J Korean Med Sci.
2020 Aug;35(32):e283. 10.3346/jkms.2020.35.e283.
A Premature Baby with Severe Oligohydramnios and Hypotension: a Case Report of Renal Tubular Dysgenesis
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Hospital, Seoul, Korea
- 2Department of Pediatrics, Soonchunhyang University Hospital, Seoul, Korea
- 3Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 4Kidney Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 5Wide River Institute of Immunology, Seoul National University, Seoul, Korea
- KMID: 2505582
- DOI: http://doi.org/10.3346/jkms.2020.35.e283
Abstract
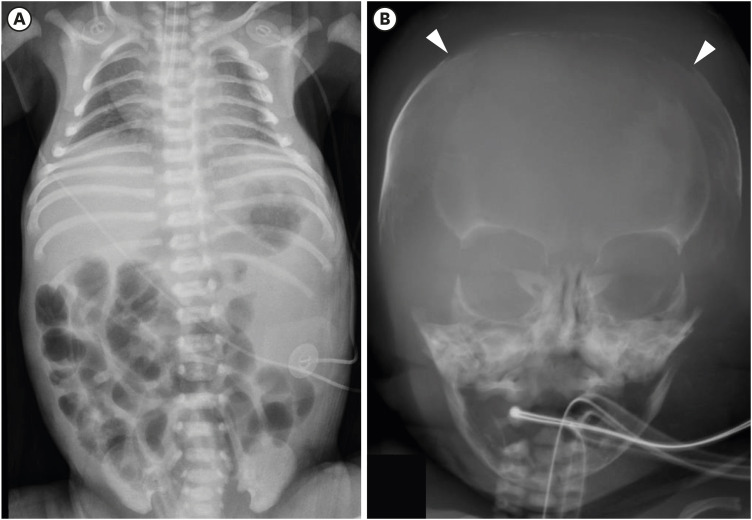
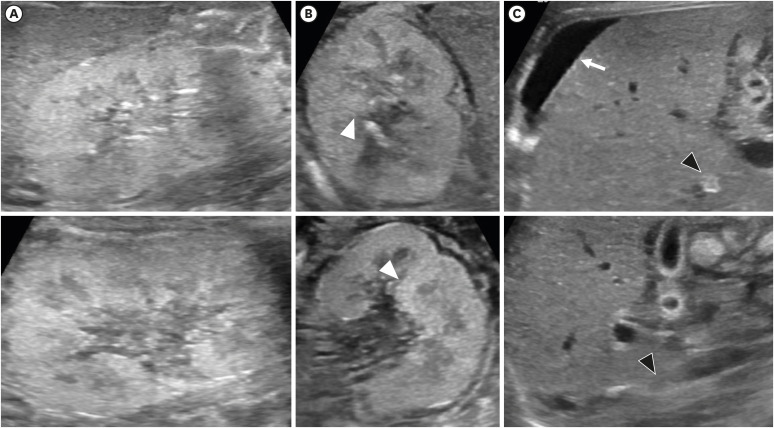
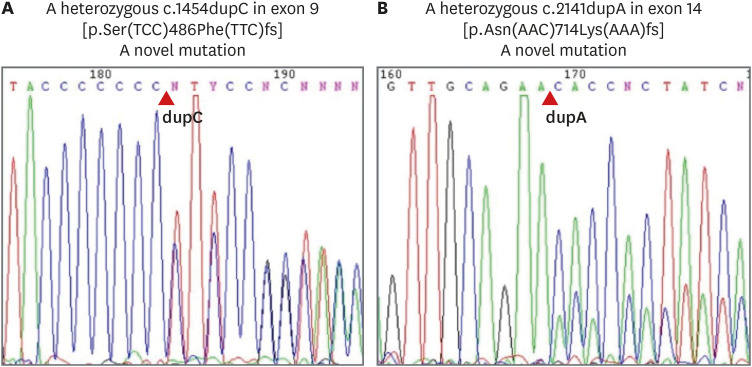
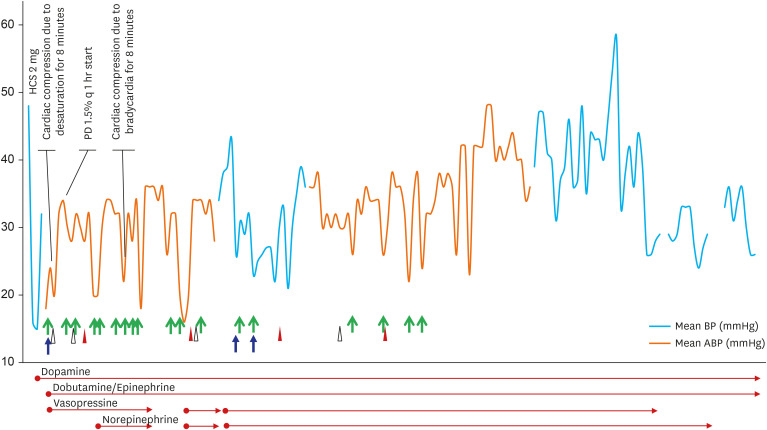
- Renal tubular dysgenesis (RTD) is a rare fatal disorder in which there is poor development of proximal tubules, leading to oligohydramnios and the Potter sequences. RTD occurs secondary to renin-angiotensin system (RAS) blockade during the early stages of fetal development or due to autosomal recessive mutation of genes in the RAS pathway. A boy born at 33+1 weeks due to cord prolapse was found to be anuric and hypotensive. Pregnancy was complicated by severe oligohydramnios from gestational age 28+4 weeks. Abdominal sonography revealed diffuse globular enlargement of both kidneys with increased cortical parenchymal echogenicity. Infantogram showed a narrow thoracic cage and skull X-ray showed large fontanelles and wide sutures suggestive of ossification delay. Basal plasma renin activity was markedly elevated and angiotensin-converting enzyme was undetectable. Despite adequate use of medications, peritoneal dialysis, and respiratory support, he did not recover and expired on the 23rd day of life. At first, autosomal recessive polycystic kidney disease was suspected, but severe oligohydramnios along with refractory hypotension, anuria, skull ossification delay and high renin levels made RTD suspicious. ACE gene analysis revealed compound heterozygous pathogenic variations of c.1454.dupC in exon 9 and c.2141dupA in exon 14, confirming RTD. Based on our findings, we propose that, although rare, RTD should be suspected in patients with severe oligohydramnios and refractory hypotension.
Figure
Reference
-
1. Kozinszky Z, Sikovanyecz J, Pásztor N. Severe midtrimester oligohydramnios: treatment strategies. Curr Opin Obstet Gynecol. 2014; 26(2):67–76. PMID: 24614021.2. Klaassen I, Neuhaus TJ, Mueller-Wiefel DE, Kemper MJ. Antenatal oligohydramnios of renal origin: long-term outcome. Nephrol Dial Transplant. 2007; 22(2):432–439. PMID: 17065192.
Article3. Gribouval O, Gonzales M, Neuhaus T, Aziza J, Bieth E, Laurent N, et al. Mutations in genes in the renin-angiotensin system are associated with autosomal recessive renal tubular dysgenesis. Nat Genet. 2005; 37(9):964–968. PMID: 16116425.
Article4. Gubler MC, Antignac C. Renin-angiotensin system in kidney development: renal tubular dysgenesis. Kidney Int. 2010; 77(5):400–406. PMID: 19924102.
Article5. Plazanet C, Arrondel C, Chavant F, Gubler MC. Fetal renin-angiotensin-system blockade syndrome: renal lesions. Pediatr Nephrol. 2014; 29(7):1221–1230. PMID: 24477978.
Article6. Vivante A, Kohl S, Hwang DY, Dworschak GC, Hildebrandt F. Single-gene causes of congenital anomalies of the kidney and urinary tract (CAKUT) in humans. Pediatr Nephrol. 2014; 29(4):695–704. PMID: 24398540.
Article7. Lee KH, Gee HY, Shin JI. Genetics of vesicoureteral reflux and congenital anomalies of the kidney and urinary tract. Investig Clin Urol. 2017; 58(Suppl 1):S4–S13.
Article8. Yosypiv IV. Renin-angiotensin system in ureteric bud branching morphogenesis: implications for kidney disease. Pediatr Nephrol. 2014; 29(4):609–620. PMID: 24061643.
Article9. Lacoste M, Cai Y, Guicharnaud L, Mounier F, Dumez Y, Bouvier R, et al. Renal tubular dysgenesis, a not uncommon autosomal recessive disorder leading to oligohydramnios: role of the Renin-Angiotensin system. J Am Soc Nephrol. 2006; 17(8):2253–2263. PMID: 16790508.
Article10. Gubler MC. Renal tubular dysgenesis. Pediatr Nephrol. 2014; 29(1):51–59. PMID: 23636579.
Article11. Fiselier TJ, Lijnen P, Monnens L, van Munster P, Jansen M, Peer P. Levels of renin, angiotensin I and II, angiotensin-converting enzyme and aldosterone in infancy and childhood. Eur J Pediatr. 1983; 141(1):3–7. PMID: 6315441.
Article12. Gribouval O, Morinière V, Pawtowski A, Arrondel C, Sallinen SL, Saloranta C, et al. Spectrum of mutations in the renin-angiotensin system genes in autosomal recessive renal tubular dysgenesis. Hum Mutat. 2012; 33(2):316–326. PMID: 22095942.
Article13. Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17(5):405–424. PMID: 25741868.
Article14. Ruf K, Wirbelauer J, Beissert A, Frieauff E. Successful treatment of severe arterial hypotension and anuria in a preterm infant with renal tubular dysgenesis- a case report. Matern Health Neonatol Perinatol. 2018; 4(1):27. PMID: 30598831.
Article15. Miyawaki M, Okutani T, Higuchi R, Yoshikawa N. Plasma angiotensin II concentrations in the early neonatal period. Arch Dis Child Fetal Neonatal Ed. 2006; 91(5):F359–62. PMID: 16595591.
Article16. Bergmann C. ARPKD and early manifestations of ADPKD: the original polycystic kidney disease and phenocopies. Pediatr Nephrol. 2015; 30(1):15–30. PMID: 24584572.
Article17. Wiesel A, Queisser-Luft A, Clementi M, Bianca S, Stoll C, Group ES, et al. Prenatal detection of congenital renal malformations by fetal ultrasonographic examination: an analysis of 709,030 births in 12 European countries. Eur J Med Genet. 2005; 48(2):131–144. PMID: 16053904.
Article18. Richer J, Daoud H, Geier P, Jarinova O, Carson N, Feberova J, et al. Resolution of refractory hypotension and anuria in a premature newborn with loss-of-function of ACE. Am J Med Genet A. 2015; 167(7):1654–1658. PMID: 25899979.
Article