Korean J Gastroenterol.
2020 Jul;76(1):28-36. 10.4166/kjg.2020.76.1.28.
Current Status of Amebic Liver Abscess in Korea Comparing with Pyogenic Liver Abscess
- Affiliations
-
- 1Division of Gastroenterology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2504567
- DOI: http://doi.org/10.4166/kjg.2020.76.1.28
Abstract
- Background/Aims
With the improvement of hygiene, the incidence of amebic liver abscess is decreasing in South Korea. On the other hand, there is little data on the status of amebic liver abscess compared to pyogenic liver abscess.
Methods
Patients with an amebic liver abscess, in whom Entamoeba histolytica (E. histolytica) IgG was positive, were identified retrospectively in a university hospital. The clinical, laboratory, and radiological characteristics of amebic liver abscess were compared with those of pyogenic liver abscess in the same period.
Results
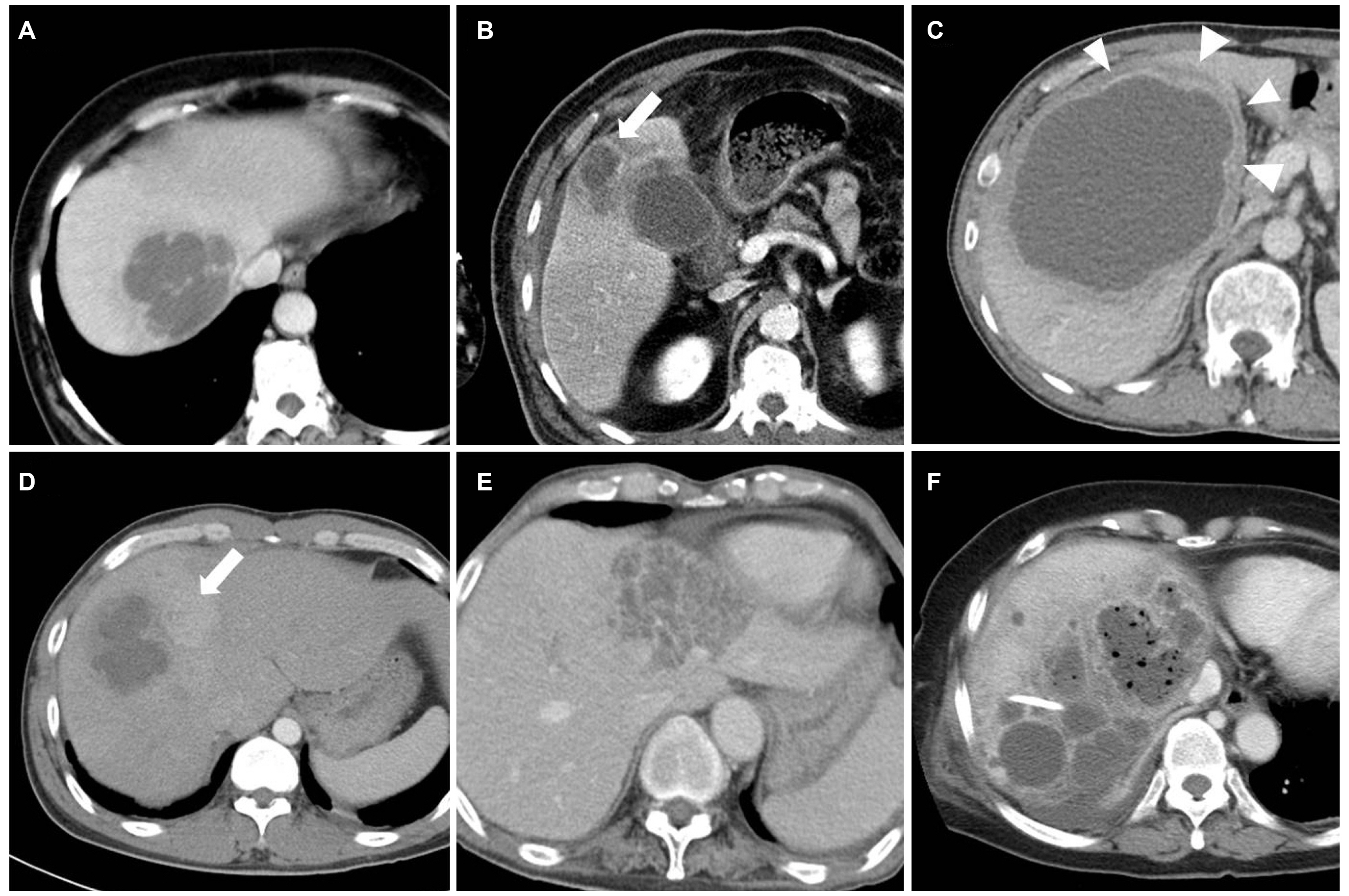
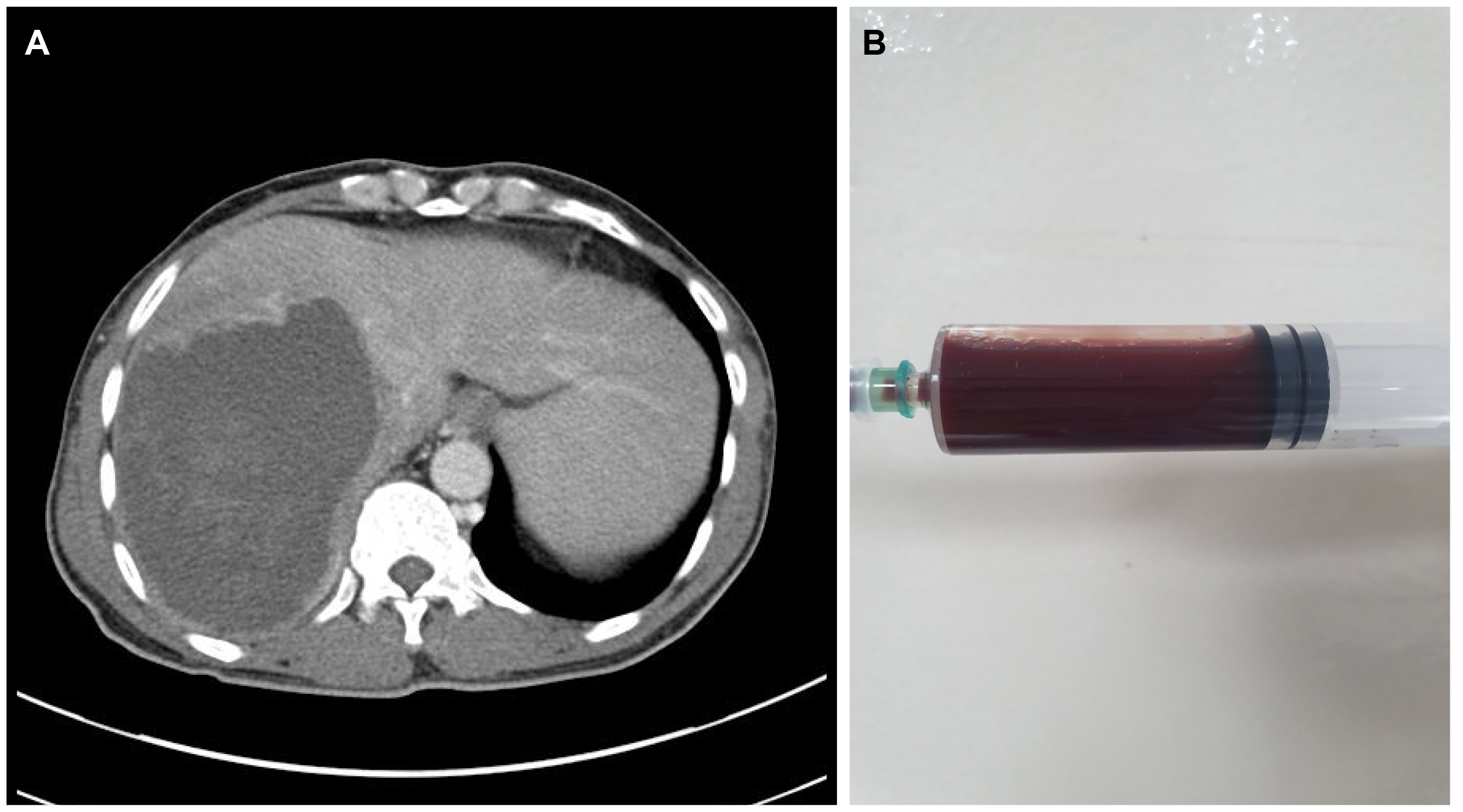
Between March 2010 and October 2016, 413 patients with a liver abscess were identified. Among them, the serologic test for E. histolytica was performed in 209 patients. Fifteen (7.2%) were classified as an amebic liver abscess, and the remainder were diagnosed with a pyogenic liver abscess. The age, gender, white blood cell, and CRP was comparable between the two groups. Procalcitonin was lower in amebic liver abscess than the pyogenic one. On CT, peripheral rim enhancement was more frequent, but cluster signs were not observed in amebic liver abscess compared to pyogenic liver abscess. None of the patients with amebic liver abscess died. In contrast, the mortality of pyogenic liver abscess was 4.7%.
Conclusions
Amebic liver abscess should still be considered as one of the causes of liver abscess in Korea. It is difficult to discriminate an amebic liver abscess from a pyogenic liver abscess only according to the clinical, laboratory, and radiologic findings. Therefore, it is necessary to perform a serologic test for E. histolytica for a precise evaluation of liver abscess in a high-risk group.
Figure
Cited by 1 articles
-
The Role of Serology Test in Diagnosis of Amebic Liver Abscess
Young Mi Hong
Korean J Gastroenterol. 2020;76(1):1-3. doi: 10.4166/kjg.2020.76.1.1.
Reference
-
1. Haque R, Huston CD, Hughes M, Houpt E, Petri WA Jr. 2003; Amebiasis. N Engl J Med. 348:1565–1573. DOI: 10.1056/NEJMra022710. PMID: 12700377.
Article2. Seo TJ, Park CH, Lee SH, et al. 2005; A clinical study on liver abscess for recent 15 years in gwangju·chonnam province. Korean J Med. 68:26–38.3. Kim KB, Na BS, Lee SH, et al. 2010; A case of amebic liver abscess with pleural effusion in an AIDS patient. Infect Chemother. 42:299–302. DOI: 10.3947/ic.2010.42.5.299.
Article4. Lee JH, Lee YM, Lee CH, Choi CS. 2009; The patient with amebic liver abscess should be suspect to be infected with HIV. Korean J Med. 77:55–56.5. Ahn JH, Kim TH, Choo EJ, et al. 2006; A case of amebic colitis and amebic liver abscess in HIV-infected patient. Korean J Med. 71(Suppl 3):S1170–S1174.6. Park WB, Choe PG, Jo JH, et al. 2007; Amebic liver abscess in HIV-infected patients, Republic of Korea. Emerg Infect Dis. 13:516–517. DOI: 10.3201/eid1303.060894. PMID: 17552123. PMCID: PMC2725887.
Article7. Kim YH, Park KS. 1980; A clinical study of liver abscess. Ann Surg Treat Res Soc. 22:51–61.8. Son GH, Lee CH, Choi KH, Lee SD, Seo JK, Park YH. 1988; Changing patterns of liver abscess. Ann Surg Treat Res Soc. 35:635–641.9. Cho JK, Kim MS, Shin JH, et al. 2013; Amebic liver abscess complicated with inferior vena cava obstruction. J Korean Geriatr Soc. 17:253–258. DOI: 10.4235/jkgs.2013.17.4.253.
Article10. Kim AY, Chung RT. Feldman M, Friedman LS, Brandt LJ, editors. 2016. Bacterial, parasitic, and fungal infections of the liver, including liver abscesses. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 10th ed. Saunders;Philadelphia: p. 1390–1392.11. Jung JS, Kim SY, Kim SH, Kim YW. 1970; Clinical observation on 75 cases of the liver abscess. Ann Surg Treat Res. 12:45–53.12. Yoo YU. 1978; Clinical study of liver abscess. Ann Surg Treat Res. 20:27–34.13. Lodhi S, Sarwari AR, Muzammil M, Salam A, Smego RA. 2004; Features distinguishing amoebic from pyogenic liver abscess: a review of 577 adult cases. Trop Med Int Health. 9:718–723. DOI: 10.1111/j.1365-3156.2004.01246.x. PMID: 15189463.
Article14. Greenstein AJ, Barth J, Dicker A, Bottone EJ, Aufses AH Jr. 1985; Amebic liver abscess: a study of 11 cases compared with a series of 38 patients with pyogenic liver abscess. Am J Gastroenterol. 80:472–478.15. Ralls PW, Barnes PF, Radin DR, Colletti P, Halls J. 1987; Sonographic features of amebic and pyogenic liver abscesses: a blinded comparison. AJR Am J Roentgenol. 149:499–501. DOI: 10.2214/ajr.149.3.499. PMID: 3303877.
Article16. Brant WE. Webb WR, Brant WE, Major NM, editors. 2020. Liver. Fundamentals of body CT. 5th ed. Elsevier;St. Louis: p. 236–237.
Article17. Kawamoto S, Soyer PA, Fishman EK, Bluemke DA. 1998; Nonneoplastic liver disease: evaluation with CT and MR imaging. Radiographics. 18:827–848. DOI: 10.1148/radiographics.18.4.9672968. PMID: 9672968.
Article18. Gabata T, Kadoya M, Matsui O, et al. 2001; Dynamic CT of hepatic abscesses:significance of transient segmental enhancement. AJR Am J Roentgenol. 176:675–679. DOI: 10.2214/ajr.176.3.1760675. PMID: 11222204.19. Jeffrey RB Jr, Tolentino CS, Chang FC, Federle MP. 1988; CT of small pyogenic hepatic abscesses: the cluster sign. AJR Am J Roentgenol. 151:487–489. DOI: 10.2214/ajr.151.3.487. PMID: 3261506.
Article20. Ma DW, Ju JW, Cho SH. 2019; Monitoring intestinal Protozoa causing water- and food-borne diarrhea in the Republic of Korea. Public Health Weekly Report. 12:1208–1211.21. Petri WA Jr, Haque R, Moonah SN. Bennett JE, Raphael D, Blaser MJ, editors. 2020. Entamoeba spcies, including amebic colitis and liver abscess. Mandell, Douglas, and Bennett's Principles and practice of infectious diseases. 9th ed. Elsevier;Philadelphia: p. 3273–3286.