Arch Hand Microsurg.
2020 Sep;25(3):219-224. 10.12790/ahm.20.0034.
Distribution of Anterolateral Thigh Flap Perforator Vessels and Its Clinical Applications in Malaysian Population
- Affiliations
-
- 1Reconstructive Sciences Unit, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Malaysia
- 2Department of Plastic and Reconstructive Surgery, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
- 3Plastic and Reconstructive Unit, MSU Medical Center, Management and Science University, Shah Alam, Malaysia
- KMID: 2505903
- DOI: http://doi.org/10.12790/ahm.20.0034
Abstract
- Purpose
Extensive studies regarding vascular anatomy and clinical applications of anterolateral thigh (ALT) flap has been conducted for many years. However, the ALT flap perforator vessels anatomy in the Malaysian population is not well-analyzed. The purpose of this study was to determine the distribution of ALT flap perforator vessels and its clinical applications in reconstructive surgery.
Methods
This is a retrospective cross-sectional study conducted in two main centers of reconstructive surgery. A total of 142 cases of ALT flaps that used as an option for soft tissue reconstruction was selected. Vascular anatomy of ALT flaps was studied precisely including the origin of vessels, location of perforators, and types of perforator vessels intraoperatively during the flap harvest.
Results
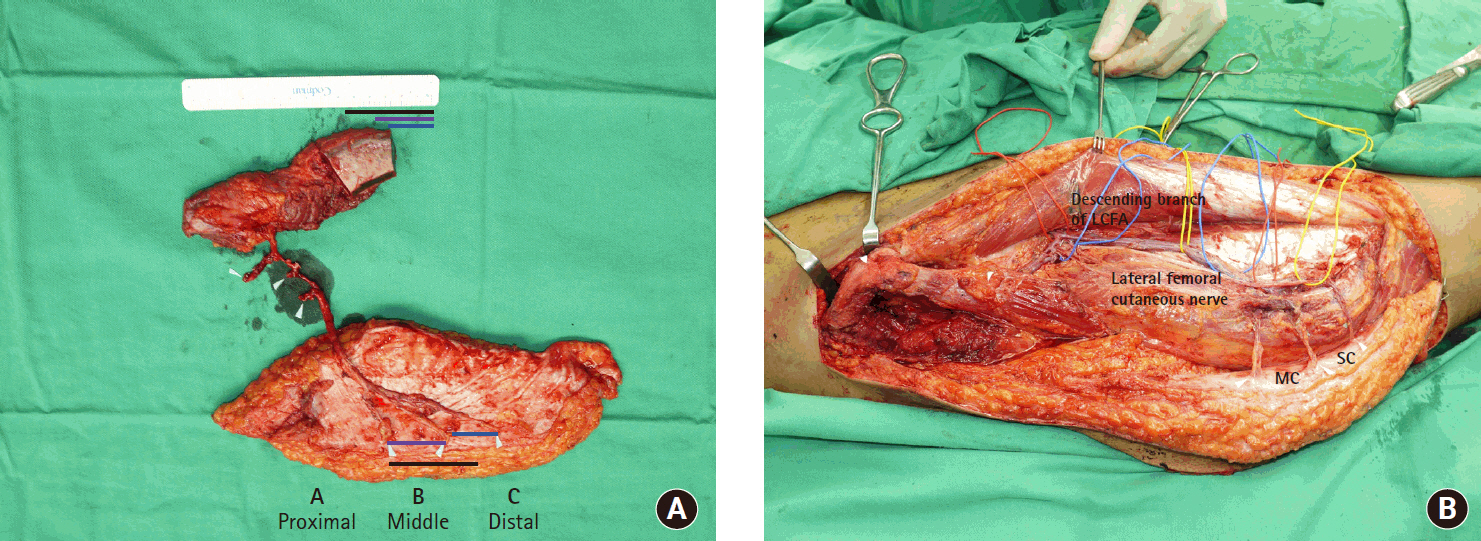
The distribution of ALT flap perforator vessels can be found at three specific locations on the thigh namely perforators A, B, and C. The highest number of cutaneous perforator vessels that supplied the ALT flap was musculocutaneous perforator with 72.3%, and dominantly at perforators B and C. The remaining perforator vessels were septocutaneous perforator with 27.7%, presented mainly at perforator A. A majority of cases involved the reconstruction of wound defects following tumor resection and trauma. The most area of reconstruction was the lower limb with 33.8%.
Conclusion
The distribution of ALT flap perforator vessels can be predicted during flap harvest and can be applied in numerous clinical applications for wound defect coverage. The knowledge regarding vascular anatomy of ALT flap perforator vessels can aid plastic surgeons in reconstructive surgery.
Figure
Reference
-
1. Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984; 37:149–59.
Article2. Valdatta L, Tuinder S, Buoro M, Thione A, Faga A, Putz R. Lateral circumflex femoral arterial system and perforators of the anterolateral thigh flap: An anatomic study. Ann Plast Surg. 2002; 49:145–50.
Article3. Lee YC, Chen WC, Chou TM, Shieh SJ. Anatomical variability of the anterolateral thigh flap perforators: vascular anatomy and its clinical implications. Plast Reconstr Surg. 2015; 135:1097–107.4. Lakhiani C, Lee MR, Saint-Cyr M. Vascular anatomy of the anterolateral thigh flap: a systematic review. Plast Reconstr Surg. 2012; 130:1254–68.5. Mourougayan V. Variation in the vascular anatomy of anterolateral thigh flap and its management. Eur J Plast Surg. 2005; 28:340–2.
Article6. Kawai K, Imanishi N, Nakajima H, Aiso S, Kakibuchi M, Hosokawa K. Vascular anatomy of the anterolateral thigh flap. Plast Reconstr Surg. 2004; 114:1108–17.
Article7. Malhotra K, Lian TS, Chakradeo V. Vascular anatomy of anterolateral thigh flap. Laryngoscope. 2008; 118:589–92.
Article8. Seth R, Manz RM, Dahan IJ, et al. Comprehensive analysis of the anterolateral thigh flap vascular anatomy. Arch Facial Plast Surg. 2011; 13:347–54.
Article9. Darji AP, Chauhan H, Shrimankar P, et al. A cadaveric study of variations in the origin of lateral circumflex femoral artery. Int J Anat Res. 2015; 3:1732–6.
Article10. Tansatit T, Wanidchaphloi S, Sanguansit P. The anatomy of the lateral circumflex femoral artery in anterolateral thigh flap. J Med Assoc Thai. 2008; 91:1404–9.11. Yu P. Characteristics of the anterolateral thigh flap in a Western population and its application in head and neck reconstruction. Head Neck. 2004; 26:759–69.
Article12. Yu P, Youssef A. Efficacy of the handheld doppler in preoperative identification of the cutaneous perforators in the anterolateral thigh flap. Plast Reconstr Surg. 2006; 118:928–35.
Article13. Xu Z, Zhao XP, Yan TL, et al. A 10-year retrospective study of free anterolateral thigh flap application in 872 head and neck tumour cases. Int J Oral Maxillofac Surg. 2015; 44:1088–94.
Article14. Lee JC, St-Hilaire H, Christy MR, Wise MW, Rodriguez ED. Anterolateral thigh flap for trauma reconstruction. Ann Plast Surg. 2010; 64:164–8.
Article15. Wolff KD, Kesting M, Thurmüller P, Böckmann R, Hölzle F. The anterolateral thigh as a universal donor site for soft tissue reconstruction in maxillofacial surgery. J Craniomaxillofac Surg. 2006; 34:323–31.
Article16. Nasajpour H, Steele MH. Anterolateral thigh free flap for “head-to-toe” reconstruction. Ann Plast Surg. 2011; 66:530–3.
Article17. Garvey PB, Selber JC, Madewell JE, Bidaut L, Feng L, Yu P. A prospective study of preoperative computed tomographic angiography for head and neck reconstruction with anterolateral thigh flaps. Plast Reconstr Surg. 2011; 127:1505–14.
Article18. Ao M, Uno K, Maeta M, Nakagawa F, Saito R, Nagase Y. De-epithelialised anterior (anterolateral and anteromedial) thigh flaps for dead space filling and contour correction in head and neck reconstruction. Br J Plast Surg. 1999; 52:261–7.
Article19. Ali RS, Bluebond-Langner R, Rodriguez ED, Cheng MH. The versatility of the anterolateral thigh flap. Plast Reconstr Surg. 2009; 124(6 Suppl):e395–407.
Article20. Bhadkamkar MA, Wolfswinkel EM, Hatef DA, et al. The ultra-thin, fascia-only anterolateral thigh flap. J Reconstr Microsurg. 2014; 30:599–606.
Article21. Liu WW, Yang AK, Ou YD. The harvesting and insetting of a chimeric anterolateral thigh flap to reconstruct through and through cheek defects. Int J Oral Maxillofac Surg. 2011; 40:1421–3.
Article22. Sananpanich K, Tu YK, Kraisarin J, Chalidapong P. Flow-through anterolateral thigh flap for simultaneous soft tissue and long vascular gap reconstruction in extremity injuries: Anatomical study and case report. Injury. 2008; 39 Suppl 4:47–54.
Article23. Demirkan F, Chen HC, Wei FC, et al. The versatile anterolateral thigh flap: A musculocutaneous flap in disguise in head and neck reconstruction. Br J Plast Surg. 2000; 53:30–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of the Digit Using Anterolateral Thigh Perforator Flap
- Anatomical Characteristics and Versatility of the Anterolateral Thigh Flap
- Scrotal Reconstruction with Pedicled Anterolateral Thigh Perforator Flap
- Reconstruction of Soft Tissue Defect of Knee Joint Area Using Anterolateral Thigh Perforator Flap
- Scrotal Reconstruction with Pedicled Anterolateral Thigh Perforator Flap in Fournier's Gangrene