J Korean Med Sci.
2020 Jul;35(29):e233. 10.3346/jkms.2020.35.e233.
Changes in Characteristics of Patients with Liver Cirrhosis Visiting a Tertiary Hospital over 15 Years: a Retrospective Multi-Center Study in Korea
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 3Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 4Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea
- 5Department of Internal Medicine, Dongguk University College of Medicine, Gyeongju, Korea
- KMID: 2504698
- DOI: http://doi.org/10.3346/jkms.2020.35.e233
Abstract
- Background
Liver cirrhosis has become a heavy burden not only for patients, but also for our society. However, little is known about the recent changes in clinical outcomes and characteristics of patients with cirrhosis-related complications in Korea. Therefore, we aimed to evaluate changes in characteristics of patients with liver cirrhosis in Daegu-Gyeongbuk province in Korea over the past 15 years.
Methods
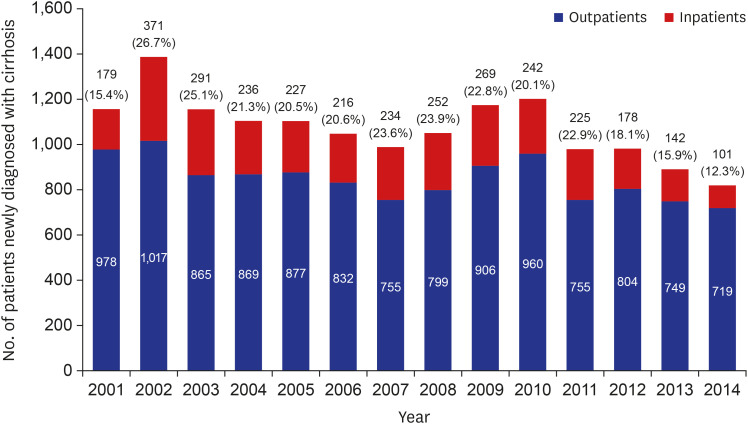
We retrospectively reviewed the medical records of 15,716 liver cirrhotic patients from 5 university hospitals in Daegu-Gyeongbuk province from 2000 to 2014. The Korean Standard Classification of Diseases-6 code associated with cirrhosis was investigated through medical records and classified according to the year of first visit.
Results
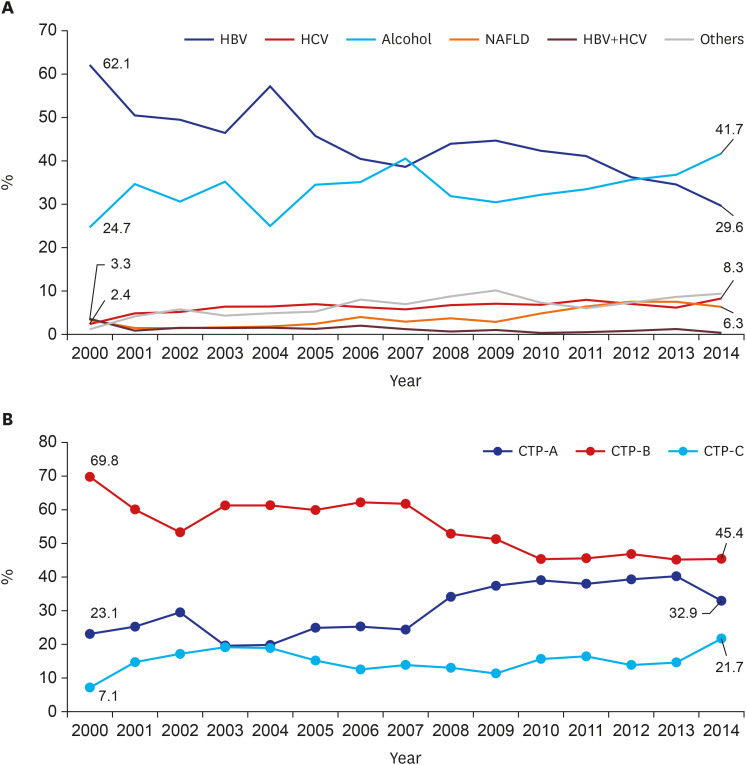
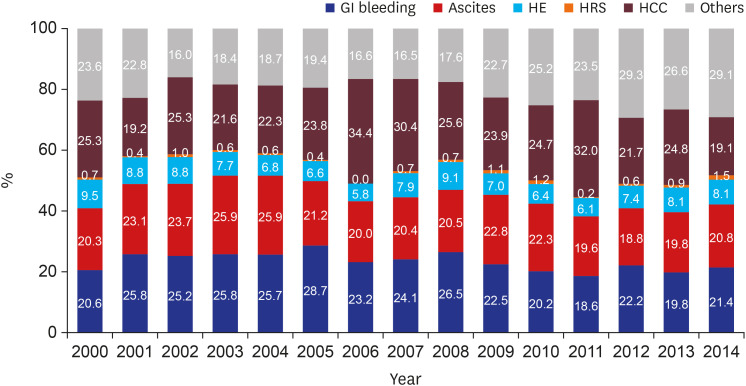
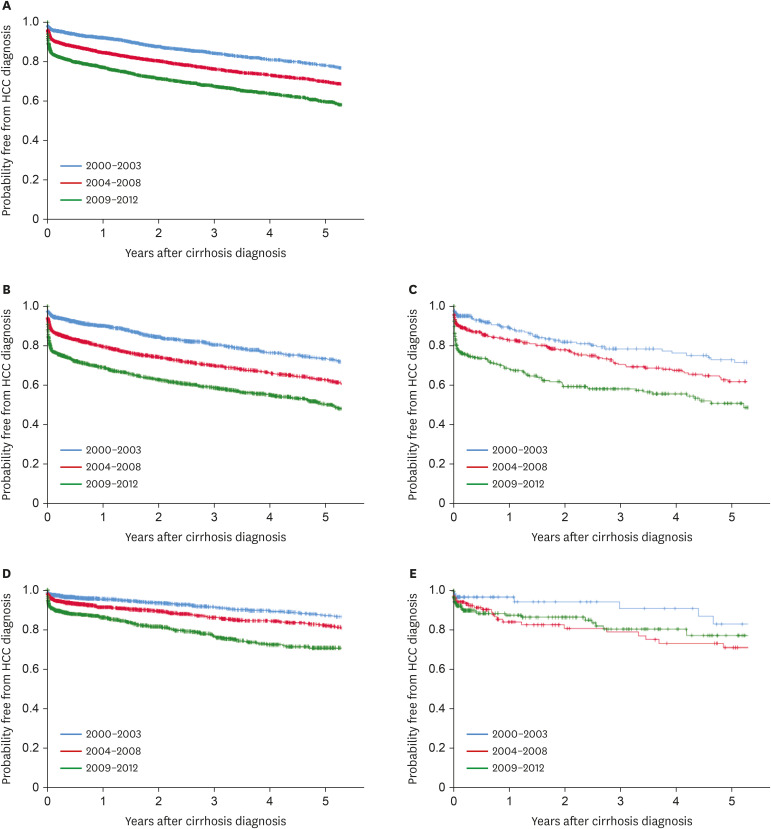
A total of 15,716 patients was diagnosed with cirrhosis. A number of patients newly diagnosed with cirrhosis has decreased each year. In 2000, patients were most likely to be diagnosed with hepatitis B virus (HBV) cirrhosis, followed by alcoholic cirrhosis. There was a significant decrease in HBV (P < 0.001), but alcohol, hepatitis C virus (HCV), and non-alcoholic fatty liver disease (NAFLD) showed a significant increase during the study period (alcohol, P = 0.036; HCV, P = 0.001; NAFLD, P = 0.001). At the time of initial diagnosis, the ratio of Child-Turcotte-Pugh (CTP) class A gradually increased from 23.1% to 32.9% (P < 0.001). The most common cause of liver-related hospitalization in 2000 was hepatocellular carcinoma (HCC) (25.5%); in 2014, gastrointestinal bleeding with esophageal and gastric varices (21.4%) was the most common cause. Cases of hospitalization with liver-related complication represented 76.4% of all cases in 2000 but 70.9% in 2014. Incidence rate of HCC has recently increased. In addition, HCC-free survival was significantly lower in CTP class A than in classes B and C. Finally, there was significant difference in HCC occurrence according to causes (P < 0.001). HBV and HCV cirrhosis had lower HCC-free survival than alcoholic and NAFLD cirrhosis.
Conclusion
In recent years, the overall number of cirrhosis patients has decreased. This study confirmed the recent trend in decrease of cirrhosis, especially of cirrhosis due to HBV, and the increase of HCV, alcoholic and NAFLD cirrhosis. Targeted screening for at-risk patients will facilitate early detection of liver diseases allowing effective intervention and may have decreased the development of cirrhosis and its complications.
Figure
Reference
-
1. Statistics Korea. Updated 2018. Accessed December 2018. http://www.kostat.go.kr/portal/korea/kor_nw/5/3/index.action.2. Statistic Korea. Updated 2018. Accessed July 2019. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E07&conn_path=I2.3. Wong MC, Huang J. The growing burden of liver cirrhosis: implications for preventive measures. Hepatol Int. 2018; 12(3):201–203. PMID: 29679258.
Article4. Yim SY, Kim JH. The epidemiology of hepatitis B virus infection in Korea. Korean J Intern Med. 2019; 34(5):945–953. PMID: 30919608.
Article5. Kim BK, Jang ES, Kim JH, Park SY, Ahn SV, Kim HJ, et al. Current status of and strategies for hepatitis C control in South Korea. Clin Mol Hepatol. 2017; 23(3):212–218. PMID: 28942625.
Article6. Jeong SH, Jang ES, Choi HY, Kim KA, Chung W, Ki M. Current status of hepatitis C virus infection and countermeasures in South Korea. Epidemiol Health. 2017; 39:e2017017. PMID: 28774165.
Article7. Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, et al. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. 2010; 29(4):437–445. PMID: 20636661.
Article8. Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014; 12(1):145. PMID: 25242656.
Article9. Hsiang JC, Bai WW, Raos Z, Stableforth W, Upton A, Selvaratnam S, et al. Epidemiology, disease burden and outcomes of cirrhosis in a large secondary care hospital in South Auckland, New Zealand. Intern Med J. 2015; 45(2):160–169. PMID: 25371019.
Article10. Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol. 2015; 49(8):690–696. PMID: 25291348.11. Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines: management of alcoholic liver disease. Clin Mol Hepatol. 2013; 19(3):216–254. PMID: 24133661.12. Statistics Korea. Updated 2015. Accessed August 2019. http://kosis.kr/statHtml/statHtml.do?orgId=358&tblId=DT_358N_H402101&conn_path=I2.13. Cho EJ, Kim SE, Suk KT, An J, Jeong SW, Chung WJ, et al. Current status and strategies for hepatitis B control in Korea. Clin Mol Hepatol. 2017; 23(3):205–211. PMID: 28942624.
Article14. WHO statistical information system. Updated 2018. Accessed August 2019. http://www.who.int/substance_abuse/publications/global_alcohol_report/en/.15. Chung WJ, Chun HJ, Lee SM. Socioeconomic costs of alcohol drinking in Korea. J Prev Med Public Health. 2006; 39(1):21–29. PMID: 16613068.16. Lee JK, Kim YI, Yoon SJ, Lee JY, Lee H, Park JH, et al. Estimating the burden of diseases due to high alcohol consumption in Korea. J Prev Med Public Health. 2005; 38(2):175–181. PMID: 16315755.17. Kim DY, Kim IH, Jeong SH, Cho YK, Lee JH, Jin YJ, et al. A nationwide seroepidemiology of hepatitis C virus infection in South Korea. Liver Int. 2013; 33(4):586–594. PMID: 23356674.
Article18. Shin HR, Hwang SY, Nam CM. The prevalence of hepatitis C virus infection in Korea: pooled analysis. J Korean Med Sci. 2005; 20(6):985–988. PMID: 16361809.
Article19. Moon KM, Baik SK. Usefulness of ultrasonographic scoring system in diagnosis of alcoholic cirrhosis. Clin Ultrasound. 2016; 1(2):92–100.
Article20. Kim BK, Kim SU, Park JY, Kim DY, Ahn SH, Park MS, et al. Applicability of BCLC stage for prognostic stratification in comparison with other staging systems: single centre experience from long-term clinical outcomes of 1717 treatment-naïve patients with hepatocellular carcinoma. Liver Int. 2012; 32(7):1120–1127. PMID: 22524688.
Article21. Kim BH, Lim YS, Kim EY, Kong HJ, Won YJ, Han S, et al. Temporal improvement in survival of patients with hepatocellular carcinoma in a hepatitis B virus-endemic population. J Gastroenterol Hepatol. 2018; 33(2):475–483. PMID: 28612951.
Article22. Kwak HW, Park JW, Nam BH, Yu A, Woo SM, Kim TH, et al. Clinical outcomes of a cohort series of patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol. 2014; 29(4):820–829. PMID: 24325272.
Article23. Sung JJ, Tsoi KK, Wong VW, Li KC, Chan HL. Meta-analysis: Treatment of hepatitis B infection reduces risk of hepatocellular carcinoma. Aliment Pharmacol Ther. 2008; 28(9):1067–1077. PMID: 18657133.
Article24. Choi J, Han S, Kim N, Lim YS. Increasing burden of liver cancer despite extensive use of antiviral agents in a hepatitis B virus-endemic population. Hepatology. 2017; 66(5):1454–1463. PMID: 28628942.
Article25. Cougot D, Neuveut C, Buendia MA. HBV induced carcinogenesis. J Clin Virol. 2005; 34 Suppl 1:S75–8.
Article26. Fung J, Lai CL, Yuen MF. Hepatitis B and C virus-related carcinogenesis. Clin Microbiol Infect. 2009; 15(11):964–970. PMID: 19874379.
Article