Ann Hepatobiliary Pancreat Surg.
2020 Aug;24(3):373-380. 10.14701/ahbps.2020.24.3.373.
Retroduodenal resection of the extrahepatic common bile duct with in situ re-implantation of the main pancreatic duct:A report of two cases
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2505354
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.373
Abstract
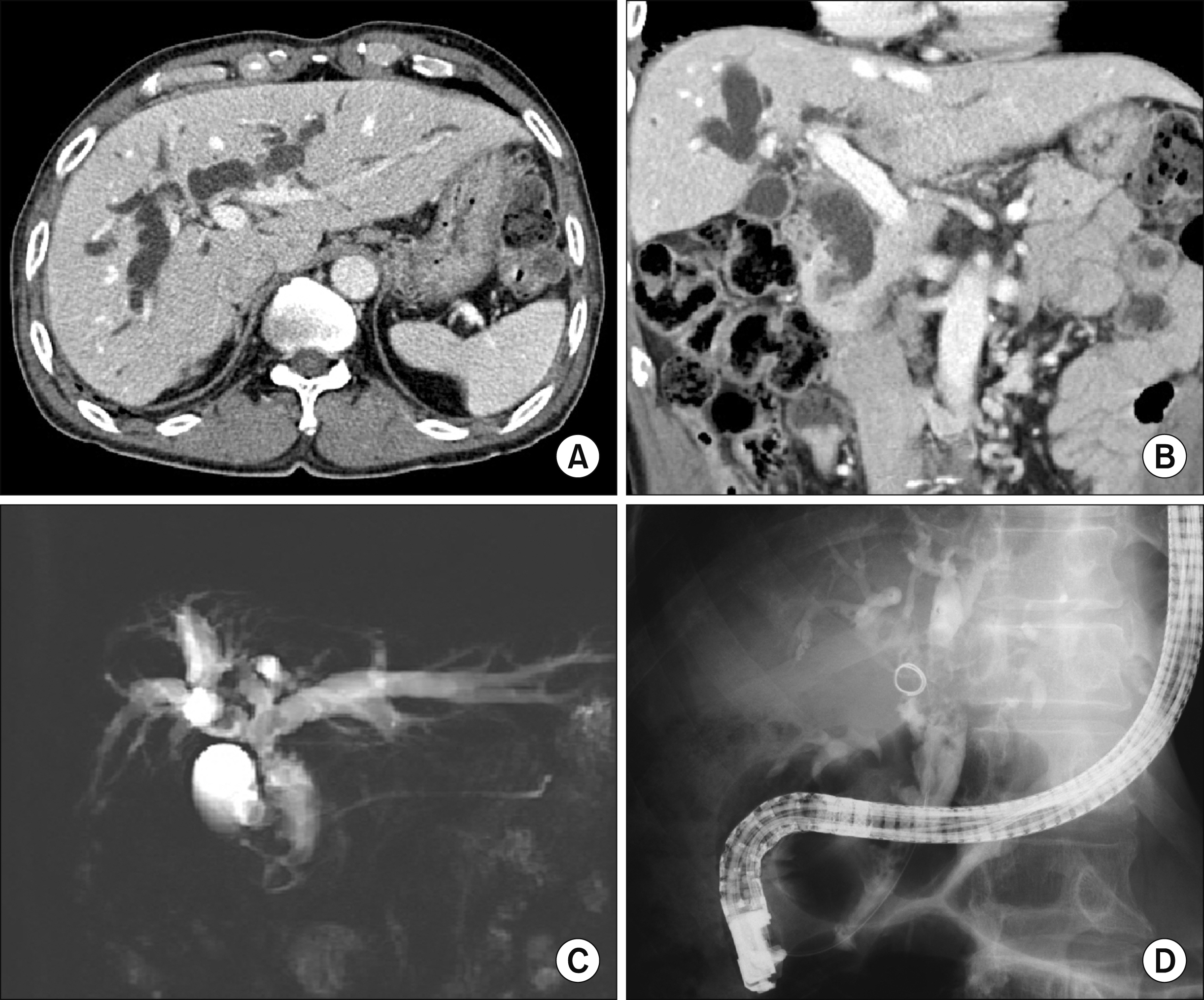
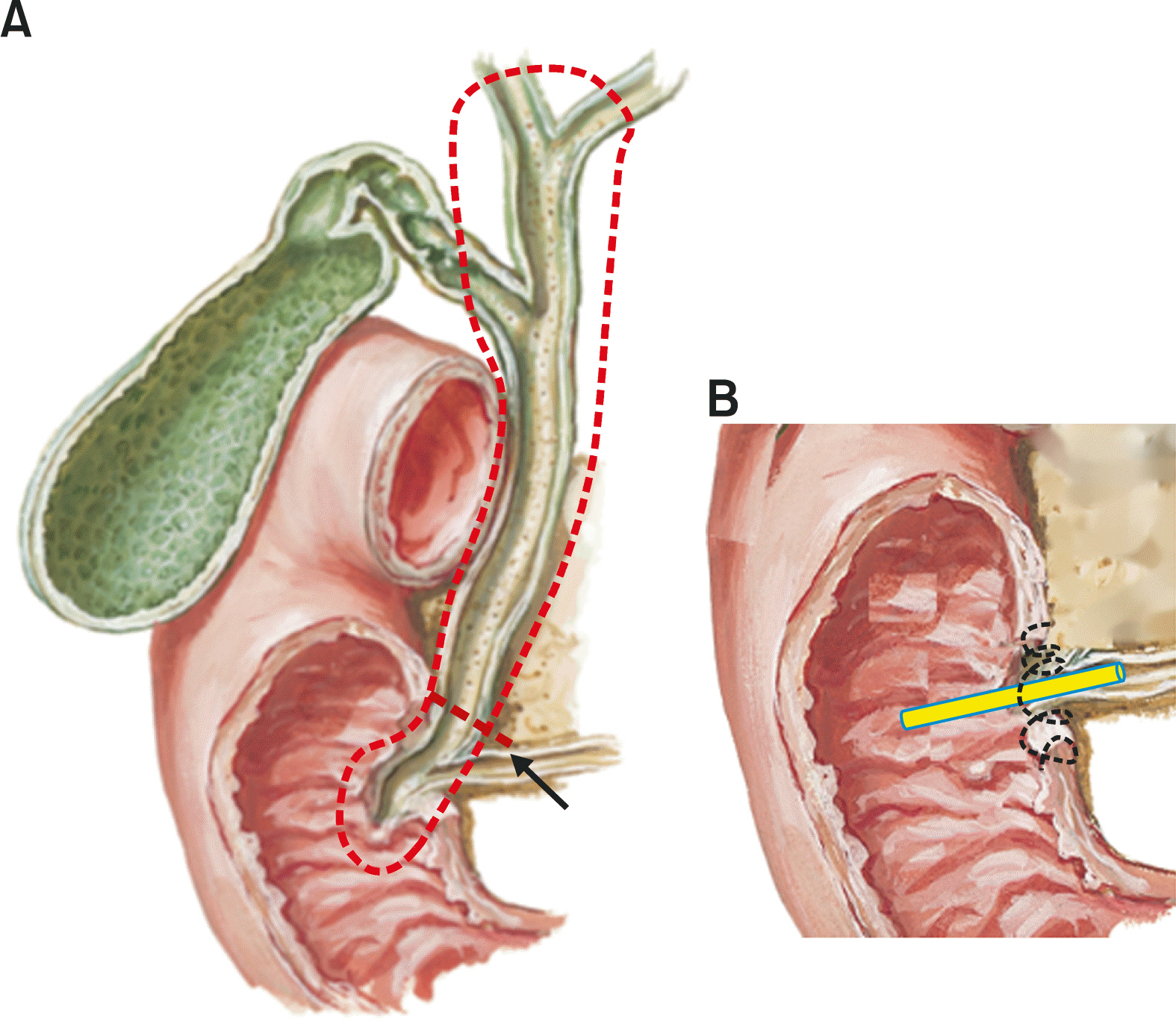
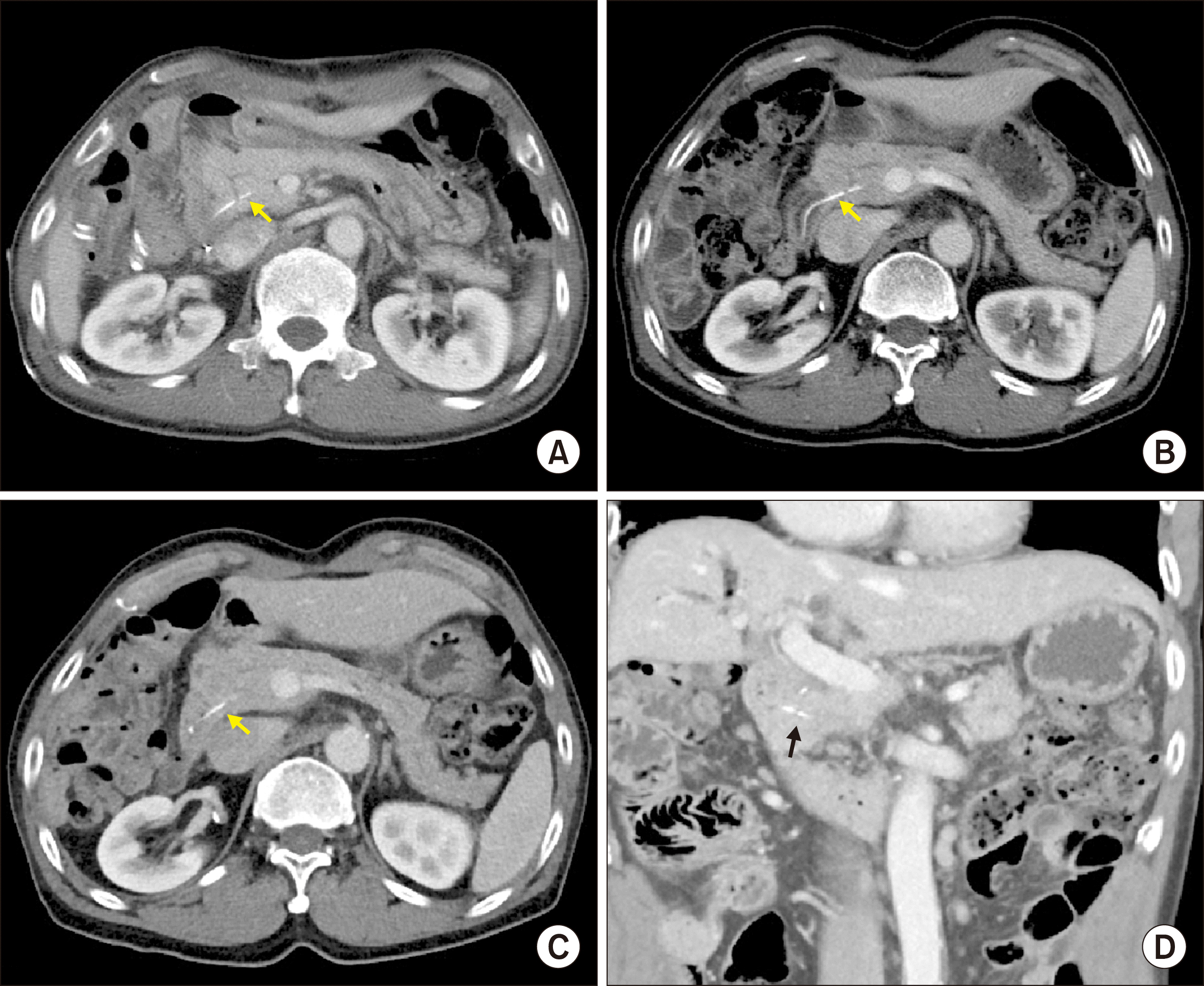
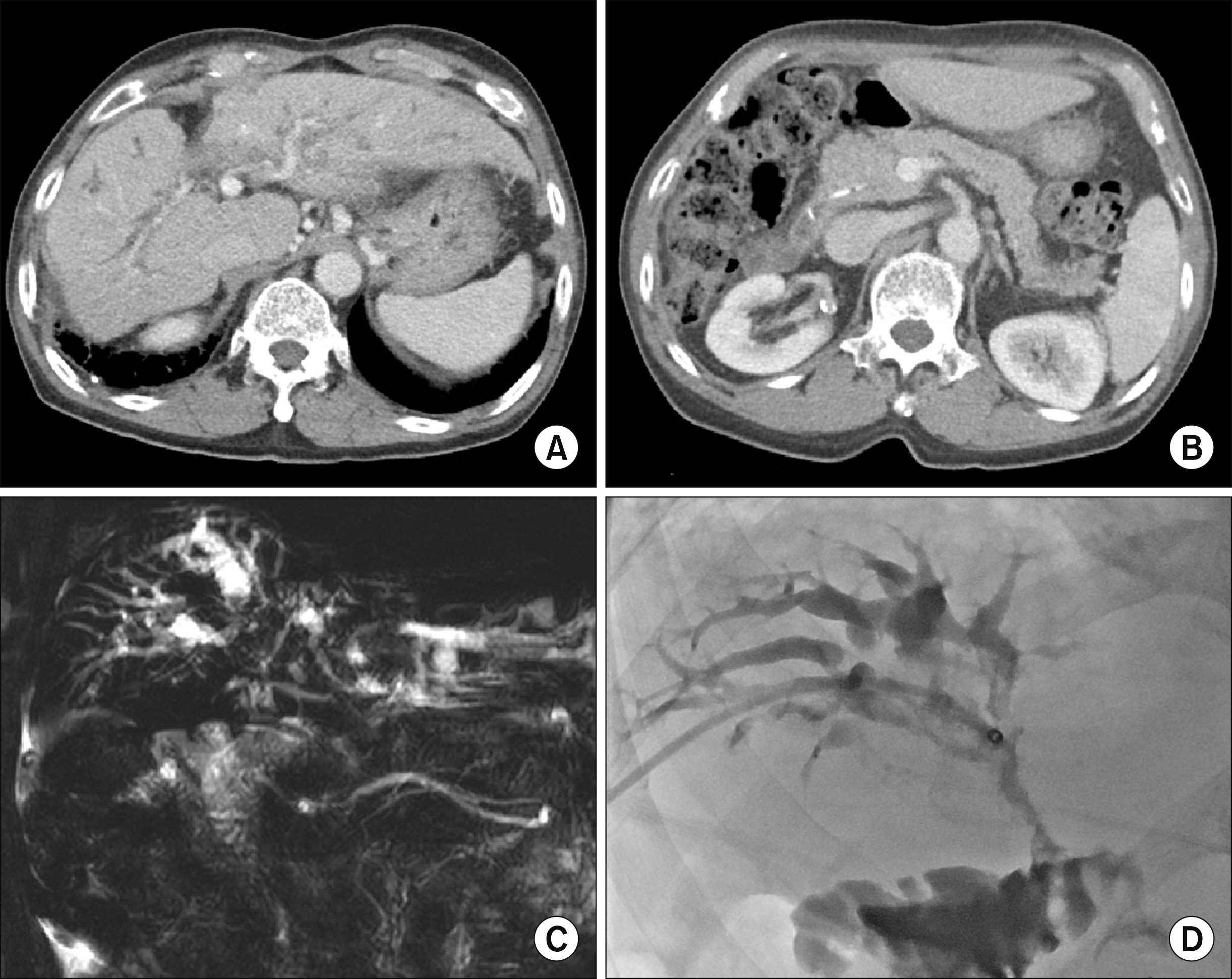
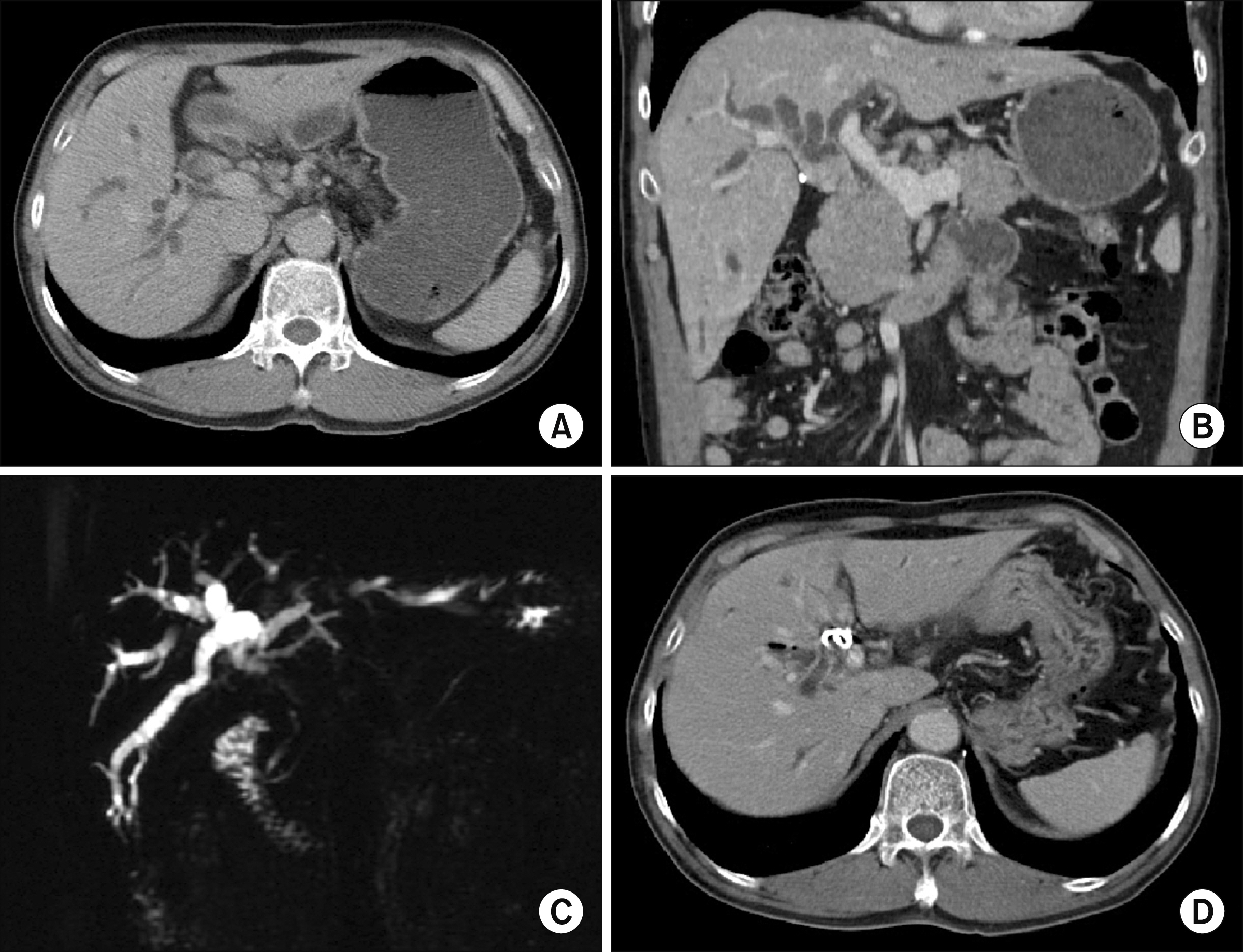
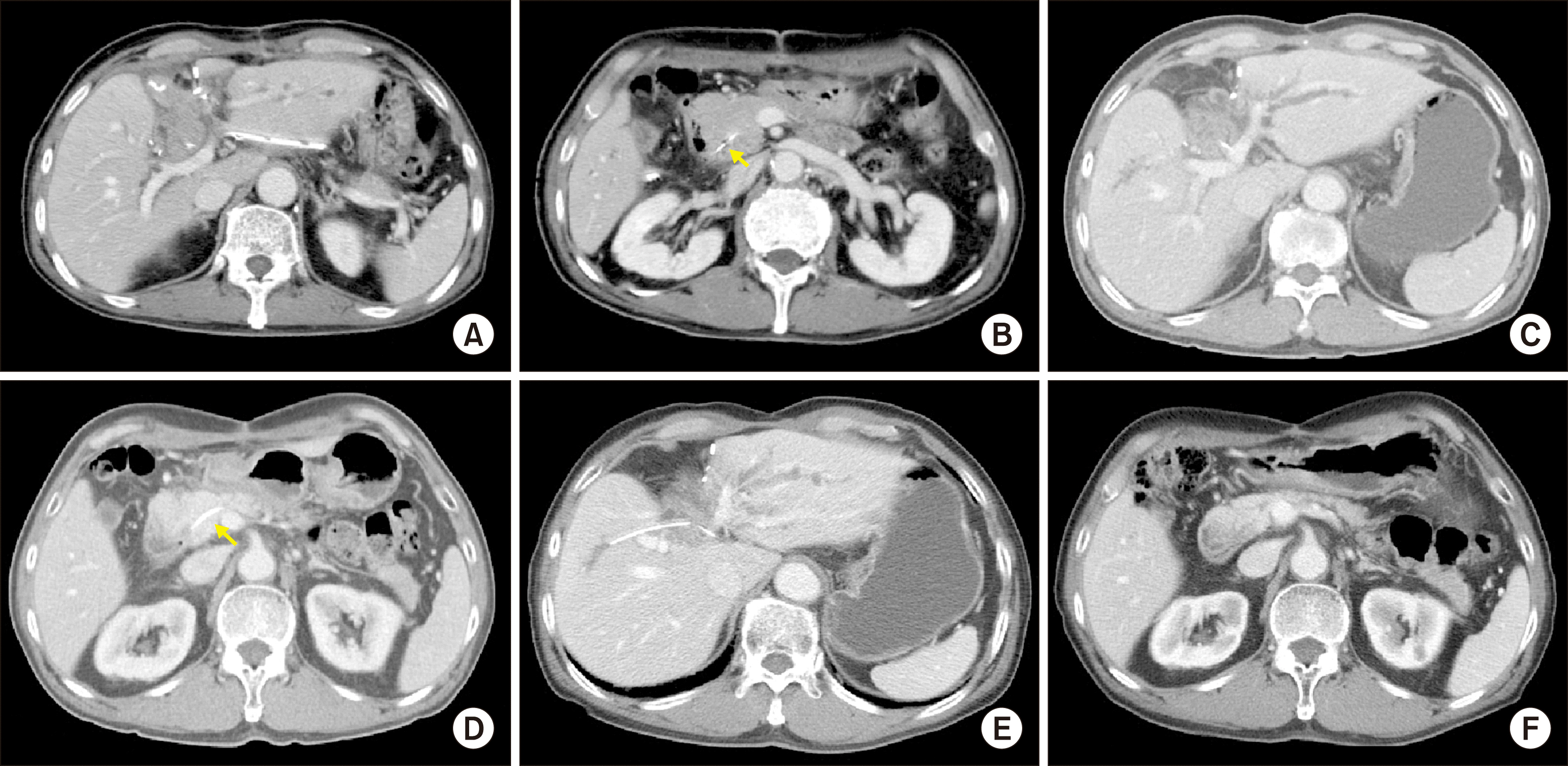
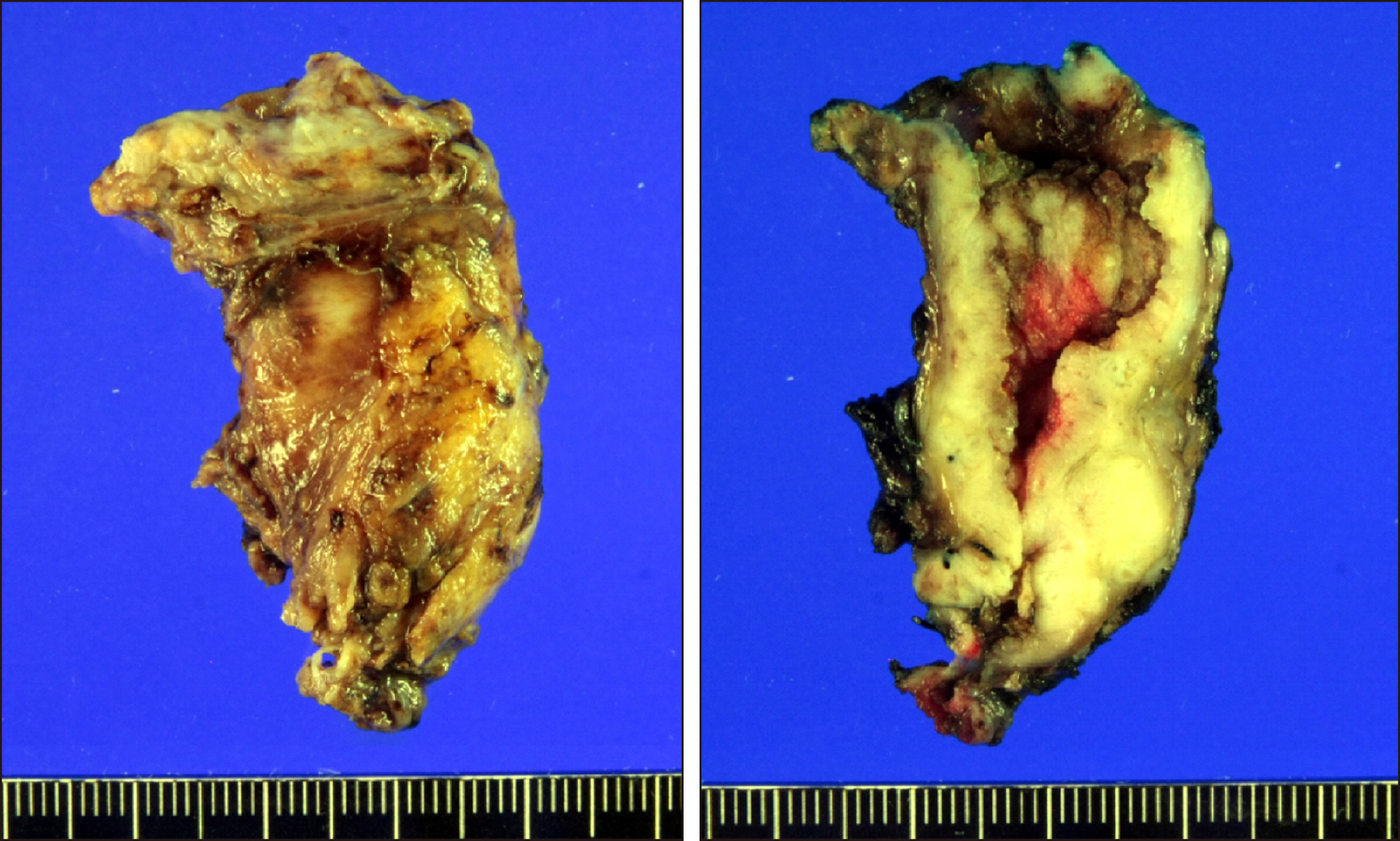
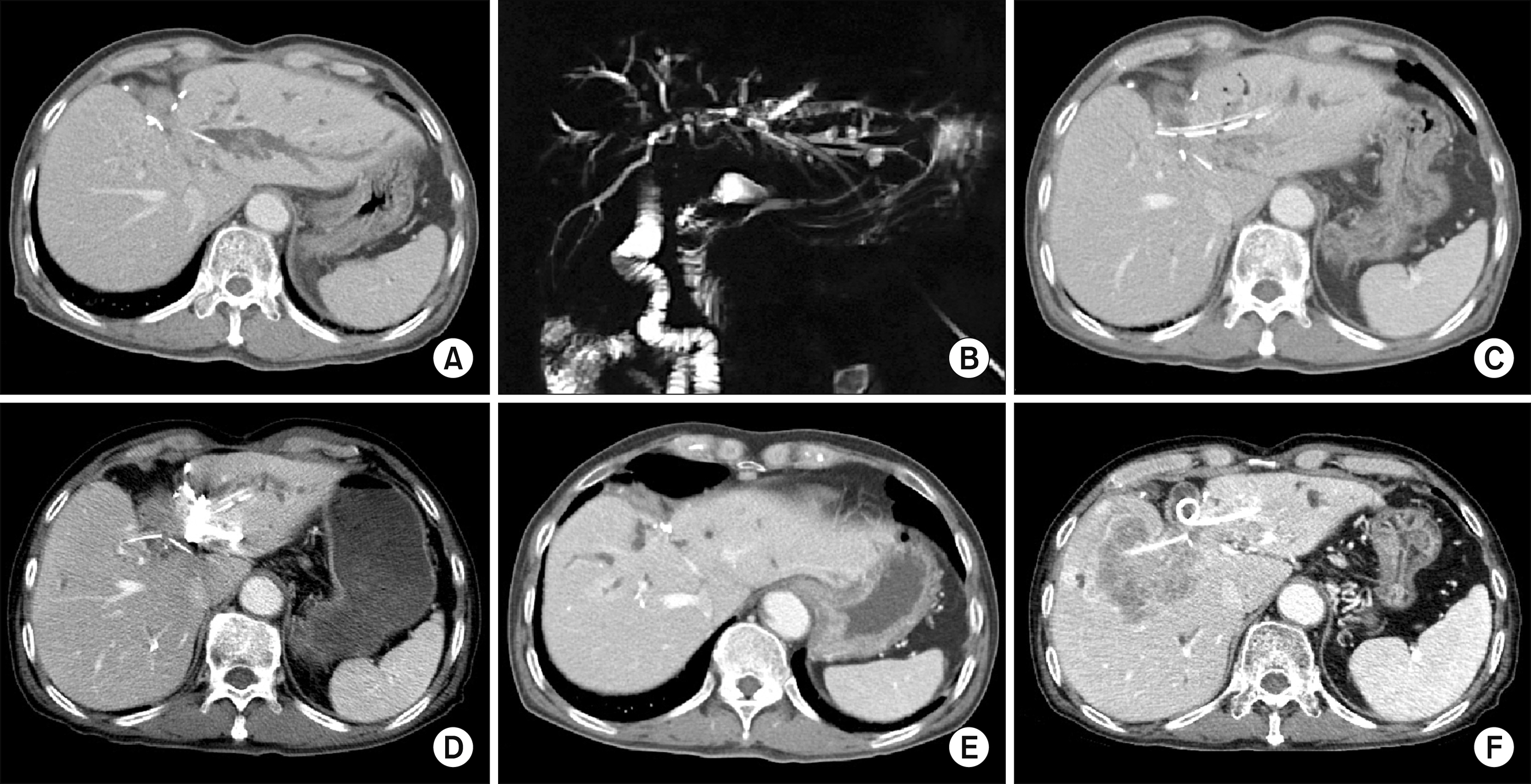
- Resection of the whole distal common bile duct (CBD) with in situ re-implantation of the main pancreatic duct can be a surgical option to avoid pancreaticoduodenectomy. in this study, we present two cases of cholangiocarcinomas with diffuse involvement of the extrahepatic CBD that was resected through a retroduodenal approach and re-implantation of the main pancreatic duct. The first case was a 70-year-old male patient with intraductal papillary neoplasm with invasive cholangiocarcinoma. He underwent retroduodenal resection of the whole CBD and in situ re-implantation of the main pancreatic duct. He was disease-free for 8 years, but tumor recurrence occurred at the hepaticojejunostomy site. This patient is currently undergoing chemoradiation therapy for treatment of recurrent lesions. The second case was a 71-year-old male patient with diffuse cholangiocarcinoma involving the whole extrahepatic CBD. He underwent medial sectionectomy, retroduodenal resection of the whole CBD and in situ re-implantation of the main pancreatic duct. He received postoperative chemoradiation therapy. He was disease-free for 3 years, but tumor recurrence occurred at the hepaticojejunostomy site. He passed away 4 years and 6 months after surgery. In conclusion, complete resection of the extrahepatic CBD through a retroduodenal approach with in situ re-implantation of the main pancreatic duct is feasible and less invasive than PD. Therefore, the proposed less-invasive approach can be an alternative procedure in selected patients requiring complete resection of the distal CBD.
Keyword
Figure
Reference
-
1. Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, Thomas HC. 2002; Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol. 37:806–813. DOI: 10.1016/S0168-8278(02)00297-0. PMID: 12445422.
Article2. Murakami Y, Uemura K, Sudo T, Hashimoto Y, Nakashima A, Kondo N, et al. 2011; Prognostic factors after surgical resection for intrahepatic, hilar, and distal cholangiocarcinoma. Ann Surg Oncol. 18:651–658. DOI: 10.1245/s10434-010-1325-4. PMID: 20945107.
Article3. Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, et al. 2005; Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 137:396–402. DOI: 10.1016/j.surg.2004.10.008. PMID: 15800484.
Article4. Hong SM, Pawlik TM, Cho H, Aggarwal B, Goggins M, Hruban RH, et al. 2009; Depth of tumor invasion better predicts prognosis than the current American Joint Committee on Cancer T classification for distal bile duct carcinoma. Surgery. 146:250–257. DOI: 10.1016/j.surg.2009.02.023. PMID: 19628081. PMCID: PMC3402913.
Article5. Rizvi S, Khan SA, Hallemeier CL, Kelley RK, Gores GJ. 2018; Cholangiocarcinoma - evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 15:95–111. DOI: 10.1038/nrclinonc.2017.157. PMID: 28994423. PMCID: PMC5819599.
Article6. Sahai P, Kumar S. 2017; External radiotherapy and brachytherapy in the management of extrahepatic and intrahepatic cholangiocarcinoma: available evidence. Br J Radiol. 90:20170061. DOI: 10.1259/bjr.20170061. PMID: 28466653. PMCID: PMC5603950.
Article7. Kiriyama M, Ebata T, Aoba T, Kaneoka Y, Arai T, Shimizu Y, et al. 2015; Prognostic impact of lymph node metastasis in distal cholangiocarcinoma. Br J Surg. 102:399–406. DOI: 10.1002/bjs.9752. PMID: 25611179.8. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. 2014; A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 259:773–780. DOI: 10.1097/SLA.0000000000000263. PMID: 24253151.9. Addeo P, Delpero JR, Paye F, Oussoultzoglou E, Fuchshuber PR, Sauvanet A, et al. 2014; Pancreatic fistula after a pancreaticoduodenectomy for ductal adenocarcinoma and its association with morbidity: a multicentre study of the French Surgical Association. HPB (Oxford). 16:46–55. DOI: 10.1111/hpb.12063. PMID: 23461663. PMCID: PMC3892314.
Article10. Sugimoto M, Takahashi S, Gotohda N, Kato Y, Kinoshita T, Shibasaki H, et al. 2013; Schematic pancreatic configuration: a risk assessment for postoperative pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg. 17:1744–1751. DOI: 10.1007/s11605-013-2320-4. PMID: 23975030.
Article11. Hwang S, Lee SG, Kim KH, Ahn CS, Moon DB, Ha TY, et al. 2008; Extended extrahepatic bile duct resection to avoid performing pancreatoduodenectomy in patients with mid bile duct cancer. Dig Surg. 25:74–79. DOI: 10.1159/000118025. PMID: 18292664.
Article12. Lee SJ, Hwang S, Ha TY, Kim KH, Ahn CS, Moon DB, et al. 2013; Technical knacks and outcomes of extended extrahepatic bile duct resection in patients with mid bile duct cancer. Korean J Hepatobiliary Pancreat Surg. 17:109–112. DOI: 10.14701/kjhbps.2013.17.3.109. PMID: 26155223. PMCID: PMC4304529.
Article13. Hwang S, Jung DJ, Ha TY. 2020; Application of suction-type cigarette drain in leak-prone hepatopancreatobiliary surgery. Ann Hepatobiliary Pancreat Surg. 24:305–308. DOI: 10.14701/ahbps.2020.24.3.305. PMID: 32843596.
Article14. Kolb A, Kleeff J, Frohlich B, Werner J, Friess H, Büchler MW. 2009; Resection of the intrapancreatic bile duct preserving the pancreas. J Hepatobiliary Pancreat Surg. 16:31–34. DOI: 10.1007/s00534-008-0013-2. PMID: 19089312.
Article15. Hwang S, Moon KM, Park JI, Kim MH, Lee SG. 2007; Retroduodenal resection of ampullary carcinoid tumor in a patient with cavernous transformation of the portal vein. J Gastrointest Surg. 11:1322–1327. DOI: 10.1007/s11605-007-0240-x. PMID: 17674113.
Article16. Nishida Y, Sugimoto M, Kojima M, Gotohda N, Konishi M, Takahashi S. 2017; Pancreas-preserving resection of lower biliary tract adenocarcinoma: a coring-out technique. Ann Gastroenterol Surg. 1:150–155. DOI: 10.1002/ags3.12021. PMID: 29863138. PMCID: PMC5881344.
Article17. Kim JK, Hwang HK, Park JS, Cho SI, Yoon DS, Chi HS. 2008; Left hemihepatectomy and caudate lobectomy and complete extrahepatic bile duct resection using transduodenal approach for hilar cholangiocarcinoma arsing from biliary papillomatosis. J Surg Oncol. 98:139–142. DOI: 10.1002/jso.21089. PMID: 18521837.
Article18. Hong S, Song KB, Lee YJ, Park KM, Kim SC, Hwang DW, et al. 2018; Transduodenal ampullectomy for ampullary tumors - single center experience of consecutive 26 patients. Ann Surg Treat Res. 95:22–28. DOI: 10.4174/astr.2018.95.1.22. PMID: 29963536. PMCID: PMC6024084.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent pyogenic cholangitis: The pattern of thickening of the extrahepatic bile duct on CT
- Extrahepatic Bile Duct Duplication with Intraductal Papillary Neoplasm: A Case Report
- A Case of Multiple Papillary Adenocarcinoma of the Extrahepatic Bile Duct : Findings of ERCP
- Intrahepatic Bile Duct Dilatation Caused by Pancreatic Pseudocyst: A Case Report
- Two Cases of Anomalous Termination of the Common Bile Duct and the Pancreatic Duct into the Duodenal Bulb