J Korean Med Sci.
2020 Aug;35(33):e278. 10.3346/jkms.2020.35.e278.
Beta-blocker Therapy at Discharge in Patients with Acute Heart Failure and Atrial Fibrillation
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Center of Biomedical Data Science, Yonsei University Wonju College of Medicine, Wonju, Korea
- 3Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 4Department of Internal Medicine, School of Medicine, Sungkyunkwan University, Seoul, Korea
- 5Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 6Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 7Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 8Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 9Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 10Department of Internal Medicine, Heart Research Center of Chonnam National University, Gwangju, Korea
- 11Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea
- 12MetroWest Medical Center, Framingham, MA, USA
- KMID: 2505594
- DOI: http://doi.org/10.3346/jkms.2020.35.e278
Abstract
- Background
β-blockers (BBs) are considered primary therapy in stable heart failure (HF) with reduced ejection fraction (HFrEF) without atrial fibrillation (AF); evidence-based benefits of BB on outcome have been documented. However, BBs have not been shown to improve mortality or reduce hospital admissions in HF patients with AF. This study assessed the relationship between BBs at discharge and relevant clinical outcomes in acute heart failure (AHF) patients with AF.
Methods
From the Korean Acute Heart Failure Registry, 936 HFrEF and 639 HF patients with preserved ejection fraction (HFpEF) and AF were selected. Propensity score (PS) matching accounted for BB selection bias when assessing associations.
Results
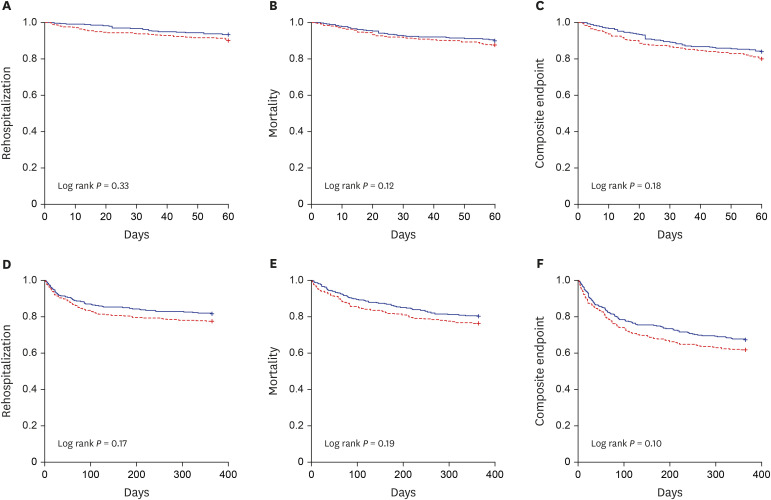
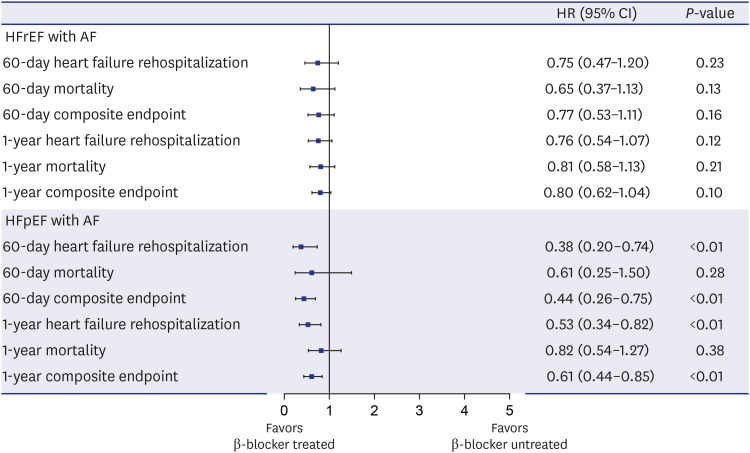
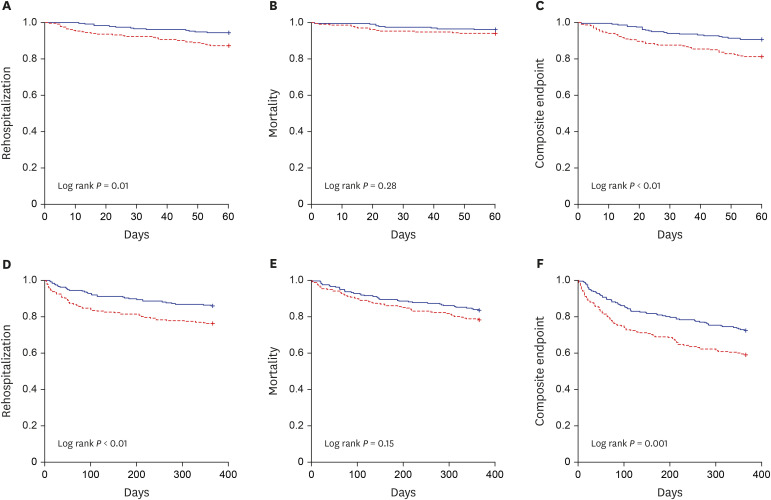
BB-untreated patients in the overall cohort of HFrEF and HFpEF had greater deteriorated clinical and laboratory characteristics. In the 670 PS-matched cohort of HFrEF patients, incidences of all clinical events at 60 days and 1 year were not different according to use of BBs. In the 470 PS-matched cohort of HFpEF, rehospitalization and composite outcome at 6 months and 1 year more frequently occurred in non-users of BBs. After adjusting for covariates in the multivariable Cox model of matched cohorts, BB was not associated with clinical outcomes at 60 days and 1 year in HFrEF with AF patients. In HFpEF patients with AF, BB use was associated with reduced 6-month (hazard ratio [HR], 0.38; 95% confidence interval [CI], 0.20–0.74) and 1-year rehospitalization (HR, 0.53; 95% CI, 0.34–0.82).
Conclusion
In the HFrEF with AF PS-matched cohort, the use of BBs at discharge was not associated with clinical outcome. However, in HFpEF with AF, the use of BB was associated with reduced rehospitalization during the 6-month and 1-year follow up.
Keyword
Figure
Reference
-
1. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128(16):1810–1852. PMID: 23741057.2. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37(27):2129–2200. PMID: 27206819.3. Lee DS, Tu JV, Juurlink DN, Alter DA, Ko DT, Austin PC, et al. Risk-treatment mismatch in the pharmacotherapy of heart failure. JAMA. 2005; 294(10):1240–1247. PMID: 16160132.
Article4. Harjola VP, Follath F, Nieminen MS, Brutsaert D, Dickstein K, Drexler H, et al. Characteristics, outcomes, and predictors of mortality at 3 months and 1 year in patients hospitalized for acute heart failure. Eur J Heart Fail. 2010; 12(3):239–248. PMID: 20156940.
Article5. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999; 353(9169):2001–2007. PMID: 10376614.6. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet. 1999; 353(9146):9–13. PMID: 10023943.7. Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001; 344(22):1651–1658. PMID: 11386263.
Article8. Chiang CE, Naditch-Brûlé L, Murin J, Goethals M, Inoue H, O’Neill J, et al. Distribution and risk profile of paroxysmal, persistent, and permanent atrial fibrillation in routine clinical practice: insight from the real-life global survey evaluating patients with atrial fibrillation international registry. Circ Arrhythm Electrophysiol. 2012; 5(4):632–639. PMID: 22787011.9. Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003; 107(23):2920–2925. PMID: 12771006.10. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64(21):e1–76. PMID: 24685669.11. Rienstra M, Damman K, Mulder BA, Van Gelder IC, McMurray JJ, Van Veldhuisen DJ. Beta-blockers and outcome in heart failure and atrial fibrillation: a meta-analysis. JACC Heart Fail. 2013; 1(1):21–28. PMID: 24621795.12. Kotecha D, Holmes J, Krum H, Altman DG, Manzano L, Cleland JG, et al. Efficacy of β blockers in patients with heart failure plus atrial fibrillation: an individual-patient data meta-analysis. Lancet. 2014; 384(9961):2235–2243. PMID: 25193873.
Article13. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18(8):891–975. PMID: 27207191.14. Lee SE, Cho HJ, Lee HY, Yang HM, Choi JO, Jeon ES, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014; 16(6):700–708. PMID: 24797348.
Article15. Ahn MS, Yoo BS, Yoon J, Lee SH, Kim JY, Ahn SG, et al. Guideline-directed therapy at discharge in patients with heart failure and atrial fibrillation. Heart. 2020; 106(4):292–298. PMID: 31492703.
Article16. Kotecha D, Flather MD, Altman DG, Holmes J, Rosano G, Wikstrand J, et al. Heart rate and rhythm and the benefit of beta-blockers in patients with heart failure. J Am Coll Cardiol. 2017; 69(24):2885–2896. PMID: 28467883.17. Li SJ, Sartipy U, Lund LH, Dahlström U, Adiels M, Petzold M, et al. Prognostic significance of resting heart rate and use of β-blockers in atrial fibrillation and sinus rhythm in patients with heart failure and reduced ejection fraction: findings from the Swedish Heart Failure Registry. Circ Heart Fail. 2015; 8(5):871–879. PMID: 26243796.18. Nielsen PB, Larsen TB, Gorst-Rasmussen A, Skjøth F, Lip GY. β-blockers in atrial fibrillation patients with or without heart failure: association with mortality in a nationwide cohort study. Circ Heart Fail. 2016; 9(2):e002597. PMID: 26823497.
Article19. Cohn JN, Pfeffer MA, Rouleau J, Sharpe N, Swedberg K, Straub M, et al. Adverse mortality effect of central sympathetic inhibition with sustained-release moxonidine in patients with heart failure (MOXCON). Eur J Heart Fail. 2003; 5(5):659–667. PMID: 14607206.
Article20. Simpson J, Castagno D, Doughty RN, Poppe KK, Earle N, Squire I, et al. Is heart rate a risk marker in patients with chronic heart failure and concomitant atrial fibrillation? Results from the MAGGIC meta-analysis. Eur J Heart Fail. 2015; 17(11):1182–1191. PMID: 26358762.
Article21. Olsson LG, Swedberg K, Ducharme A, Granger CB, Michelson EL, McMurray JJ, et al. Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure-Assessment of Reduction in Mortality and morbidity (CHARM) program. J Am Coll Cardiol. 2006; 47(10):1997–2004. PMID: 16697316.22. Cleland JG, Bunting KV, Flather MD, Altman DG, Holmes J, Coats AJ, et al. Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. Eur Heart J. 2018; 39(1):26–35. PMID: 29040525.
Article23. Wachter R, Schmidt-Schweda S, Westermann D, Post H, Edelmann F, Kasner M, et al. Blunted frequency-dependent upregulation of cardiac output is related to impaired relaxation in diastolic heart failure. Eur Heart J. 2009; 30(24):3027–3036. PMID: 19720638.
Article24. Meyer M, LeWinter MM. Heart rate and heart failure with preserved ejection fraction: time to slow β-blocker use? Circ Heart Fail. 2019; 12(8):e006213. PMID: 31525068.25. Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010; 362(15):1363–1373. PMID: 20231232.
Article26. Lam PH, Dooley DJ, Deedwania P, Singh SN, Bhatt DL, Morgan CJ, et al. Heart rate and outcomes in hospitalized patients with heart failure with preserved ejection fraction. J Am Coll Cardiol. 2017; 70(15):1861–1871. PMID: 28982499.