Anesth Pain Med.
2020 Jul;15(3):349-355. 10.17085/apm.20006.
Effects of 10-min prewarming on core body temperature during gynecologic laparoscopic surgery under general anesthesia: a randomized controlled trial
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2504898
- DOI: http://doi.org/10.17085/apm.20006
Abstract
- Background
Previous research has shown a beneficial effect of prewarming for preventing inadvertent perioperative hypothermia. However, there are few studies of the effects of a short prewarming period, especially in gynecologic laparoscopic surgery.
Methods
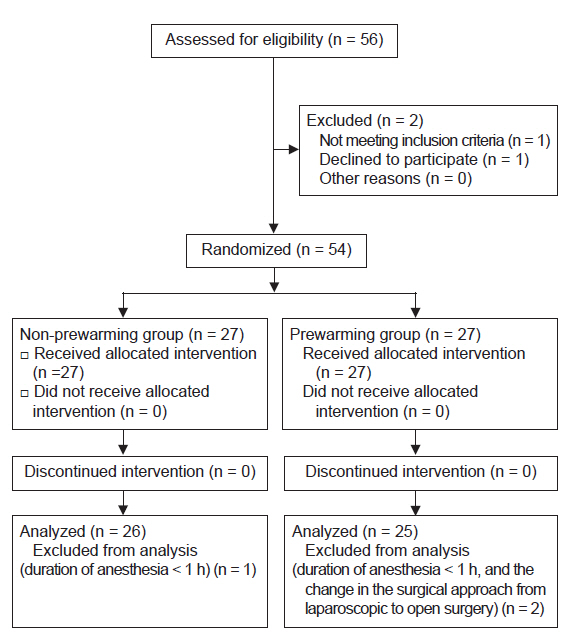
Fifty-four patients were randomly assigned to 2 groups. Patients in the non-prewarming group were only warmed intraoperatively with a forced air warming device, while those in the prewarming group were warmed for 10 min before anesthetic induction and during the surgery. The primary outcome was incidence of intraoperative hypothermia.
Results
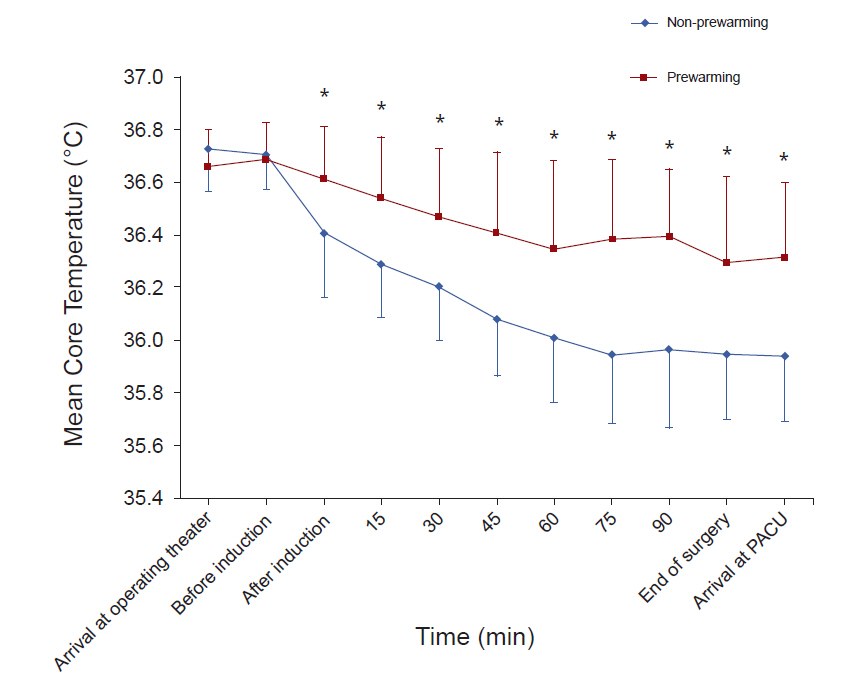
Intraoperative hypothermia was observed in 73.1% of the patients in the non-prewarming group and 24% of the patients in the prewarming group (P < 0.001). There were significant differences in core temperature changes between the groups (P < 0.001). Postoperative shivering occurred in 8 of the 26 (30.8%) patients in the non-prewarming group and in 1 of the 25 (4.0%) patients in the prewarming group (P = 0.024).
Conclusions
Forced air warming for 10 min before induction on the operating table combined with intraoperative warming was an effective method to prevent hypothermia in patients undergoing gynecologic laparoscopic surgery.
Keyword
Figure
Reference
-
1. National Institute for Health and Care Excellence. Hypothermia: prevention and management in adults having surgery. National Institute for Health and Care Excellence [serial on the Internet]. 2008 Apr [cited 2008 April 23]. Available from http://nice.org.uk/guidance/CG65.2. Frank SM, Fleisher LA, Breslow MJ, Higgins MS, Olson KF, Kelly S, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA. 1997; 277:1127–34.3. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of wound infection and temperature group. N Engl J Med. 1996; 334:1209–15.4. Schmied H, Kurz A, Sessler DI, Kozek S, Reiter A. Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty. Lancet. 1996; 347:289–92.5. Lenhardt R, Marker E, Goll V, Tschernich H, Kurz A, Sessler DI, et al. Mild intraoperative hypothermia prolongs postanesthetic recovery. Anesthesiology. 1997; 87:1318–23.6. Madrid E, Urrútia G, Roqué i Figuls M, Pardo-Hernandez H, Campos JM, Paniagua P, et al. Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults. Cochrane Database Syst Rev. 2016; 4:CD009016.7. Andrzejowski J, Hoyle J, Eapen G, Turnbull D. Effect of prewarming on post-induction core temperature and the incidence of inadvertent perioperative hypothermia in patients undergoing general anaesthesia. Br J Anaesth. 2008; 101:627–31.8. Lau A, Lowlaavar N, Cooke EM, West N, German A, Morse DJ, et al. Effect of preoperative warming on intraoperative hypothermia: a randomized-controlled trial. Can J Anaesth. 2018; 65:1029–40.9. Matsukawa T, Sessler DI, Sessler AM, Schroeder M, Ozaki M, Kurz A, et al. Heat flow and distribution during induction of general anesthesia. Anesthesiology. 1995; 82:662–73.10. Sessler DI, Schroeder M, Merrifield B, Matsukawa T, Cheng C. Optimal duration and temperature of prewarming. Anesthesiology. 1995; 82:674–81.11. Horn EP, Bein B, Böhm R, Steinfath M, Sahili N, Höcker J. The effect of short time periods of pre-operative warming in the prevention of peri-operative hypothermia. Anaesthesia. 2012; 67:612–7.12. Yoo JH, Ok SY, Kim SH, Park SY, Han YM, Kim D. The effect of 10 minutes of prewarming for prevention of inadvertent perioperative hypothermia: comparison with 30 minutes of prewarming. Anesth Pain Med. 2018; 13:447–53.13. Badjatia N, Strongilis E, Gordon E, Prescutti M, Fernandez L, Fernandez A, et al. Metabolic impact of shivering during therapeutic temperature modulation: the Bedside Shivering Assessment Scale. Stroke. 2008; 39:3242–7.14. Mäkinen MT. Comparison of body temperature changes during laparoscopic and open cholecystectomy. Acta Anaesthesiol Scand. 1997; 41:736–40.15. Nguyen NT, Fleming NW, Singh A, Lee SJ, Goldman CD, Wolfe BM. Evaluation of core temperature during laparoscopic and open gastric bypass. Obes Surg. 2001; 11:570–5.16. Farley DR, Greenlee SM, Larson DR, Harrington JR. Double-blind, prospective, randomized study of warmed, humidified carbon dioxide insufflation vs standard carbon dioxide for patients undergoing laparoscopic cholecystectomy. Arch Surg. 2004; 139:739–44.17. Bush HL Jr, Hydo LJ, Fischer E, Fantini GA, Silane MF, Barie PS. Hypothermia during elective abdominal aortic aneurysm repair: the high price of avoidable morbidity. J Vasc Surg. 1995; 21:392–402.18. Perl T, Peichl LH, Reyntjens K, Deblaere I, Zaballos JM, Bräuer A. Efficacy of a novel prewarming system in the prevention of perioperative hypothermia. A prospective, randomized, multicenter study. Minerva Anestesiol. 2014; 80:436–43.19. Sun Z, Honar H, Sessler DI, Dalton JE, Yang D, Panjasawatwong K, et al. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. Anesthesiology. 2015; 122:276–85.20. Jo YY, Chang YJ, Kim YB, Lee S, Kwak HJ. Effect of preoperative forced-air warming on hypothermia in elderly patients undergoing transurethral resection of the prostate. Urol J. 2015; 12:2366–70.21. Jun JH, Chung MH, Kim EM, Jun IJ, Kim JH, Hyeon JS, et al. Effect of pre-warming on perioperative hypothermia during holmium laser enucleation of the prostate under spinal anesthesia: a prospective randomized controlled trial. BMC Anesthesiol. 2018; 18:201.22. Stavem K, Saxholm H, Smith-Erichsen N. Accuracy of infrared ear thermometry in adult patients. Intensive Care Med. 1997; 23:100–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of short-term prewarming on body temperature in arthroscopic shoulder surgery
- Effects of Heated-Humidified Anesthetic Gas in the Elderly Patients with Colorectal Cancer during Laparoscopic Surgery: Randomized Controlled Trial
- The Effects of Insufflation with Heated CO2 upon Body Temperature and Arterial Blood Gas Analysis during Gynecologic Laparoscopic Surgery
- The effect of warmed inspired gases on body temperature during arthroscopic shoulder surgery under general anesthesia
- Comparison of the effects of sevoflurane and propofol on core body temperature during laparoscopic abdominal surgery