J Korean Neurosurg Soc.
2020 Jul;63(4):495-503. 10.3340/jkns.2019.0169.
Thyroid-Stimulating Hormone-Secreting Pituitary Adenomas : Single Institutional Experience of 14 Consecutive Cases
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2504644
- DOI: http://doi.org/10.3340/jkns.2019.0169
Abstract
Objective
: Thyroid-stimulating hormone (TSH)-secreting pituitary adenoma (PA) is an extremely rare functioning form of PA that accounts for 0.7–2% of all such cases. The previously reported outcomes of the surgical removal of TSH-PA are poor. Owing to its extremely low incidence, most available reports on TSH-PA are case reports or small case series. Thus, we investigated the clinical and endocrinological outcomes of surgically treated TSH-PA through our institutional series.
Methods
: We retrospectively reviewed 14 consecutive cases of surgically treated TSH-PA, focusing on the clinical, radiological, surgical, and endocrinological data.
Results
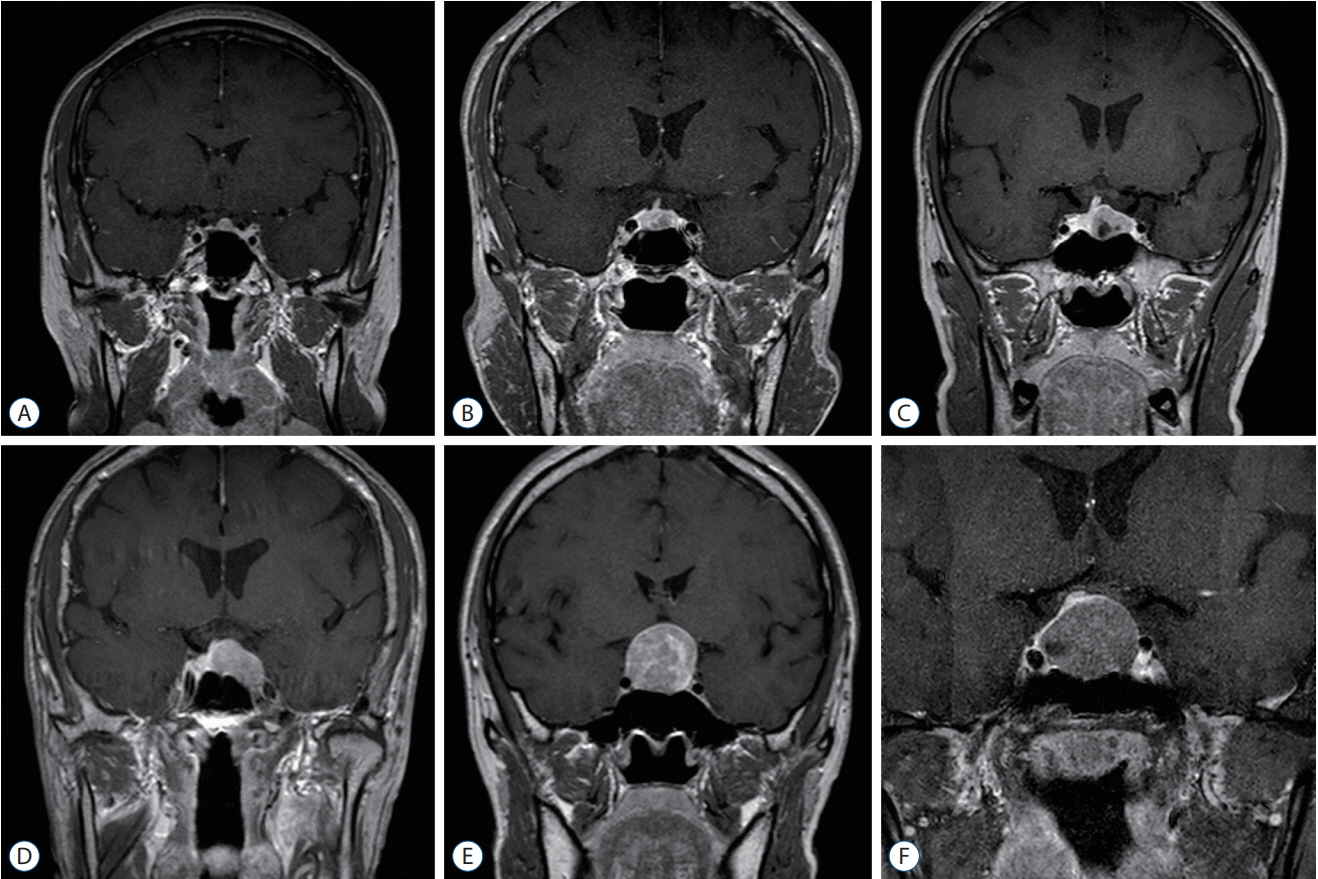
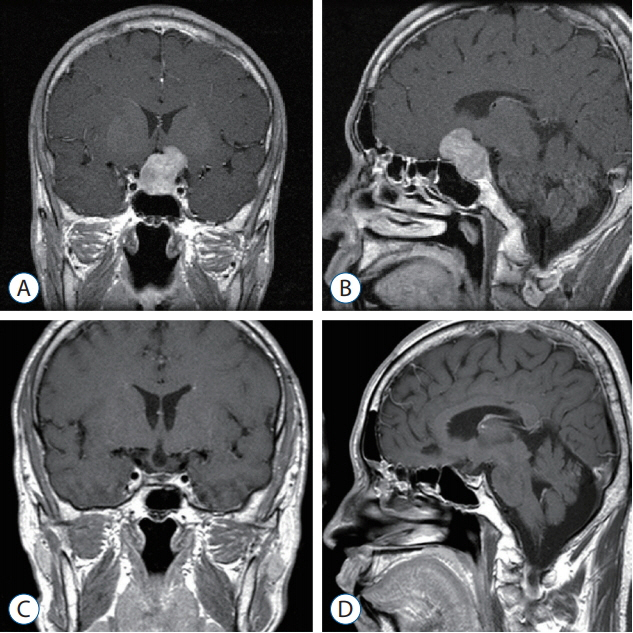
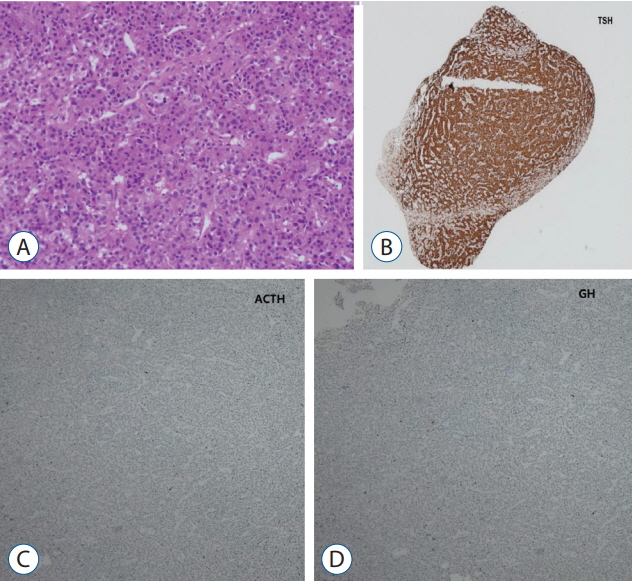
: There were seven male (50%) and seven female (50%) patients. The mean age was 42.5 years (range, 19–63). The mean tumor size was 16.6 mm (range, 4–30). Optic chiasm compression was noted in six patients (42.9%), and no patient showed cavernous sinus invasion. Thirteen of 14 patients (92.8%) underwent transnasal transsphenoidal approach (TSA), and one patient underwent TSA followed by transcranial approach for residual tumor removal. Thirteen of 14 patients (92.8%) showed endocrinological remission; all patients who experienced remission showed subnormal levels of TSH (<0.4 μU/mL) on postoperative day 2. Recurrence occurred in two patients (14.2%). One patient underwent subsequent revision transnasal TSA for recurrent tumor removal, and the other patient underwent gamma knife radiosurgery for recurrence.
Conclusion
: Surgical treatment showed excellent surgical outcomes. The TSH level in the immediate postoperative period may be a predictor for endocrinological remission.
Figure
Reference
-
References
1. Beck-Peccoz P, Lania A, Beckers A, Chatterjee K, Wemeau JL. 2013 European thyroid association guidelines for the diagnosis and treatment of thyrotropin-secreting pituitary tumors. Eur Thyroid J. 2:76–82. 2013.
Article2. Beck-Peccoz P, Persani L. Medical management of thyrotropin-secreting pituitary adenomas. Pituitary. 5:83–88. 2002.3. Brucker-Davis F, Oldfield EH, Skarulis MC, Doppman JL, Weintraub BD. Thyrotropin-secreting pituitary tumors: diagnostic criteria, thyroid hormone sensitivity, and treatment outcome in 25 patients followed at the National Institutes of Health. J Clin Endocrinol Metab. 84:476–486. 1999.
Article4. Ezzat S, Horvath E, Kovacs K, Smyth HS, Singer W, Asa SL. Basic fibroblast growth factor expression by two prolactin and thyrotropinproducing pituitary adenomas. Endocr Pathol. 6:125–134. 1995.
Article5. Hughes JD, Young WF, Chang AY, Link MJ, Garces YI, Laack NN, et al. Radiosurgical management of patients with persistent or recurrent cushing disease after prior transsphenoidal surgery: a management algorithm based on a 25-year experience. Neurosurgery. 86:557–564. 2020.
Article6. Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery. 33:610–617. discussion 617-618. 1993.
Article7. Macchia E, Gasperi M, Lombardi M, Morselli L, Pinchera A, Acerbi G, et al. Clinical aspects and therapeutic outcome in thyrotropin-secreting pituitary adenomas: a single center experience. J Endocrinol Invest. 32:773–779. 2009.
Article8. Micko AS, Wöhrer A, Wolfsberger S, Knosp E. Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg. 122:803–811. 2015.
Article9. Minniti G, Osti MF, Niyazi M. Target delineation and optimal radiosurgical dose for pituitary tumors. Radiat Oncol. 11:135. 2016.
Article10. Minnitia G, Clarkea E, Scaringia C, Enrici RM. Stereotactic radiotherapy and radiosurgery for non-functioning and secreting pituitary adenomas. Rep Pract Oncol Radiother. 21:370–378. 2016.
Article11. Mouslech Z, Somali M, Sakali AK, Savopoulos C, Mastorakos G, Hatzitolios AI. TSH-secreting pituitary adenomas treated by gamma knife radiosurgery: our case experience and a review of the literature. Hormones (Athens). 15:122–128. 2016.
Article12. Mouslech Z, Somali M, Sakali AK, Savopoulos C, Mastorakos G, Hatzitolios AI. TSH-secreting pituitary adenomas treated by gamma knife radiosurgery: our case experience and a review of the literature. Hormones. 15:122–128. 2016.
Article13. Ónnestam L, Berinder K, Burman P, Dahlqvist P, EdenEngström B, Wahlberg J, et al. National incidence and prevalence of TSH-secreting pituitary adenomas in Sweden. J Clin Endocrinol Metab. 98:626–635. 2013.
Article14. Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol 17 Suppl 4. iv1–iv62. 2015.
Article15. Palace MR. Perioperative management of thyroid dysfunction. Health Serv Insights. 10:1178632916689677. 2017.
Article16. Rotermund R, Riedel N, Burkhardt T, Matschke J, Schmidt N-O, Aberle J, et al. Surgical treatment and outcome of TSH-producing pituitary adenomas. Acta Neurochir (Wien). 159:1219–1226. 2017.
Article17. Sanno N, Teramoto A, Osamura RY. Long-term surgical outcome in 16 patients with thyrotropin pituitary adenoma. J Neurosurg. 93:194–200. 2000.
Article18. Tjornstrand A, Gunnarsson K, Evert M, Holmberg E, Ragnarsson O, Rosén T, et al. The incidence rate of pituitary adenomas in western Sweden for the period 2001-2011. Eur J Endocrinol. 171:519–526. 2014.
Article19. Tjörnstrand A, Nyström HF. Diagnostic approach to TSH-producing pituitary adenoma. Eur J Endocrinol. 177:R183–R197. 2017.20. Yamada S, Fukuhara N, Horiguchi K, Yamaguchi-Okada M, Nishioka H, Takeshita A, et al. Clinicopathological characteristics and therapeutic outcomes in thyrotropin-secreting pituitary adenomas: a single-center study of 90 cases. J Neurosurg. 121:1462–1473. 2014.
Article21. Zhao W, Ye H, Li Y, Zhou L, Lu B, Zhang S, et al. Thyrotropin-secreting pituitary adenomas: diagnosis and management of patients from one Chinese center. Wien Klin Wochenschr. 124:678–684. 2012.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical Transsphenoidal Approach for Pituitary Denomas
- Comparative evaluation of CT and secreting hormones in pituitary adenomas
- MRI of the TSH(Thyroid Stimulating Hormone) -Secreting Pituitary Adenoma
- Clinical Characteristics and Treatments of Patients with TSH Secreting Pituitary Adenoma
- Pituitary Adenomas in Childhood and Adolescence