J Korean Neurosurg Soc.
2020 Jul;63(4):519-531. 10.3340/jkns.2020.0026.
Current Status of Neurosurgical and Neurointensive Care Units in Korea : A Brief Report on Nationwide Survey Results
- Affiliations
-
- 1Department of Neurosurgery, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurosurgery, Eunpyeong St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Neurosurgery, Inha Hospital, Inha University School of Medicine, Incheon, Korea
- 4Department of Neurosurgery, Hanyang University Guri Hospital, Guri, Korea
- 5Department of Neurosurgery, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea
- 6Department of Neurosurgery, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 7Department of Neurosurgery, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 8Department of Anesthology and Pain Medicine, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 9Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea
- 10Department of Neurosurgery, Korea Universuty Guro Hospital, Seoul, Korea
- KMID: 2504647
- DOI: http://doi.org/10.3340/jkns.2020.0026
Abstract
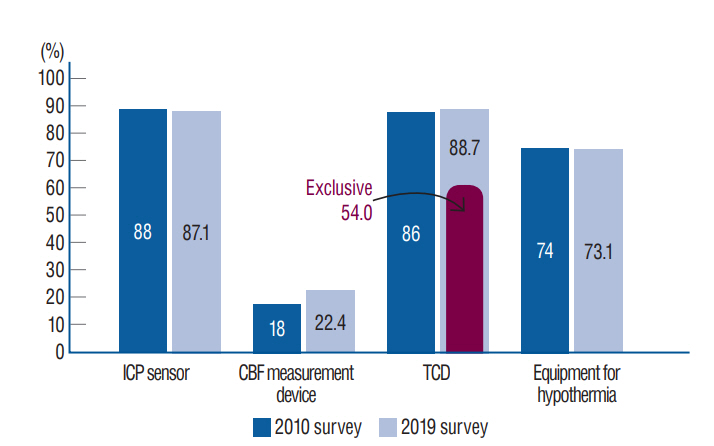
Objective
: The purpose of this study is identify the operation status of the neurosurgical care units (NCUs) in neurosurgical residency training hospitals nationwide and determine needed changes by comparing findings with those obtained from the Korean Neurosurgical Society (KNS) and Korean Society of Neurointensive Care Medicine (KNIC) survey of 2010. Method : This survey was conducted over 1 year in 86 neurosurgical residency training hospitals and two neurosurgery specialist hospitals and focused on the following areas : 1) the current status of the infrastructure and operating systems of NCUs in Korea, 2) barriers to installing neurointensivist team systems, 3) future roles of the KNS and KNIC, and 4) a handbook for physicians and practitioners in NCUs. We compared and analyzed the results of this survey with those from a KNIC survey of 2010.
Results
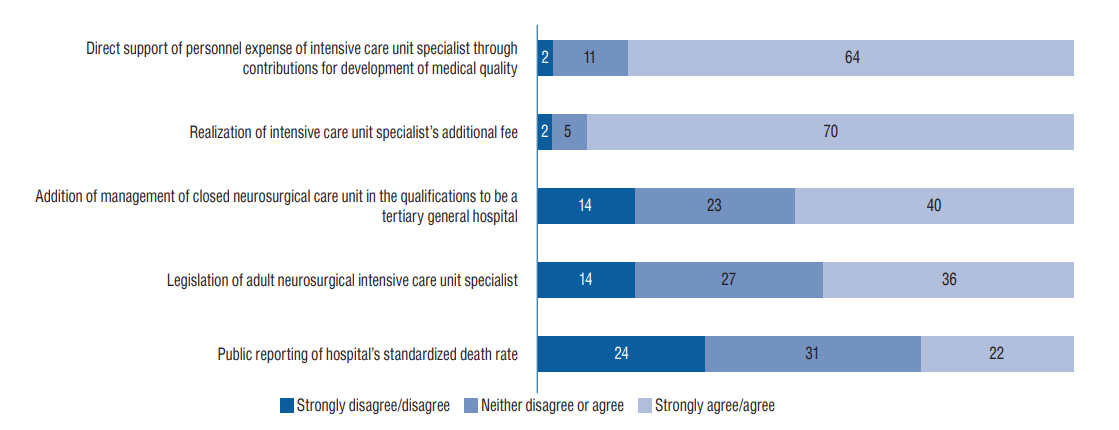
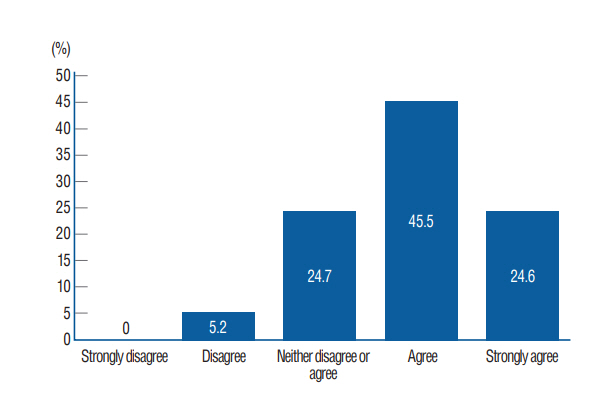
: Seventy seven hospitals (87.5%) participated in the survey. Nineteen hospitals (24.7%) employed a neurointensivist or faculty member; Thirty seven hospitals (48.1%) reported high demand for neurointensivists, and 62 hospitals (80.5%) stated that the mandatory deployment of a neurointensivist improved the quality of patient care. Forty four hospitals (57.1%) believed that hiring neurointensivist would increase hospital costs, and in response to a question on potential earnings declines. In terms of potential solutions to these problems, 70 respondents (90.9%) maintained that additional fees were necessary for neurointensivists’ work, and 64 (83.1%) answered that direct support was needed of the personnel expenses for neurointensivists.
Conclusion
: We hope the results of this survey will guide successful implementation of neurointensivist systems across Korea.
Figure
Cited by 1 articles
-
Trend of Intensive Care Unit Admission in Neurology-Neurosurgery Adult Patients in South Korea : A Nationwide Population-Based Cohort Study
Saeyeon Kim, Tak Kyu Oh, In-Ae Song, Young-Tae Jeon
J Korean Neurosurg Soc. 2024;67(1):84-93. doi: 10.3340/jkns.2023.0082.
Reference
-
References
1. Korbakis G, Vespa PM. Multimodal neurologic monitoring. Handb Clin Neurol. 140:91–105. 2017.
Article2. Markandaya M, Thomas KP, Jahromi B, Koenig M, Lockwood AH, Nyquist PA, et al. The role of neurocritical care: a brief report on the survey results of neurosciences and critical care specialists. Neurocrit Care. 16:72–81. 2012.
Article3. Misseri G, Cortegiani A, Gregoretti C. How to communicate between surgeon and intensivist? Curr Opin Anaesthesiol. 33:170–176. 2020.
Article4. Park BJ. Current Status of Neurointensive Care Unit in Korea. The 1st Annual Meeting of Korean Neurointensivecare Society; 2010 Apr 4; Seoul, Korea.5. Rivera Lara L, Püttgen HA. Multimodality monitoring in the neurocritical care unit. Continuum (Minneap Minn). 24:1776–1788. 2018.
Article6. Rodricks MB, Hawkins SE, Anderson GA, Basignani C, Tuppeny M. Mandatory intensivist management decreases length of stay, facilitates an increase in admissions and minimizes closure of a neurocritical care unit. Neurocrit Care. 23:307–312. 2015.
Article7. Ryu JA, Yang JH, Chung CR, Suh GY, Hong SC. Impact of neurointensivist co-management on the clinical outcomes of patients admitted to a neurosurgical intensive care unit. J Korean Med Sci. 32:1024–1030. 2017.
Article8. Sheth KN, Drogan O, Manno E, Geocadin RG, Ziai W. Neurocritical care education during neurology residency: AAN survey of US program directors. Neurology. 78:1793–1796. 2012.
Article9. Song HK, Lee BI, Lee JH, Lee KS, Whang SH. Status of neurocritical care in Korea: a nationwide questionnaire survey. J Neurocrit Care. 6:82–86. 2013.10. Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 32:2311–2317. 2004.
Article11. Varelas PN, Conti MM, Spanaki MV, Potts E, Bradford D, Sunstrom C, et al. The impact of a neurointensivist-led team on a semiclosed neurosciences intensive care unit. Crit Care Med. 32:2191–2198. 2004.
Article12. Varelas PN, Eastwood D, Yun HJ, Spanaki MV, Hacein Bey L, Kessaris C, et al. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg. 104:713–719. 2006.
Article13. Varelas PN, Schultz L, Conti M, Spanaki M, Genarrelli T, Hacein-Bey L. The impact of a neuro-intensivist on patients with stroke admitted to a neurosciences intensive care unit. Neurocrit Care. 9:293–299. 2008.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proposal for the Promotion of Korean Neurosurgery
- Current Status of Intensive Care Units Registered as Critical Care Subspecialty Training Hospitals in Korea
- The Current Status and the Perspectives of Nutrition Survey
- A Study on the Neurosurgical Intensive Care Unit
- A Survey of Patients Who Were Admitted for Life-Sustaining Therapy in Nationwide Medical Institutions