Healthc Inform Res.
2020 Jul;26(3):166-174. 10.4258/hir.2020.26.3.166.
Application of Predictive Modelling to Improve the Discharge Process in Hospitals
- Affiliations
-
- 1Healthcare Analytics, Baby Memorial Hospital, Kozhikode, India
- 2Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, India
- KMID: 2505257
- DOI: http://doi.org/10.4258/hir.2020.26.3.166
Abstract
Objectives
To find out the factors influencing discharge process turnaround time (TAT) and to accurately predict the discharge process TAT.
Methods
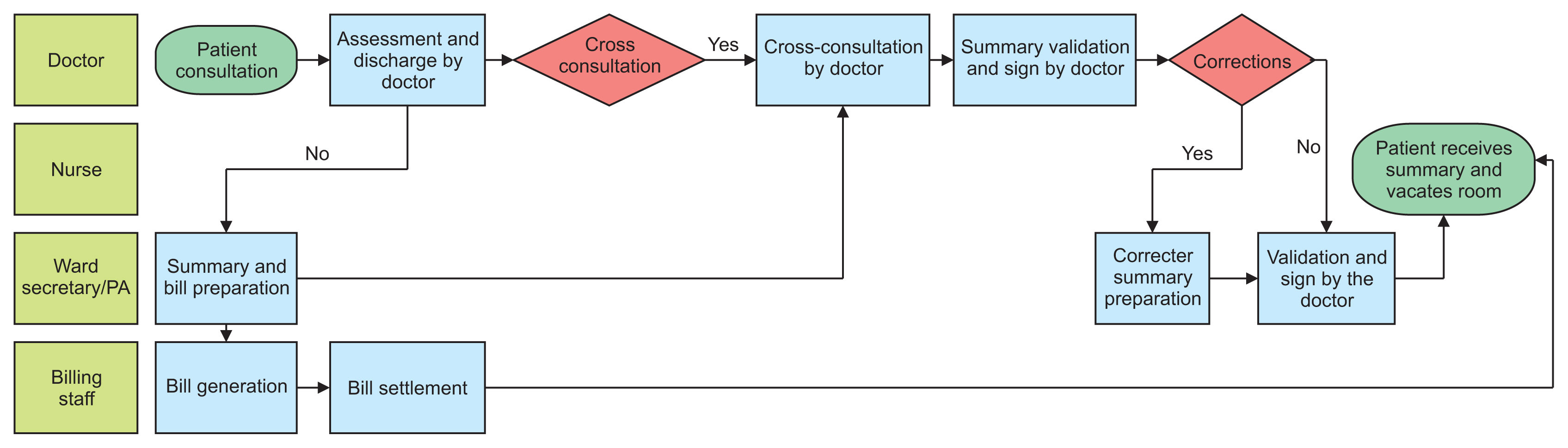
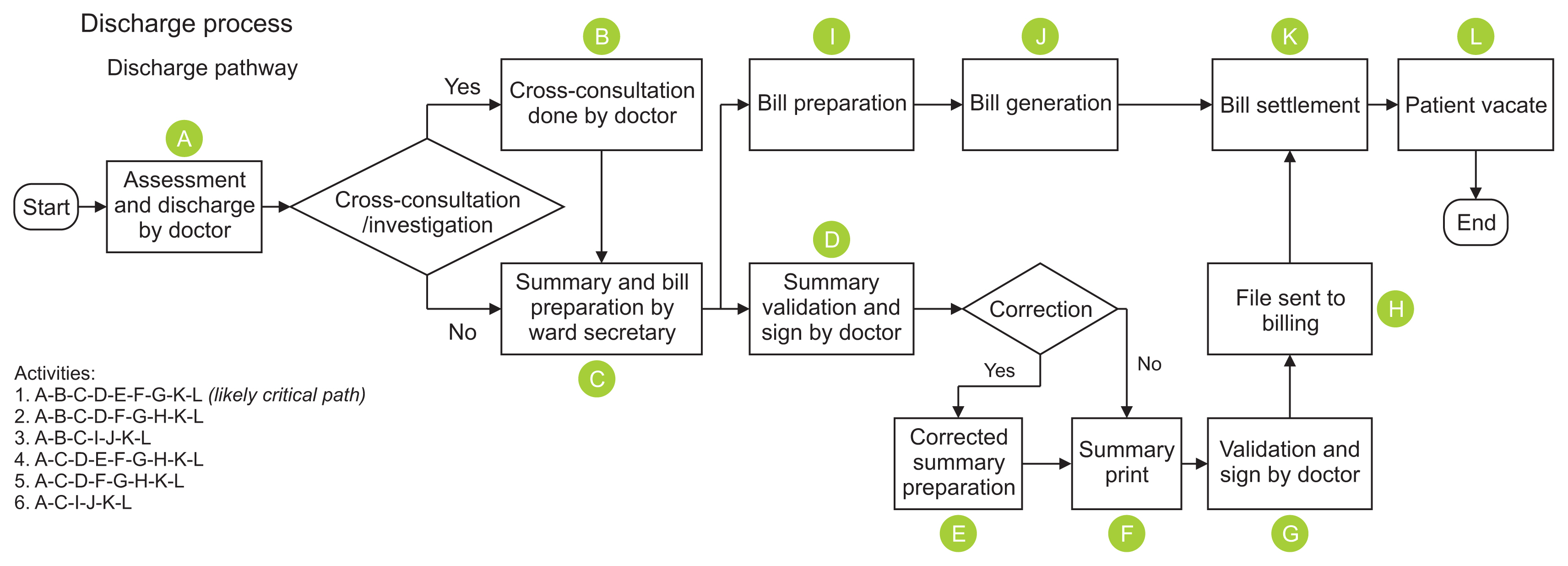
The discharge process of cardiology department inpatients in a tertiary care hospital was mapped over a month. The likely factors influencing discharge TAT were tested for significance by ANOVA. Multiple linear regression (MLR) was used to predict the TAT. The sample was divided into testing and training sets for regression. A model was generated using the training set and compared with the testing set for accuracy.
Results
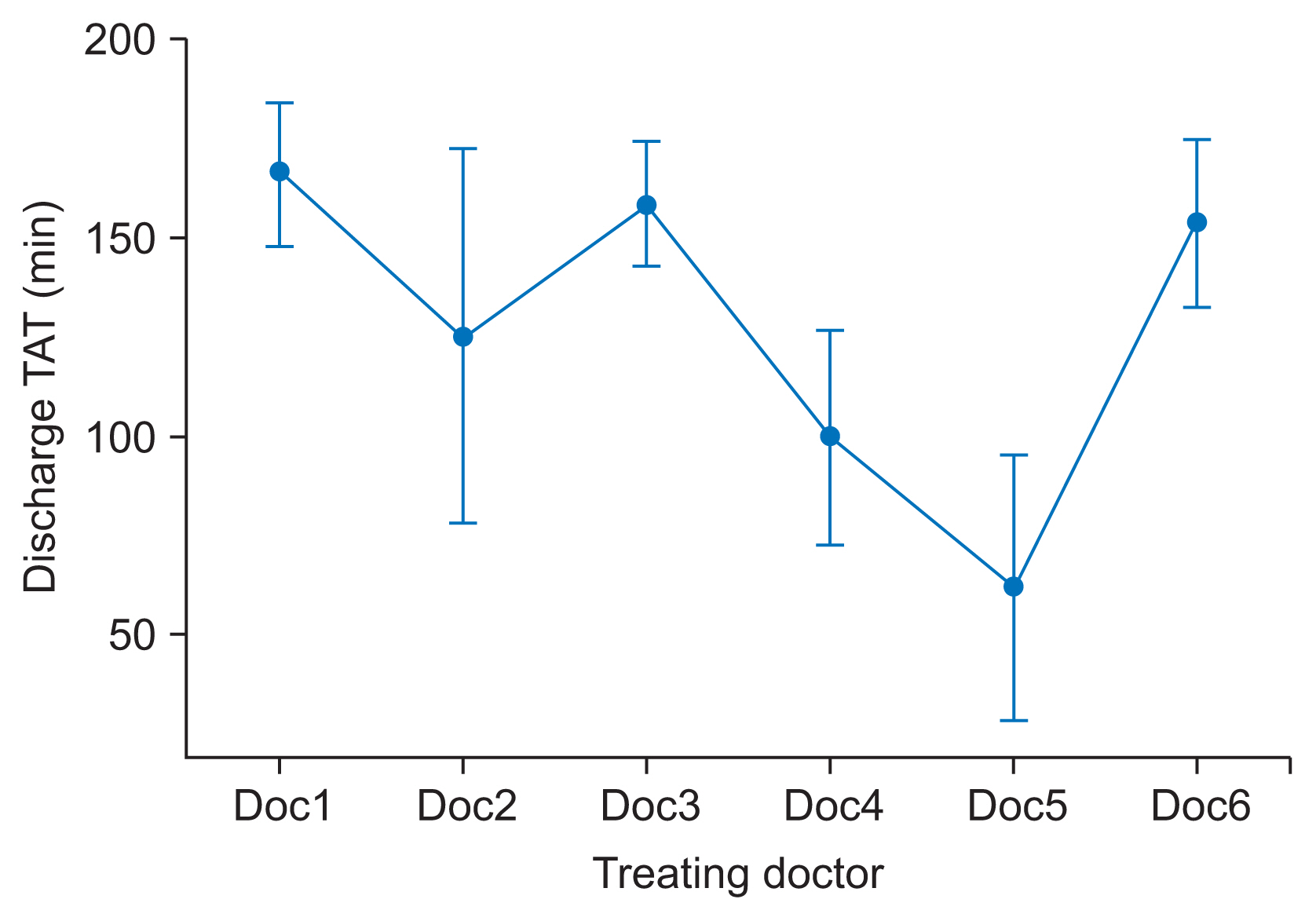
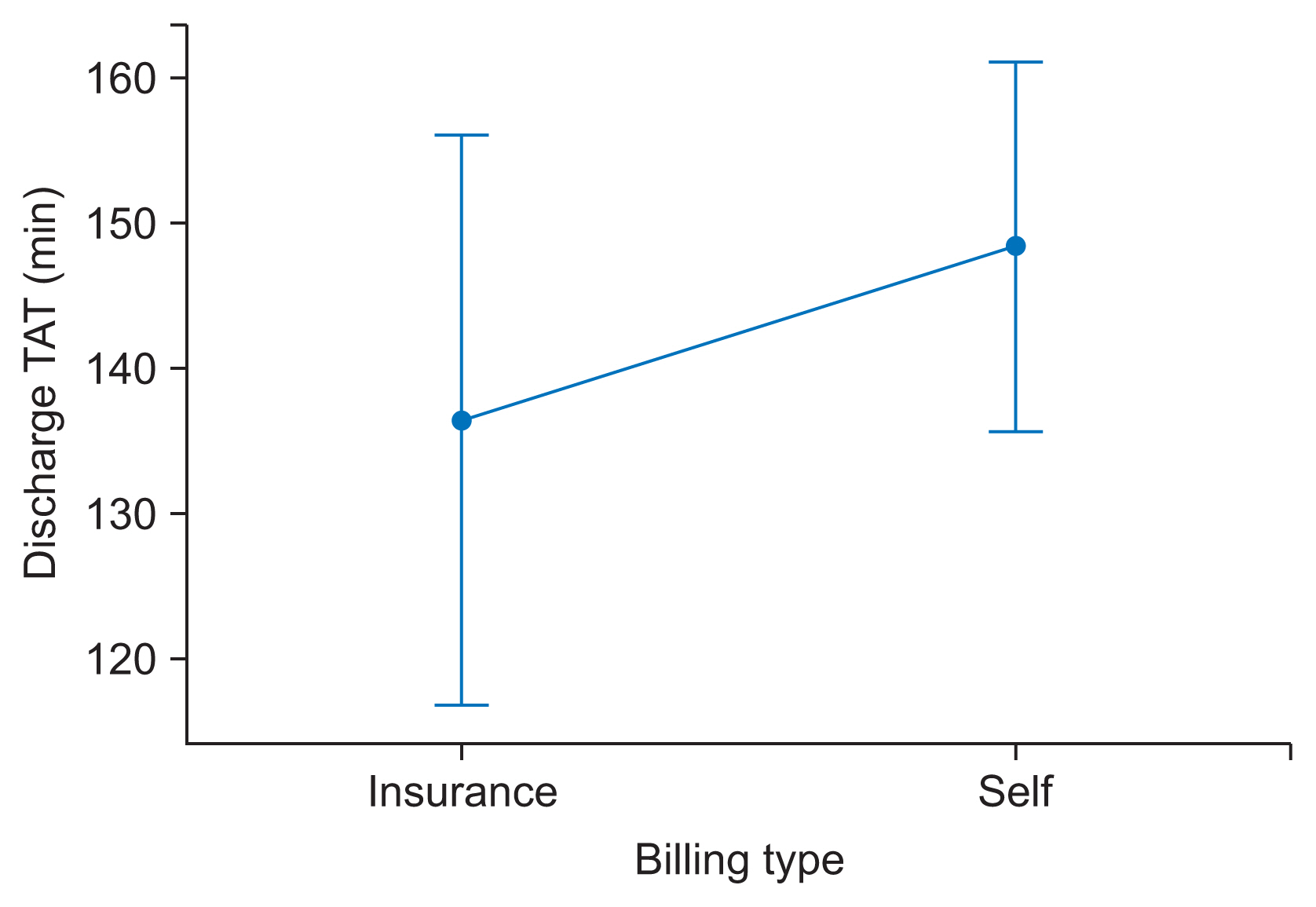
After a process map was plotted, the significant factors influencing the TAT were identified to be the treating doctor, and pending evaluations on the day of discharge. The MLR model was developed with Python libraries based on the two factors identified. The model predicted the discharge TAT with a 69% R2 value and 32.4 minutes (standard error) on the testing set and a 77.3% R2 value and 26.7 minutes (standard error) on the overall sample.
Conclusions
This study was an initiation to find out factors influencing discharge TAT and how those factors can be used to predict discharge in the hospital of interest. The study was validated and predicted the TAT with 77% accuracy after the significant factors that affect the discharge process were identified.
Figure
Reference
-
References
1. Kaur H, Kochar R. A study on discharge process of discharged patients of a multispecialty hospital Ludhiana. Int J Eng Manag Res. 2017; 7(3):688–94.2. Maloney CG, Wolfe D, Gesteland PH, Hales JW, Nkoy FL. A tool for improving patient discharge process and hospital communication practices: the "Patient Tracker". AMIA Annu Symp Proc. 2007; 2007:493–7.3. Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007; 2(5):314–23.
Article4. Falvo T, Grove L, Stachura R, Vega D, Stike R, Schlenker M, et al. The opportunity loss of boarding admitted patients in the emergency department. Acad Emerg Med. 2007; 14(4):332–7.
Article5. Shukla K, Upadhyay S. Predictive modelling for turn around time (TAT) of discharge process for insured patients in a corporate hospital of Pune city. J Health Manag. 2018; 20(1):56–63.
Article6. Dalal AK, Poon EG, Karson AS, Gandhi TK, Roy CL. Lessons learned from implementation of a computerized application for pending tests at hospital discharge. J Hosp Med. 2011; 6(1):16–21.
Article7. Hisham S. Statistical analysis of discharge data [Internet]. [place unknown]: github.com;2019. [cited at 2020 Jul 27]. Available from: https://github.com/hisham2k9/Share_files/blob/master/dischage%20model.ipynb.8. McKinney W. Python for data analysis: data wrangling with Pandas, NumPy, and IPython. Sebastopol (CA): O’Reilly Media;2012.9. Combes C, Kadri F, Chaabane S. Predicting hospital length of stay using regression models: Application to emergency department. In : Proceedings of the 10th International Conference on Modeling, Optimization & Simulation (MOSIM); 2014 Nov 5–7; Nancy, France.10. Sullivan B, Ming D, Boggan JC, Schulteis RD, Thomas S, Choi J, et al. An evaluation of physician predictions of discharge on a general medicine service. J Hosp Med. 2015; 10(12):808–10.
Article11. De Grood A, Blades K, Pendharkar SR. A review of discharge-prediction processes in acute care hospitals. Healthc Policy. 2016; 12(2):105–15.12. Pandis N. Multiple linear regression analysis. Am J Orthod Dentofacial Orthop. 2016; 149(4):581.
Article13. Thorpe KE. The use of regression analysis to determine hospital payment: the case of Medicare’s indirect teaching adjustment. Inquiry. 1988; 25(2):219–31.14. StatTrek. Residual analysis in regression [Internet]. [place unknown]: StatTrek;c2020. [cited at 2020 Jul 27]. Available from: https://stattrek.com/regression/residual-analysis.aspx#.15. Smith PF, Ganesh S, Liu P. A comparison of random forest regression and multiple linear regression for prediction in neuroscience. J Neurosci Methods. 2013; 220(1):85–91.
Article16. Edelman ER, van Kuijk SM, Hamaekers AE, de Korte MJ, van Merode GG, Buhre WF. Improving the prediction of total surgical procedure time using linear regression modeling. Front Med (Lausanne). 2017; 4:85.
Article17. Bouphan P, Srichan R. Factors affecting the research for solving health problem of health personnel at sub-district health promoting hospitals. Procedia Soc Behav Sci. 2017; 237:1097–104.
Article18. Freburger JK. Analysis of the relationship between the utilization of physical therapy services and outcomes for patients with acute stroke. Phys Ther. 1999; 79(10):906–18.19. Stephen O, Sain M, Maduh UJ, Jeong DU. An efficient deep learning approach to pneumonia classification in healthcare. J Healthc Eng. 2019; 2019:4180949.
Article20. Kaymak S, Almezhghwi K, Shelag AA. Classification of diseases on chest X-rays using deep learning. In : Aliev R, Kacprzyk J, Pedrycz W, Jamshidi M, Sadikoglu F, editors. 13th International Conference on Theory and Applications of Fuzzy Systems and Soft Computing; Cham, Switzerland: Springer;2018; p. 516–23.
Article21. Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019; 6(2):94–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validity of Principal Diagnoses in Discharge Summaries and ICD-10 Coding Assessments Based on National Health Data of Thailand
- A Multilevel Analysis about the Impact of Patient’s Willingness for Discharge on Successful Discharge from Long-term Care Hospitals
- R-based reproduction of the estimation process hidden behind NONMEM(R) Part 1: first-order approximation method
- Review of Core Elements used in Medical Records and their Definitions for Medical Informatics Standard
- Between-Hospital Variation in All-Cause Mortality for Potentially Avoidable Hospitalizations in Older People