Healthc Inform Res.
2020 Jul;26(3):193-200. 10.4258/hir.2020.26.3.193.
Toolkit to Compute Time-Based Elixhauser Comorbidity Indices and Extension to Common Data Models
- Affiliations
-
- 1Department of Biomedical Informatics, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 2Department of Population Health Sciences, University of Texas Health Science Center at San Antonio, San Antonio, TX, USA
- 3Department of Information Technology, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 4Department of Surgery, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 5Department of Health Policy and Management, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- KMID: 2505260
- DOI: http://doi.org/10.4258/hir.2020.26.3.193
Abstract
Objectives
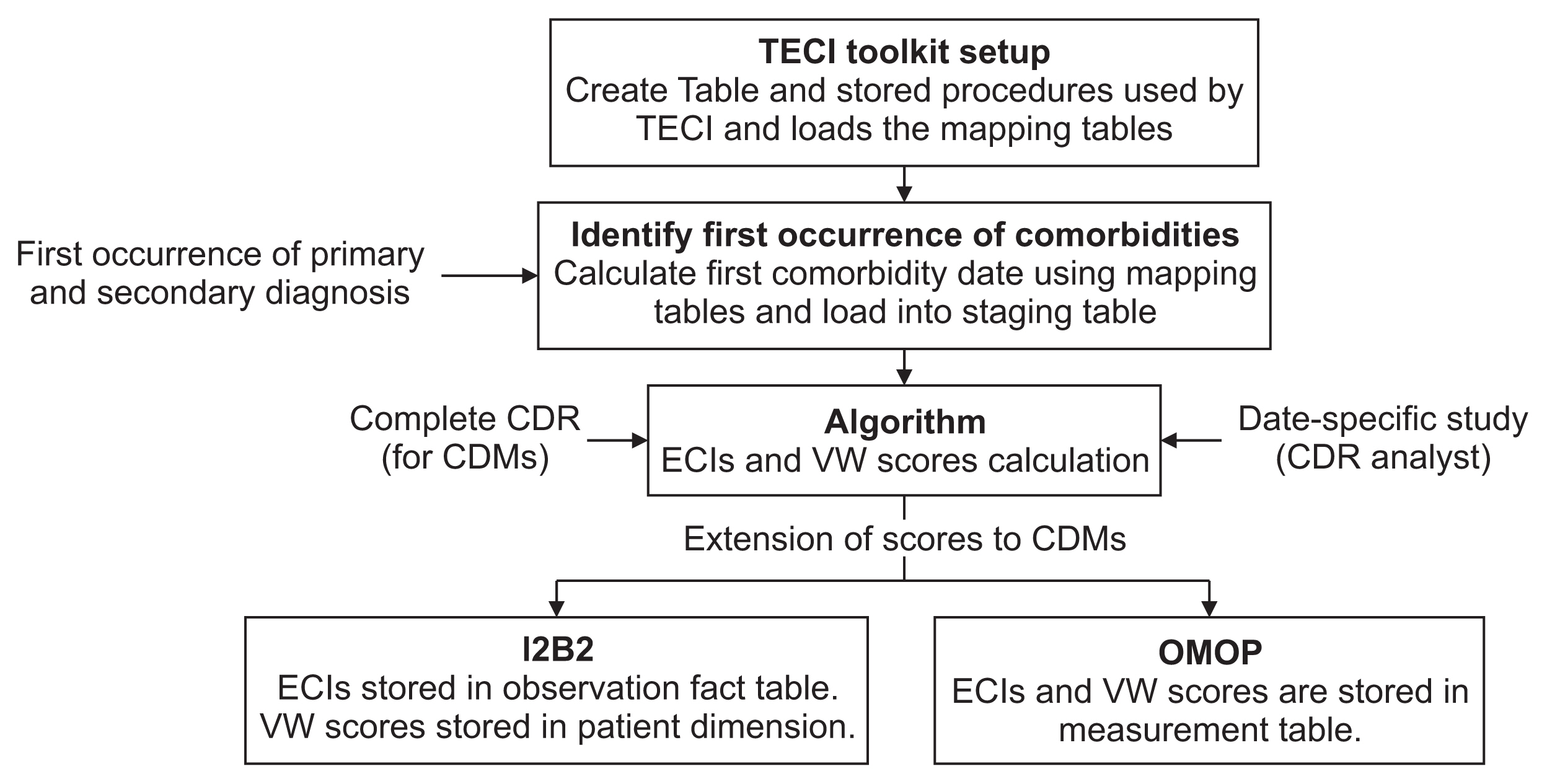
The time-dependent study of comorbidities provides insight into disease progression and trajectory. We hypothesize that understanding longitudinal disease characteristics can lead to more timely intervention and improve clinical outcomes. As a first step, we developed an efficient and easy-to-install toolkit, the Time-based Elixhauser Comorbidity Index (TECI), which pre-calculates time-based Elixhauser comorbidities and can be extended to common data models (CDMs).
Methods
A Structured Query Language (SQL)-based toolkit, TECI, was built to pre-calculate time-specific Elixhauser comorbidity indices using data from a clinical data repository (CDR). Then it was extended to the Informatics for Integrating Biology and the Bedside (I2B2) and Observational Medical Outcomes Partnership (OMOP) CDMs.
Results
At the University of Arkansas for Medical Sciences (UAMS), the TECI toolkit was successfully installed to compute the indices from CDR data, and the scores were integrated into the I2B2 and OMOP CDMs. Comorbidity scores calculated by TECI were validated against: scores available in the 2015 quarter 1–3 Nationwide Readmissions Database (NRD) and scores calculated using the comorbidities using a previously validated algorithm on the 2015 quarter 4 NRD. Furthermore, TECI identified 18,846 UAMS patients that had changes in comorbidity scores over time (year 2013 to 2019). Comorbidities for a random sample of patients were independently reviewed, and in all cases, the results were found to be 100% accurate.
Conclusions
TECI facilitates the study of comorbidities within a time-dependent context, allowing better understanding of disease associations and trajectories, which has the potential to improve clinical outcomes.
Keyword
Figure
Reference
-
References
1. Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009; 7(4):357–63.
Article2. Epstein RH, Dexter F. Development and validation of a structured query language implementation of the Elixhauser comorbidity index. J Am Med Inform Assoc. 2017; 24(4):845–50.
Article3. Kattoor AJ, Pothineni NV, Goel A, Syed M, Syed S, Paydak H, et al. Prescription patterns and outcomes of patients with atrial fibrillation treated with direct oral anticoagulants and warfarin: a real-world analysis. J Cardiovasc Pharmacol Ther. 2019; 24:428–34.
Article4. Tinker A. How to improve patient outcomes for chronic diseases and comorbidities [Internet]. Salt Lake City (UT): HealthCatalyst;2017. [cited at 2020 Apr 15]. Available from: http://www.healthcatalyst.com/wp-content/uploads/2014/04/How-to-Improve-Patient-Outcomes.pdf.5. Zulman DM, Asch SM, Martins SB, Kerr EA, Hoffman BB, Goldstein MK. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014; 29(3):529–37.
Article6. Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002; 162(20):2269–76.
Article7. Fraccaro P, Kontopantelis E, Sperrin M, Peek N, Mallen C, Urban P, et al. Predicting mortality from changeover-time in the Charlson Comorbidity Index: a retrospective cohort study in a data-intensive UK health system. Medicine (Baltimore). 2016; 95(43):e4973.8. Giannoula A, Gutierrez-Sacristan A, Bravo A, Sanz F, Furlong LI. Identifying temporal patterns in patient disease trajectories using dynamic time warping: a population-based study. Sci Rep. 2018; 8(1):4216.
Article9. Jensen AB, Moseley PL, Oprea TI, Ellesoe SG, Eriksson R, Schmock H, et al. Temporal disease trajectories condensed from population-wide registry data covering 6.2 million patients. Nat Commun. 2014; 5:4022.
Article10. McPhail SM. Multimorbidity in chronic disease: impact on health care resources and costs. Risk Manag Healthc Policy. 2016; 9:143–56.
Article11. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36(1):8–27.
Article12. Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014; 472(9):2878–86.
Article13. Van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009; 47(6):626–33.
Article14. Healthcare Cost and Utilization Project. Creation of Elixhauser comorbidity variables (ICD-10-CM Elixhauser comorbidity software, version 2020. 1) [Internet]. Rockville (MD): Healthcare Cost and Utilization Project;2019. [cited at 2020 Apr 15]. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comoanaly_icd10cm_2020_1.txt.15. Healthcare Cost and Utilization Project. Nationwide HCUP databases [Internet]. Agency for Healthcare Research and Quality [Internet]. Rockville (MD): Healthcare Cost and Utilization Project;2019. [cited at 2020 Apr 15]. Available from: https://www.hcup-us.ahrq.gov/databases.jsp.16. Wang CY, Baldwin LM, Saver BG, Dobie SA, Green PK, Cai Y, et al. The contribution of longitudinal comorbidity measurements to survival analysis. Med Care. 2009; 47(7):813–21.
Article17. Zeng C, Ellis JL, Steiner JF, Shoup JA, McQuillan DB, Bayliss EA. Assessment of morbidity over time in predicting health outcomes. Med Care. 2014; Mar. 52:Suppl 3. S52–9.
Article18. Strauss VY, Jones PW, Kadam UT, Jordan KP. Distinct trajectories of multimorbidity in primary care were identified using latent class growth analysis. J Clin Epidemiol. 2014; 67(10):1163–71.
Article19. Garza M, Del Fiol G, Tenenbaum J, Walden A, Zozus MN. Evaluating common data models for use with a longitudinal community registry. J Biomed Inform. 2016; 64:333–41.
Article20. Klann JG, Phillips LC, Herrick C, Joss MA, Wagholikar KB, Murphy SN. Web services for data warehouses: OMOP and PCORnet on i2b2. J Am Med Inform Assoc. 2018; 25(10):1331–8.
Article21. Klann JG, Joss MAH, Embree K, Murphy SN. Data model harmonization for the All Of Us Research Program: transforming i2b2 data into the OMOP common data model. PLoS One. 2019; 14(2):e0212463.
Article22. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–9.
Article23. Klann JG, Abend A, Raghavan VA, Mandl KD, Murphy SN. Data interchange using i2b2. J Am Med Inform Assoc. 2016; 23(5):909–15.
Article24. Reich C, Ryan P, Belenkaya R, Natarajan K, Blacketer C. OMOP Common Data Model v6.0 Specifications [Internet]. [place unknown]: Github.com;2018. [cited at 2020 Apr 15]. Available from: https://github.com/OHDSI/CommonDataModel/wiki.25. Observational Health Data Sciences and Informatics. Athena standardized vocabularies [Internet]. Bethesda (MD): Observational Health Data Sciences and Informatics;2018. [cited at 2020 Apr 15]. Available from: http://athena.ohdsi.org/search-terms/terms?conceptClass=Staging+%2F+Scales&page=1&pageSize=15&query=comorbid.26. Makadia R, Ryan PB. Transforming the premier perspective hospital database into the Observational Medical Outcomes Partnership (OMOP) common data model. EGEMS (Wash DC). 2014; 2(1):1110.27. Healthcare Cost and Utilization Project. NRD file specifications-2013 [Internet]. Rockville (MD): Healthcare Cost and Utilization Project;2015. [cited at 2020 Apr 15]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nrd/nrdfilespecs.jsp.28. Healthcare Cost and Utilization Project. NRD file specifications-2015 [Internet]. Rockville (MD): Healthcare Cost and Utilization Project;2015. [cited at 2020 Apr 15]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nrd/nrdfilespecs.jsp.29. Duncan I, Ahmed T, Dove H, Maxwell TL. Medicare cost at end of life. Am J Hosp Palliat Care. 2019; 36(8):705–10.
Article30. Wright A, Feblowitz J, Maloney FL, Henkin S, Bates DW. Use of an electronic problem list by primary care providers and specialists. J Gen Intern Med. 2012; 27(8):968–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Social Media Mining Toolkit (SMMT)
- Comorbidity Adjustment in Health Insurance Claim Database
- A Comparative Study on Comorbidity Measurements with Lookback Period using Health Insurance Database: Focused on Patients Who Underwent Percutaneous Coronary Intervention
- Accelerating next generation sequencing data analysis: an evaluation of optimized best practices for Genome Analysis Toolkit algorithms
- Spinal Fractures in Ankylosing Spondylitis: Patterns, Management, and Complications in the United States – Analysis of Latest Nationwide Inpatient Sample Data