clin Pract. 2010; 25:481–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Status of Intensive Care Unit Patients According to the Referral to the Nutrition Support Team and Compliance with the Recommendations
- Organization and Roles of the Trauma Team
- Lack of evidence for a nutritional support team in a trauma intensive care unit?
- Nutrition Support in Trauma Patients
- Enteral Nutrition Strategies for Achieving Glycemic Control in the Critical Care Setting