Ann Hepatobiliary Pancreat Surg.
2020 Aug;24(3):339-344. 10.14701/ahbps.2020.24.3.339.
Hepatic atrophy treatment with portal vein embolization to control intrahepatic duct stenosis-associated cholangitis
- Affiliations
-
- 1Departments of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Departments of Diagnostic Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2505348
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.339
Abstract
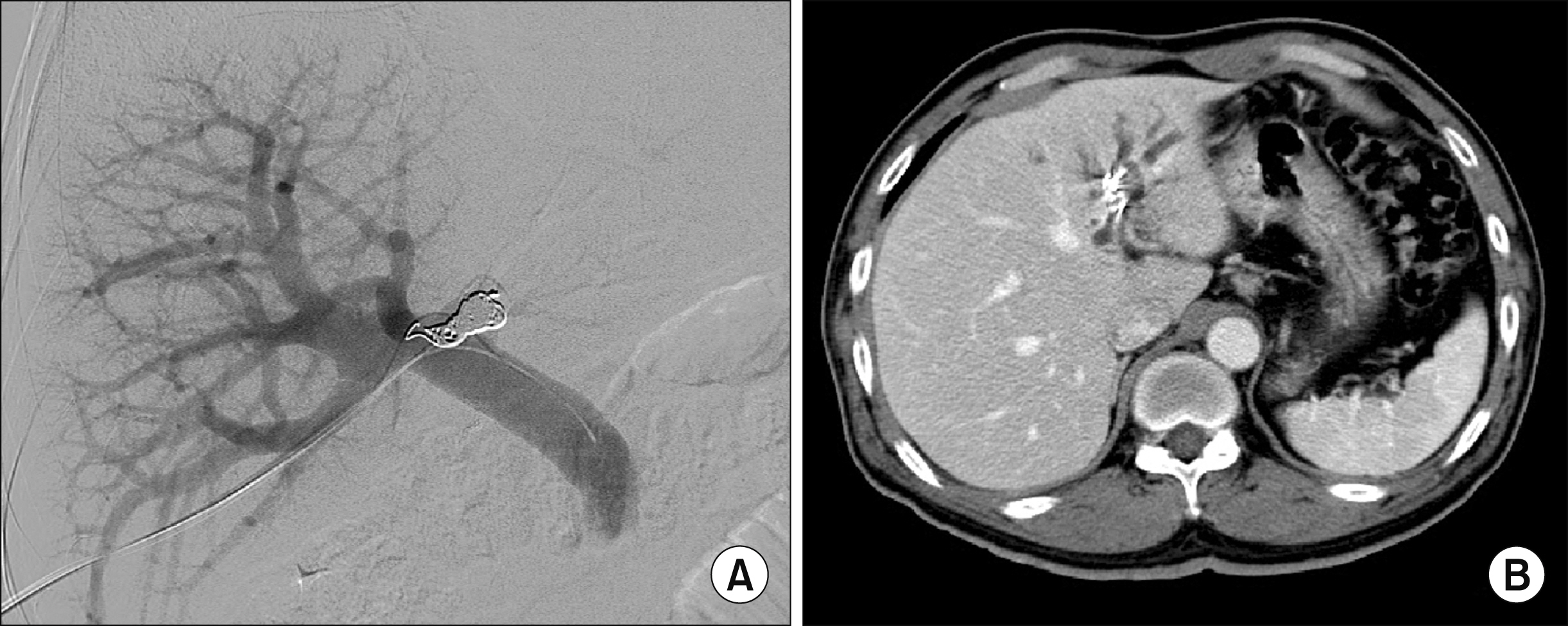
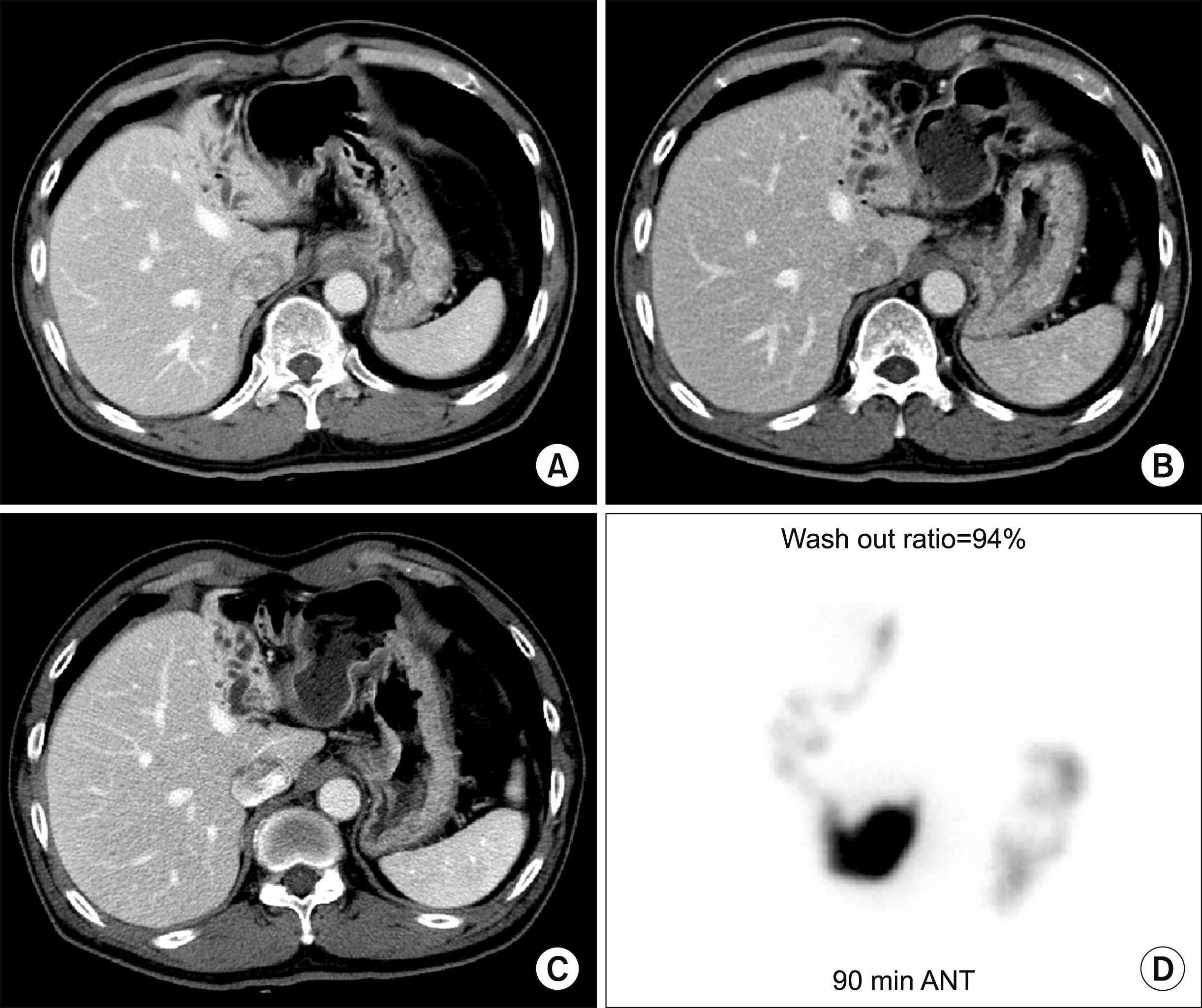
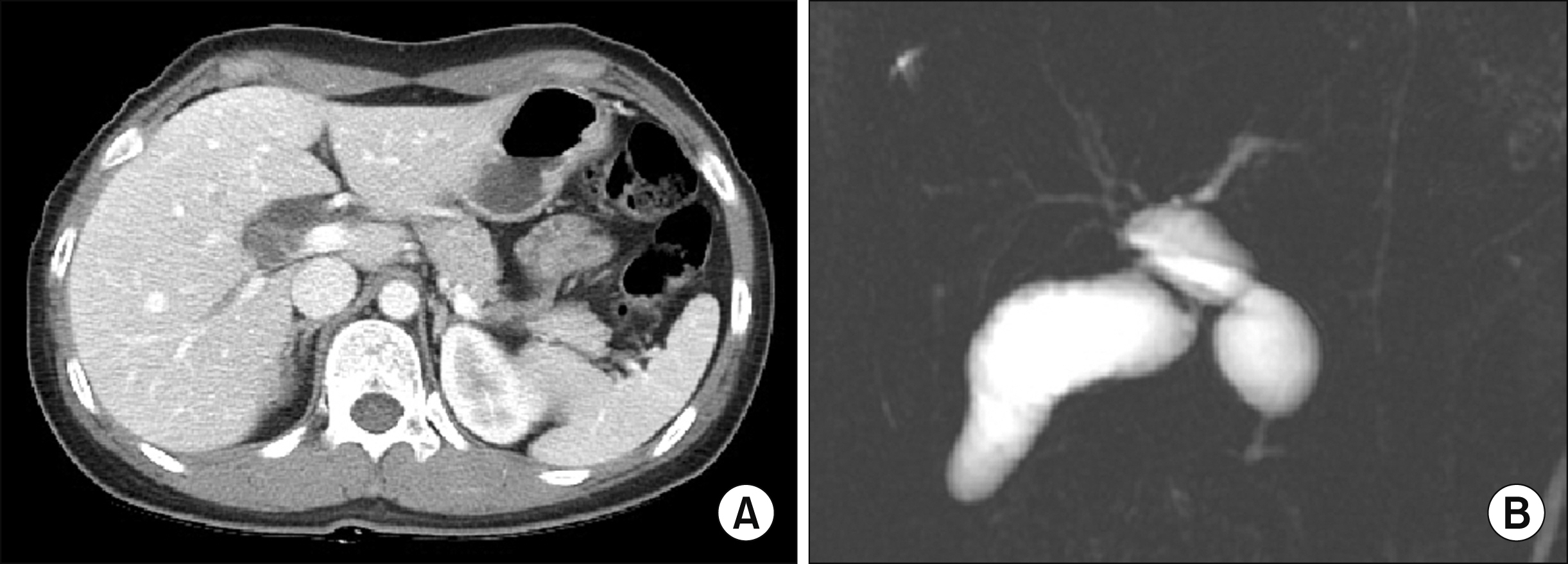
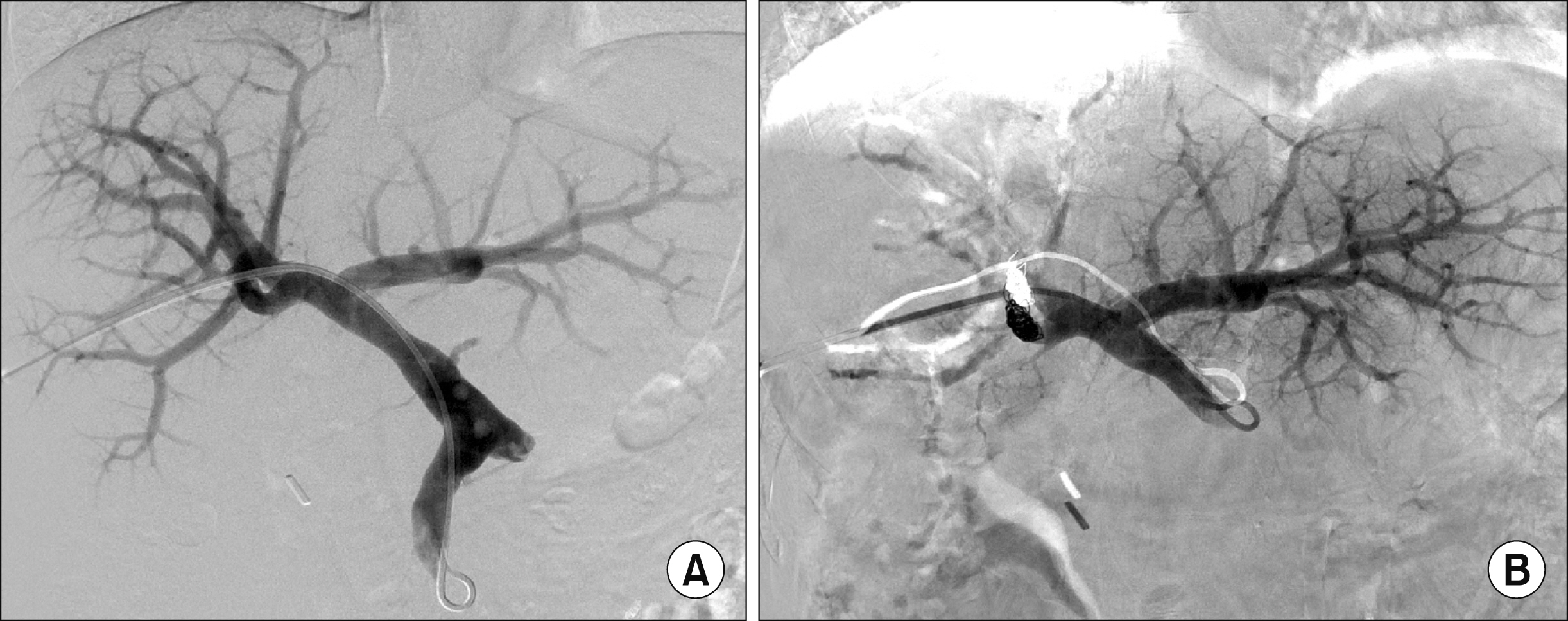
- We present two cases of hepatic atrophy treatment with portal vein embolization (PVE) to control intractable cholangitis. The first case was a 60-year-old male who was admitted for repeated episodes of cholangitis. He had undergone cholecystectomy and Roux-en-Y choledochojejunostomy 2 years earlier. Imaging studies showed left intrahepatic duct dilatation and anastomotic site stricture. The patient was reluctant to undergo another surgery. Thus, we decided to perform left PVE to induce atrophy of the left liver. The left liver shrank and stayed silent for 5 years, but a radiological intervention was necessary to treat symptomatic anastomotic stenosis. The patient has done well for 12 years after PVE. The second case was a 51-year-old female who was also admitted for repeated episodes of cholangitis. She had undergone excision of type I choledochal cyst 2 years earlier. Imaging studies showed right hepatic duct stenosis. Cholangitis developed repeatedly. Thus, radiologic interventions were performed 8 times over 9 years. Finally, she was referred for surgery, but she was very reluctant to undergo another surgery. We planned a wait-and-see strategy following right PVE. After PVE, the right liver progressively shrank. Three months after PVE, we decided to wait for a longer period until further atrophy of the right liver. The patient has been doing well for 14 months after PVE without any episode of cholangitis. In conclusion, experience from our two cases suggests that hepatic parenchymal induction therapy through percutaneous PVE can be a therapeutic option for patients with perihilar biliary stenosis-associated cholangitis.
Keyword
Figure
Reference
-
1. Hwang S, Yoon SY, Jung SW, Namgoong JM, Park GC, Gwon DI, et al. 2011; Therapeutic induction of hepatic atrophy for isolated injury of the right posterior sectoral duct following laparoscopic cholecystectomy. Korean J Hepatobiliary Pancreat Surg. 15:189–193. DOI: 10.14701/kjhbps.2011.15.3.189. PMID: 26421038. PMCID: PMC4582538.
Article2. Hwang S, Lee SG, Lee YJ, Ha TY, Ko GY, Song GW. 2007; Delayed-onset isolated injury of the right posterior segment duct after laparoscopic cholecystectomy: a report of hepatic segmental atrophy induction. Surg Laparosc Endosc Percutan Tech. 17:203–205. DOI: 10.1097/SLE.0b013e31804d4488. PMID: 17581468.
Article3. Hwang S, Park GC, Ha TY, Ko GY, Gwon DI, Choi YI, et al. 2012; Hepatic parenchymal atrophy induction for intractable segmental bile duct injury after liver resection. Hepatogastroenterology. 59:866–868. DOI: 10.5754/hge10172. PMID: 22469733.4. Hwang S, Ha TY, Ko GY, Kwon DI, Song GW, Jung DH, et al. 2015; Preoperative sequential portal and hepatic vein embolization in patients with hepatobiliary malignancy. World J Surg. 39:2990–2998. DOI: 10.1007/s00268-015-3194-2. PMID: 26304608.
Article5. Hwang S, Ko GY, Kim MH, Lee SK, Gwon DI, Ha TY, et al. 2016; Preoperative left portal vein embolization for left liver resection in high-risk hepatobiliary malignancy patients. World J Surg. 40:2758–2765. DOI: 10.1007/s00268-016-3618-7. PMID: 27384172.
Article6. Ko GY, Hwang S, Sung KB, Gwon DI, Lee SG. 2010; Interventional oncology: new options for interstitial treatments and intravascular approaches: right hepatic vein embolization after right portal vein embolization for inducing hypertrophy of the future liver remnant. J Hepatobiliary Pancreat Sci. 17:410–412. DOI: 10.1007/s00534-009-0235-y. PMID: 19890603.7. Hwang S, Lee SG, Ko GY, Kim BS, Sung KB, Kim MH, et al. 2009; Sequential preoperative ipsilateral hepatic vein embolization after portal vein embolization to induce further liver regeneration in patients with hepatobiliary malignancy. Ann Surg. 249:608–616. DOI: 10.1097/SLA.0b013e31819ecc5c. PMID: 19300228.
Article8. Yokoyama Y, Nagino M, Nimura Y. 2007; Mechanisms of hepatic regeneration following portal vein embolization and partial hepatectomy: a review. World J Surg. 31:367–374. DOI: 10.1007/s00268-006-0526-2. PMID: 17219273.
Article9. Shindoh J, Truty MJ, Aloia TA, Curley SA, Zimmitti G, Huang SY, et al. 2013; Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg. 216:201–209. DOI: 10.1016/j.jamcollsurg.2012.10.018. PMID: 23219349. PMCID: PMC3632508.
Article10. Uesaka K, Nimura Y, Nagino M. 1996; Changes in hepatic lobar function after right portal vein embolization. An appraisal by biliary indocyanine green excretion. Ann Surg. 223:77–83. DOI: 10.1097/00000658-199601000-00011. PMID: 8554422. PMCID: PMC1235066.11. Hwang S, Lee SG, Lee YJ, Park KM, Choi DR, Kim KH, et al. 1999; Right hepatic lobectomy in the treatment of right-sided hepatolithiasis. J Korean Surg Soc. 57:550–557.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Hepatic Atrophy after Transcatheter Aterial Embolization
- Recurrent Pyogenic Cholangitis: Angiographic Findings and Its Significance
- Atrophy of the Left Hepatic Lobe Caused by a Biliary Tract Disease
- Hepatic Resection for Right-Sided Intrahepatic Stones
- Portal vein embolization in intrahepatic portal vein injury after blunt trauma: a case report