J Korean Med Sci.
2020 Sep;35(35):e321. 10.3346/jkms.2020.35.e321.
Estimating the Effectiveness of Non-Pharmaceutical Interventions on COVID-19 Control in Korea
- Affiliations
-
- 1Institute of Health and Environment, Graduate School of Public Health, Seoul National University, Seoul, Korea
- 2Department of Public Health Science, Graduate School of Public Health, Seoul National University, Seoul, Korea
- KMID: 2506088
- DOI: http://doi.org/10.3346/jkms.2020.35.e321
Abstract
- Background
The coronavirus disease 2019 (COVID-19) pandemic has posed significant global public health challenges and created a substantial economic burden. Korea has experienced an extensive outbreak, which was linked to a religion-related super-spreading event. However, the implementation of various non-pharmaceutical interventions (NPIs), including social distancing, spring semester postponing, and extensive testing and contact tracing controlled the epidemic. Herein, we estimated the effectiveness of each NPI using a simulation model.
Methods
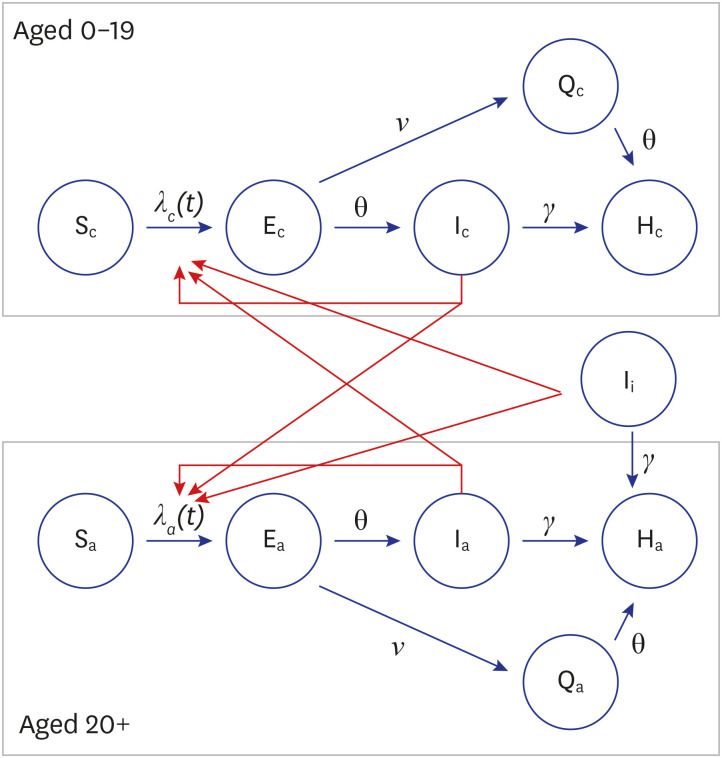
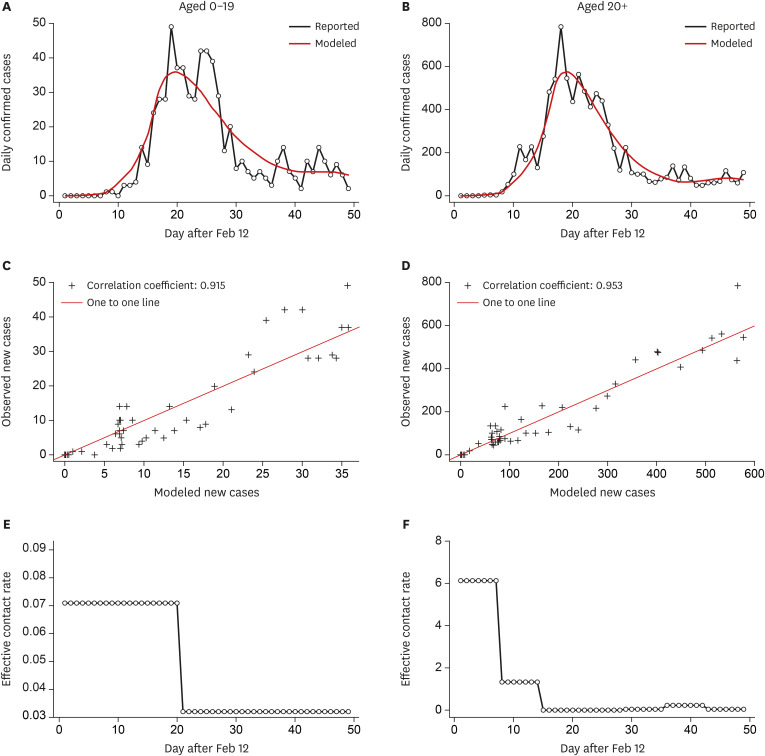
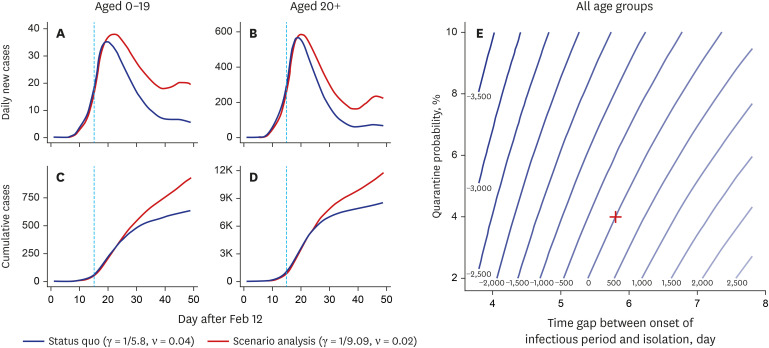
A compartment model with a susceptible-exposed-infectious-quarantinedhospitalized structure was employed. Using the Monte-Carlo-Markov-Chain algorithm with Gibbs' sampling method, we estimated the time-varying effective contact rate to calibrate the model with the reported daily new confirmed cases from February 12th to March 31st (7 weeks). Moreover, we conducted scenario analyses by adjusting the parameters to estimate the effectiveness of NPI.
Results
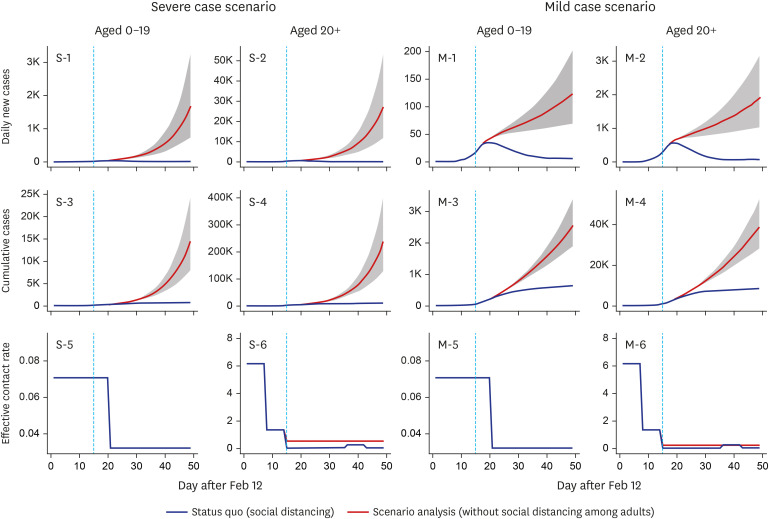
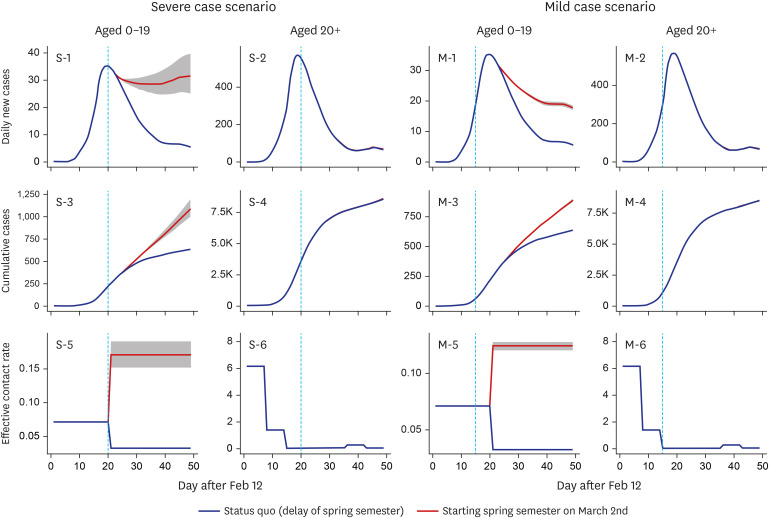
Relaxed social distancing among adults would have increased the number of cases 27.4-fold until the end of March. Spring semester non-postponement would have increased the number of cases 1.7-fold among individuals aged 0–19, while lower quarantine and detection rates would have increased the number of cases 1.4-fold.
Conclusion
Among the three NPI measures, social distancing in adults showed the highest effectiveness. The substantial effect of social distancing should be considered when preparing for the 2nd wave of COVID-19.
Figure
Cited by 1 articles
-
Nationwide Trends in Non-COVID-19 Infectious Disease Laboratory Tests in the Era of the COVID-19 Pandemic in Korea
Sun Bean Kim, Young-Eun Kim, Taemo Bang, Minwoo Hong, Munkhzul Radnaabaatar, Kyungmin Huh, Ki Ho Hong, Jaehun Jung
J Korean Med Sci. 2023;38(47):e408. doi: 10.3346/jkms.2023.38.e408.
Reference
-
1. World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 88. Geneva: World Health Organization;2020.2. Maliszewska M, Mattoo A, Van Der Mensbrugghe D. The Potential Impact of COVID-19 on GDP and Trade: a Preliminary Assessment. World Bank Policy Research Working Paper. Washington, D.C.: The World Bank;2020.3. Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020; 25(10):2000180.
Article4. Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ. 2020; 368:m1165. PMID: 32205334.
Article5. Ki M. Task Force for 2019-nCoV. Epidemiologic characteristics of early cases with 2019 novel coronavirus (2019-nCoV) disease in Korea. Epidemiol Health. 2020; 42:e2020007. PMID: 32035431.
Article6. Korean Society of Infectious Diseases. Korean Society of Pediatric Infectious Diseases. Korean Society of Epidemiology. Korean Society for Antimicrobial Therapy. Korean Society for Healthcare-associated Infection Control and Prevention. Korea Centers for Disease Control and Prevention. Report on the Epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020; 35(10):e112. PMID: 32174069.7. Walker PG, Whittaker C, Watson O, Baguelin M, Ainslie K, Bhatia S, et al. The global impact of covid-19 and strategies for mitigation and suppression. Updated 2020. https://www.preventionweb.net/publications/view/71077.8. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020; 172(9):577–582. PMID: 32150748.
Article9. Pan Y, Zhang D, Yang P, Poon LL, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020; 20(4):411–412. PMID: 32105638.
Article10. Gyeonggi Infectious Disease Control Center. Coronavirus Disease 2019 (COVID-19) Gyeonggi Daily Report, Data as Reported by 5 April 2020. Seongnam: Gyeonggi Infectious Disease Control Center;2020.11. Morton A, Finkenstädt BF. Discrete time modelling of disease incidence time series by using Markov chain Monte Carlo methods. J R Stat Soc C Appl. 2005; 54(3):575–594.
Article12. O'Neill PD. A tutorial introduction to Bayesian inference for stochastic epidemic models using Markov chain Monte Carlo methods. Math Biosci. 2002; 180(1-2):103–114. PMID: 12387918.13. Hellewell J, Abbott S, Gimma A, Bosse NI, Jarvis CI, Russell TW, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020; 8(4):e488–96. PMID: 32119825.
Article14. Pastorino B, Touret F, Gilles M, de Lamballerie X, Charrel RN. Evaluation of heating and chemical protocols for inactivating SARS-CoV-2. bioRxiv. Forthcoming. 2020; DOI: 10.1101/2020.04.11.036855.
Article15. Ferguson N, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M, et al. Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. London: Imperial College COVID-19 Response Team;2020.16. Kraemer MU, Yang CH, Gutierrez B, Wu CH, Klein B, Pigott DM, et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020; 368(6490):493–497. PMID: 32213647.
Article17. Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical interventions for containing the COVID-19 outbreak in China. medRxiv. Forthcoming. 2020; DOI: 10.1101/2020.03.03.20029843.
Article18. Kim S, Kim YJ, Peck KR, Jung E. School opening delay effect on transmission dynamics of coronavirus disease 2019 in Korea: based on mathematical modeling and simulation study. J Korean Med Sci. 2020; 35(13):e143. PMID: 32242349.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dynamics of the COVID-19 epidemic in the post-vaccination period in Korea: a rapid assessment
- Trends in gastrointestinal infections before and during non-pharmaceutical interventions in Korea in comparison with the United States
- Epidemiological changes in infectious diseases during the coronavirus disease 2019 pandemic in Korea: a systematic review
- Examination of Predicting Factors for COVID-19 Vaccination Behaviors of University Students Utilizing the Theory of Planned Behavior
- Requirements for Reusable Infection Prevention and Control Measures for COVID-19 Response