Ann Rehabil Med.
2020 Aug;44(4):284-291. 10.5535/arm.19165.
Preliminary Clinical Trial of Balance Compensation System for Improvement of Balance in Patients With Spinocerebellar Ataxia
- Affiliations
-
- 1Department of Rehabilitation Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Yonsei Institute of Sports Science and Exercise Medicine, Wonju, Korea
- 3Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2505388
- DOI: http://doi.org/10.5535/arm.19165
Abstract
Objective
To determine the immediate and short-term impact of the application of wearable balance compensation system (BCS) on balance impairment in patients with spinocerebellar ataxia (SCA).
Methods
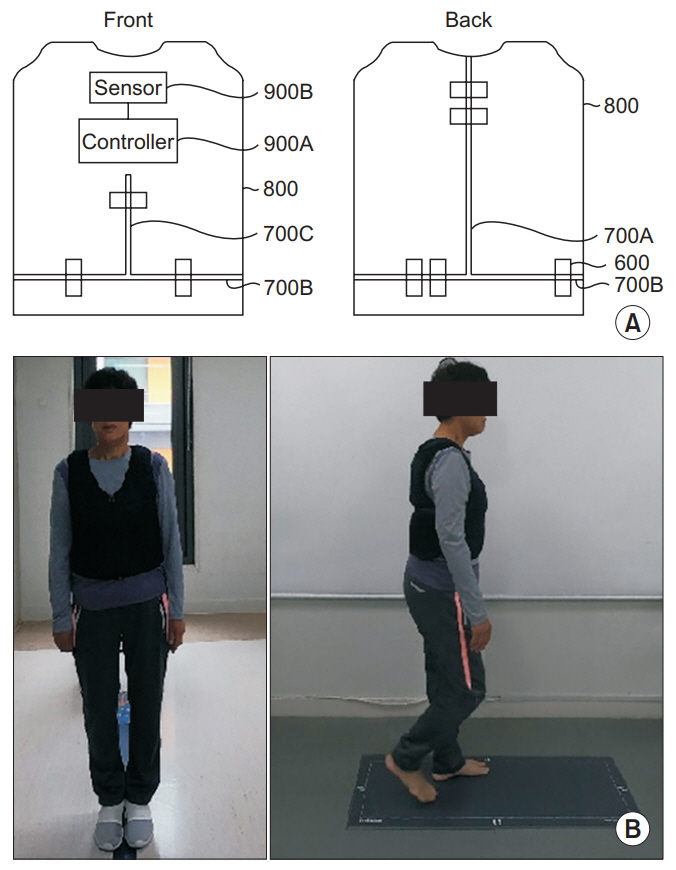
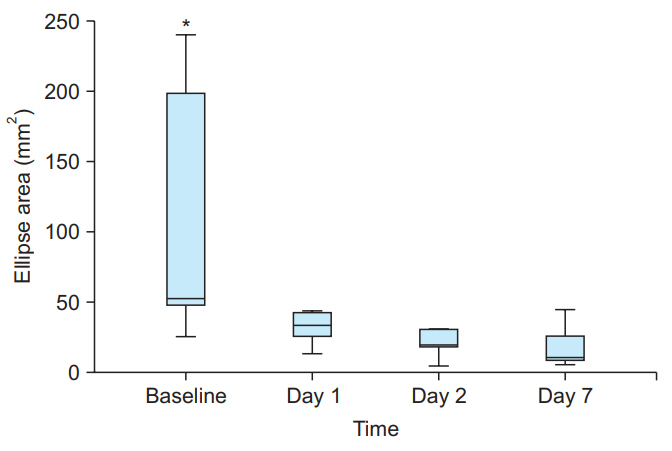
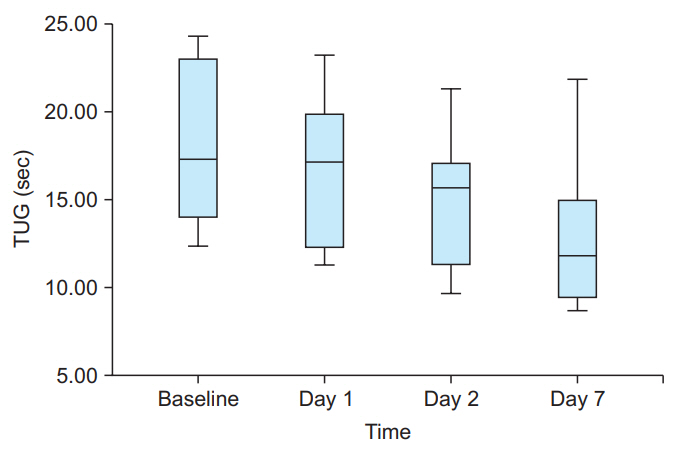
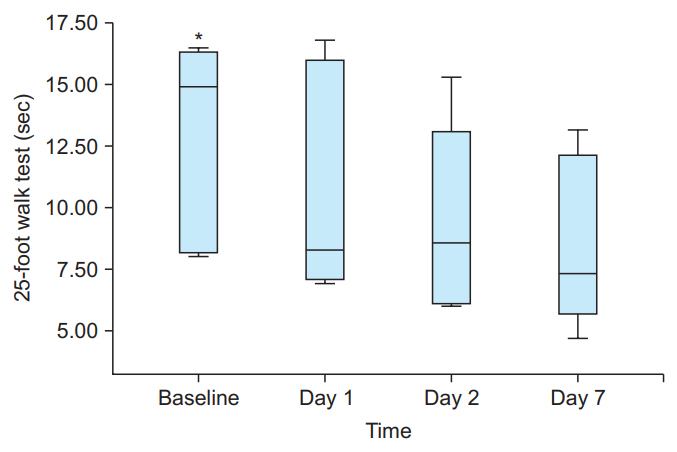
The study enrolled 6 participants with SCA with varying degrees of balance impairment. After adjustment for individual fitting, wearable BCS with up to 3% body weight was placed in a garment on the trunk. Sway direction and magnitude were measured with sensors placed posteriorly at the lumbosacral junction, immediately before and after, and at day 1, day 2, and day 7 after wearing the BCS. Timed Up & Go test (TUG) and 25-foot timed walk test were performed, and static foot pressure was measured.
Results
A significant improvement in static and dynamic balance was found during the 25-foot timed walk and in static foot pressure measurement results after wearing the BCS, when compared with that at baseline (p=0.044 vs. p=0.011). Anterior and posterior sway showed improvements from baseline after wearing the BCS. Improvement in the lateral swaying movement control was also seen.
Conclusion
Application of the BCS might be beneficial in the improvement ofthe static and dynamic balance in patients with SCA. Further research on long-term effects and with a larger sample size is indicated.
Figure
Reference
-
1. Marquer A, Barbieri G, Perennou D. The assessment and treatment of postural disorders in cerebellar ataxia: a systematic review. Ann Phys Rehabil Med. 2014; 57:67–78.
Article2. Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, et al. Prospective analysis of falls in dominant ataxias. Eur Neurol. 2013; 69:53–7.
Article3. Gaxatte C, Nguyen T, Chourabi F, Salleron J, Pardessus V, Delabriere I, et al. Fear of falling as seen in the multidisciplinary falls consultation. Ann Phys Rehabil Med. 2011; 54:248–58.
Article4. Ioffe ME, Chernikova LA, Ustinova KI. Role of cerebellum in learning postural tasks. Cerebellum. 2007; 6:87–94.
Article5. Manto M. The cerebellum, cerebellar disorders, and cerebellar research: two centuries of discoveries. Cerebellum. 2008; 7:505–16.6. Weinshenker BG, Issa M, Baskerville J. Long-term and short-term outcome of multiple sclerosis: a 3-year follow-up study. Arch Neurol. 1996; 53:353–8.7. Rodgers MM, Mulcare JA, King DL, Mathews T, Gupta SC, Glaser RM. Gait characteristics of individuals with multiple sclerosis before and after a 6-month aerobic training program. J Rehabil Res Dev. 1999; 36:183–8.8. Taylor NF, Dodd KJ, Prasad D, Denisenko S. Progressive resistance exercise for people with multiple sclerosis. Disabil Rehabil. 2006; 28:1119–26.
Article9. Gutierrez GM, Chow JW, Tillman MD, McCoy SC, Castellano V, White LJ. Resistance training improves gait kinematics in persons with multiple sclerosis. Arch Phys Med Rehabil. 2005; 86:1824–9.
Article10. White LJ, McCoy SC, Castellano V, Gutierrez G, Stevens JE, Walter GA, et al. Resistance training improves strength and functional capacity in persons with multiple sclerosis. Mult Scler. 2004; 10:668–74.11. Wiles CM, Newcombe RG, Fuller KJ, Shaw S, Furnival-Doran J, Pickersgill TP, et al. Controlled randomised crossover trial of the effects of physiotherapy on mobility in chronic multiple sclerosis. J Neurol Neurosurg Psychiatry. 2001; 70:174–9.
Article12. Lord SE, Wade DT, Halligan PW. A comparison of two physiotherapy treatment approaches to improve walking in multiple sclerosis: a pilot randomized controlled study. Clin Rehabil. 1998; 12:477–86.
Article13. Smedal T, Lygren H, Myhr KM, Moe-Nilssen R, Gjelsvik B, Gjelsvik O, et al. Balance and gait improved in patients with MS after physiotherapy based on the Bobath concept. Physiother Res Int. 2006; 11:104–16.
Article14. Chase RA, Cullen JK Jr, Sullivan SA, Ommaya AK. Modification of intention tremor in man. Nature. 1965; 206:485–7.
Article15. Hewer RL, Cooper R, Morgan MH. An investigation into the value of treating intention tremor by weighting the affected limb. Brain. 1972; 95:579–90.
Article16. Morgan MH, Hewer RL, Cooper R. Application of an objective method of assessing intention tremor: a further study on the use of weights to reduce intention tremor. J Neurol Neurosurg Psychiatry. 1975; 38:259–64.17. Morgan MH. Ataxia and weights. Physiotherapy. 1975; 61:332–4.18. Clopton N, Schultz D, Boren C, Porter J, Brillbart T. Effects of axial weight loading on gait for subjects with cerebellar ataxia: preliminary findings. Neurol Rep. 2003; 27:15–21.19. Lucy SD, Hayes KC. Postural sway profiles: normal subjects and subjects with cerebellar ataxia. Physiother Can. 1985; 37:140–8.20. Crittendon A, O’Neill D, Widener GL, Allen DD. Standing data disproves biomechanical mechanism for balance-based torso-weighting. Arch Phys Med Rehabil. 2014; 95:43–9.
Article21. Widener GL, Allen DD, Gibson-Horn C. Randomized clinical trial of balance-based torso weighting for improving upright mobility in people with multiple sclerosis. Neurorehabil Neural Repair. 2009; 23:784–91.
Article22. Hunt CM, Widener G, Allen DD. Variability in postural control with and without balance-based torsoweighting in people with multiple sclerosis and healthy controls. Phys Ther. 2014; 94:1489–98.23. Holmes G. The cerebellum of man. Brain. 1939; 62:1–30.
Article24. Widener GL, Allen DD, Gibson-Horn C. Balancebased torso-weighting may enhance balance in persons with multiple sclerosis: preliminary evidence. Arch Phys Med Rehabil. 2009; 90:602–9.
Article25. Goff B. The application of recent advances in neurophysiology to Miss M. Rood’s concept of neuromuscular facilitation. Physiotherapy. 1972; 58:409–15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinocerebellar Ataxia Type 8 Presenting as Ataxia without Definite Cerebellar Atrophy
- The Changes of Postural Balance in Patients with Total Hip Arthroplasty
- Balance in Patients After TKA
- A Case of Spinocerebellar Ataxia Type 7 with Torticollis
- A Patient with Spinocerebellar Ataxia 2 Presenting with Multiple System Atrophy