Implication of the Life-Sustaining Treatment Decisions Act on End-of-Life Care for Korean Terminal Patients
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Center for Palliative Care and Clinical Ethics, Seoul National University Hospital, Seoul, Korea
- 3Department of Pediatrics, Seoul National University Hospital, Seoul, Korea
- 4Department of Psychiatry, Seoul National University Hospital, Seoul, Korea
- KMID: 2504470
- DOI: http://doi.org/10.4143/crt.2019.740
Abstract
- Purpose
Life-sustaining treatment (LST) decisions for patients and caregivers at the end-of-life (EOL) process are supported by the “Act on Hospice and Palliative Care and Decisions on LST for Patients at the EOL,” enforced in February 2018. Itremains unclearwhetherthe act changes EOL decisions and LST implementation in clinical practice. For this study, we investigated patients’ decision-making regarding LSTs during the EOL process since the act’s enforcement.
Materials and Methods
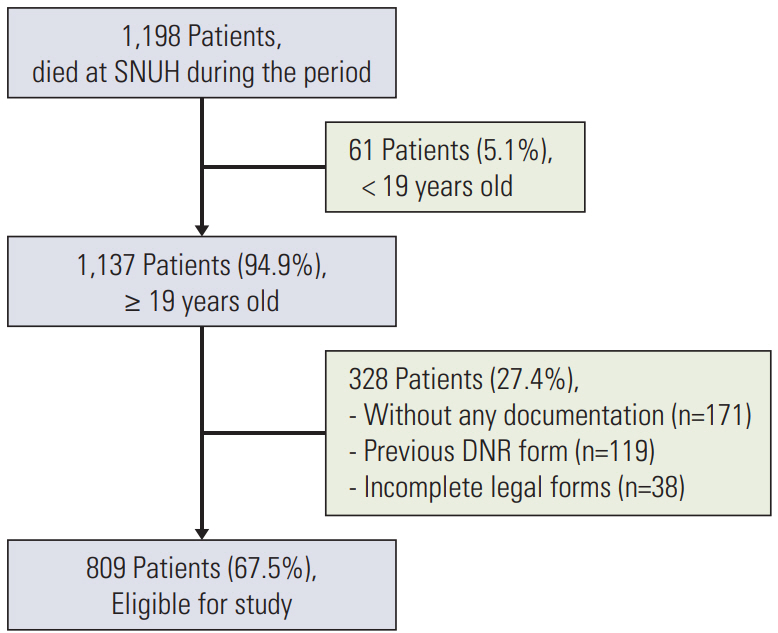
Retrospective reviews were conducted on adult patients who were able to decide to terminate LST and died at Seoul National University Hospital between February 5, 2018, and February 5, 2019. We examined demographics, who made the decisions, the type and date of documentation confirming patient's LST, and whether the LST was withheld or withdrawn.
Results
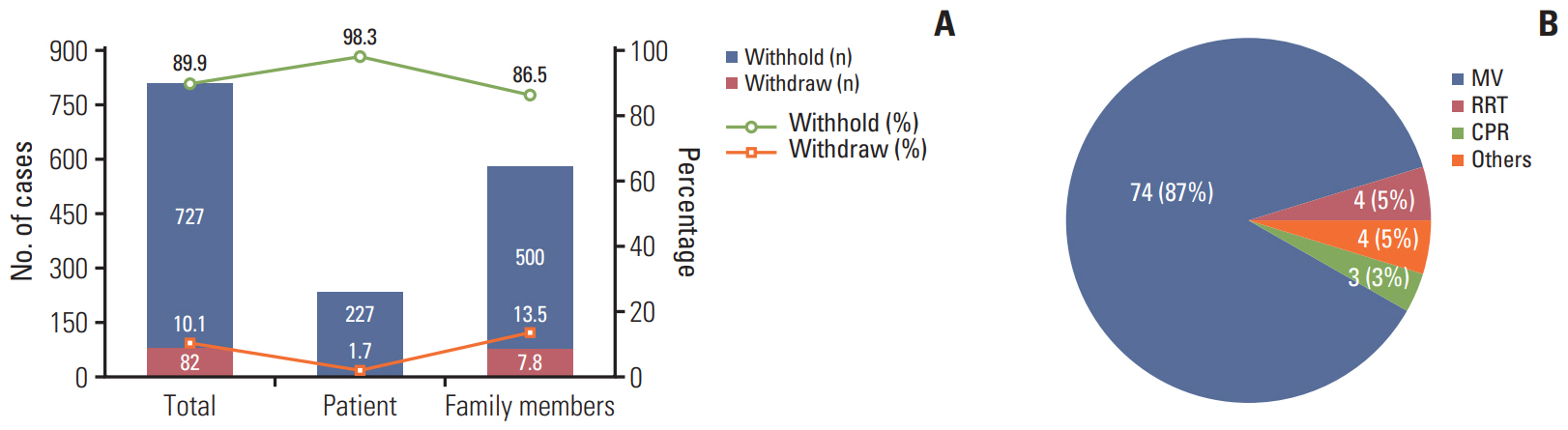
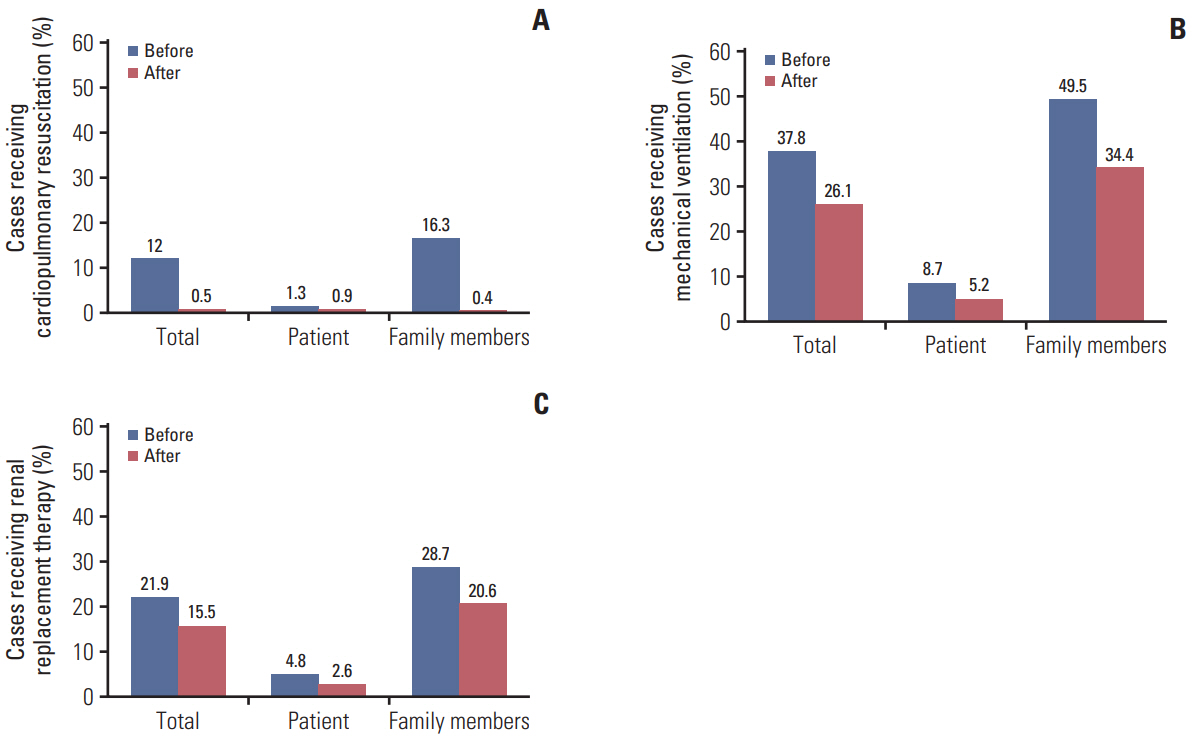
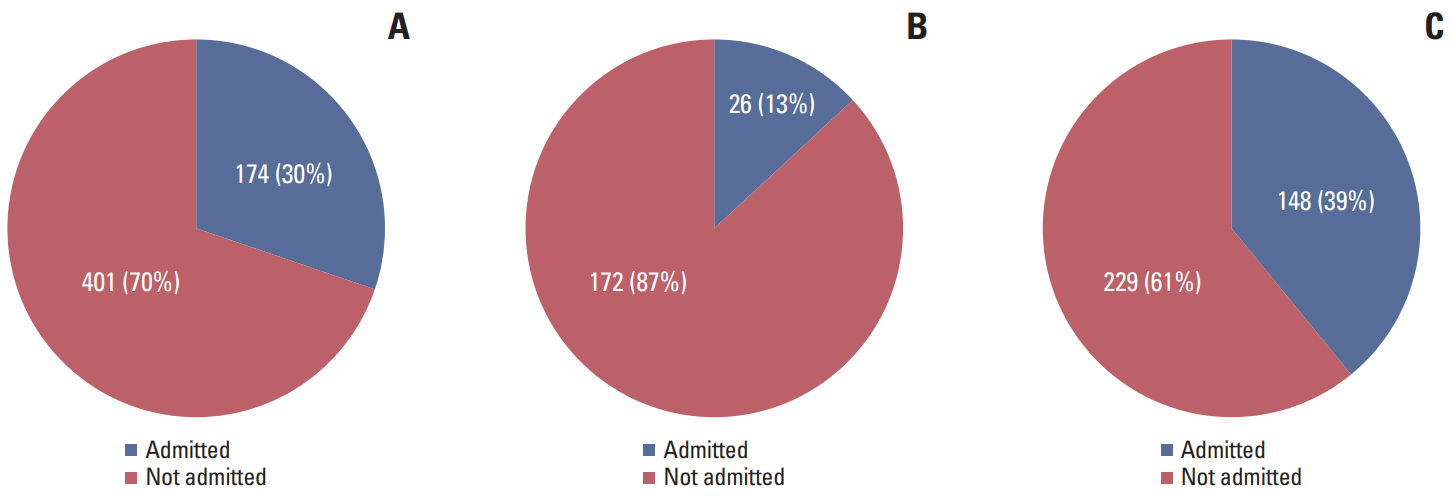
Of 809 patients who were enrolled, 29% (n=231) completed forms regarding LST themselves, and 71% (n=578) needed family members to decide. The median time from confirmation of the EOL process to death and from the Advance Statement to death were 2 and 5 days, respectively (both ranges, 0 to 244). In total, 90% (n=727) of patients withheld treatment, and 10% (n=82)withdrewit. We found a higherwithdrawalratewhen family members made the decisions (13.3% vs. 1.7%, p < 0.001).
Conclusion
After the act’s enforcement, withdrawing LSTs became lawful and self-determination rates increased. Family members still make 71% of decisions regarding LSTs, but these are often inconsistent with the patients’ wishes; thus, further efforts are needed to integrate the new act into clinical practice.
Figure
Cited by 12 articles
-
Difficulties Doctors Experience during Life-Sustaining Treatment Discussion after Enactment of the Life-Sustaining Treatment Decisions Act: A Cross-Sectional Study
Shin Hye Yoo, Wonho Choi, Yejin Kim, Min Sun Kim, Hye Yoon Park, Bhumsuk Keam, Dae Seog Heo
Cancer Res Treat. 2021;53(2):584-592. doi: 10.4143/crt.2020.735.A National Study of Life-Sustaining Treatments in South Korea: What Factors Affect Decision-Making?
So-Youn Park, Bomyee Lee, Jeong Yeon Seon, In-Hwan Oh
Cancer Res Treat. 2021;53(2):593-600. doi: 10.4143/crt.2020.803.Life-Sustaining Treatment States in Korean Cancer Patients after Enforcement of Act on Decisions on Life-Sustaining Treatment for Patients at the End of Life
Young-Woong Won, Hwa Jung Kim, Jung Hye Kwon, Ha Yeon Lee, Sun Kyung Baek, Yu Jung Kim, Do Yeun Kim, Hyewon Ryu
Cancer Res Treat. 2021;53(4):908-916. doi: 10.4143/crt.2021.325.Preparation and Practice of the Necessary Documents in Hospital for the “Act on Decision of Life-Sustaining Treatment for Patients at the End-of-Life”
Sun Kyung Baek, Hwa Jung Kim, Jung Hye Kwon, Ha Yeon Lee, Young-Woong Won, Yu Jung Kim, Sujin Baik, Hyewon Ryu
Cancer Res Treat. 2021;53(4):926-934. doi: 10.4143/crt.2021.326.Current Status and Cardinal Features of Patient Autonomy after Enactment of the Life-Sustaining Treatment Decisions Act in Korea
Hwa Jung Kim, Yu Jung Kim, Jung Hye Kwon, Young-Woong Won, Ha Yeon Lee, Sun Kyung Baek, Hyewon Ryu, Do Yeun Kim
Cancer Res Treat. 2021;53(4):917-925. doi: 10.4143/crt.2021.324.The Situation of Life-Sustaining Treatment One Year after Enforcement of the Act on Decisions on Life-Sustaining Treatment for Patients at the End-of-Life in Korea: Data of National Agency for Management of Life-Sustaining Treatment
Ha Yeon Lee, Hwa Jung Kim, Jung Hye Kwon, Sun Kyung Baek, Young-Woong Won, Yu Jung Kim, Su Jin Baik, Hyewon Ryu
Cancer Res Treat. 2021;53(4):897-907. doi: 10.4143/crt.2021.327.Analysis of Cancer Patient Decision-Making and Health Service Utilization after Enforcement of the Life-Sustaining Treatment Decision-Making Act in Korea
Dalyong Kim, Shin Hye Yoo, Seyoung Seo, Hyun Jung Lee, Min Sun Kim, Sung Joon Shin, Chi-Yeon Lim, Do Yeun Kim, Dae Seog Heo, Chae-Man Lim
Cancer Res Treat. 2022;54(1):20-29. doi: 10.4143/crt.2021.131.Changes in the incidence of cardiopulmonary resuscitation before and after implementation of the Life-Sustaining Treatment Decisions Act
Hyunjae Im, Hyun Woo Choe, Seung-Young Oh, Ho Geol Ryu, Hannah Lee
Acute Crit Care. 2022;37(2):237-246. doi: 10.4266/acc.2021.01095.Will implementation of the Life-Sustaining Treatment Decisions Act reduce the incidence of cardiopulmonary resuscitation?
In-Ae Song
Acute Crit Care. 2022;37(2):256-257. doi: 10.4266/acc.2022.00668.Recent Trends in the Withdrawal of Life-Sustaining Treatment in Patients with Acute Cerebrovascular Disease : 2017–2021
Seung Hwan Kim, Ji Hwan Jang, Young Zoon Kim, Kyu Hong Kim, Taek Min Nam
J Korean Neurosurg Soc. 2024;67(1):73-83. doi: 10.3340/jkns.2023.0074.Comparison of factors influencing the decision to withdraw life-sustaining treatment in intensive care unit patients after implementation of the Life-Sustaining Treatment Act in Korea
Claire Junga Kim, Kyung Sook Hong, Sooyoung Cho, Jin Park
Acute Crit Care. 2024;39(2):294-303. doi: 10.4266/acc.2023.01130.End-of-life care in the intensive care unit: the optimal process of decision to withdrawing life-sustaining treatment based on the Korean medical environment and culture
Ho Jin Yong, Dohhyung Kim
Acute Crit Care. 2024;39(2):321-322. doi: 10.4266/acc.2024.00675.
Reference
-
References
1. Lee SJ, Fairclough D, Antin JH, Weeks JC. Discrepancies between patient and physician estimates for the success of stem cell transplantation. JAMA. 2001; 285:1034–8.
Article2. Matsuyama R, Reddy S, Smith TJ. Why do patients choose chemotherapy near the end of life? A review of the perspective of those facing death from cancer. J Clin Oncol. 2006; 24:3490–6.
Article3. Choi Y, Keam B, Kim TM, Lee SH, Kim DW, Heo DS. Cancer treatment near the end-of-life becomes more aggressive: changes in trend during 10 years at a single institute. Cancer Res Treat. 2015; 47:555–63.
Article4. Farber SJ, Egnew TR, Herman-Bertsch JL, Taylor TR, Guldin GE. Issues in end-of-life care: patient, caregiver, and clinician perceptions. J Palliat Med. 2003; 6:19–31.
Article5. Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004; 170:1795–801.
Article6. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients' perspectives. JAMA. 1999; 281:163–8.7. Oh DY, Kim JH, Kim DW, Im SA, Kim TY, Heo DS, et al. CPR or DNR? End-of-life decision in Korean cancer patients: a single center's experience. Support Care Cancer. 2006; 14:103–8.
Article8. Kim DY, Lee KE, Nam EM, Lee HR, Lee KW, Kim JH, et al. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med. 2007; 10:1153–8.
Article9. Jho HJ, Nam EJ, Shin IW, Kim SY. Changes of end of life practices for cancer patients and their association with hospice palliative care referral over 2009-2014: a single institution study. Cancer Res Treat. 2019; 52:419–25.
Article10. Baek SK, Chang HJ, Byun JM, Han JJ, Heo DS. The association between end-of-life care and the time interval between provision of a do-not-resuscitate consent and death in cancer patients in Korea. Cancer Res Treat. 2017; 49:502–8.
Article11. Lee JK, Keam B, An AR, Kim TM, Lee SH, Kim DW, et al. Surrogate decision-making in Korean patients with advanced cancer: a longitudinal study. Support Care Cancer. 2013; 21:183–90.
Article12. Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life, No. 14013 (Feb 3, 2016).13. Hui D, Nooruddin Z, Didwaniya N, Dev R, De La Cruz M, Kim SH, et al. Concepts and definitions for "actively dying," "end of life," "terminally ill," "terminal care," and "transition of care": a systematic review. J Pain Symptom Manage. 2014; 47:77–89.
Article14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article15. Kim DY, Lee SM, Lee KE, Lee HR, Kim JH, Lee KW, et al. An evaluation of nutrition support for terminal cancer patients at teaching hospitals in Korea. Cancer Res Treat. 2006; 38:214–7.
Article16. Yun YH, Kwon YC, Lee MK, Lee WJ, Jung KH, Do YR, et al. Experiences and attitudes of patients with terminal cancer and their family caregivers toward the disclosure of terminal illness. J Clin Oncol. 2010; 28:1950–7.
Article17. Park HY, Kim YA, Sim JA, Lee J, Ryu H, Lee JL, et al. Attitudes of the general public, cancer patients, family caregivers, and physicians toward advance care planning: a nationwide survey before the enforcement of the life-sustaining treatment decision-making act. J Pain Symptom Manage. 2019; 57:774–82.
Article18. Yoo SH, Keam B, Kim M, Kim TM, Kim DW, Heo DS. The effect of hospice consultation on aggressive treatment of lung cancer. Cancer Res Treat. 2018; 50:720–8.
Article19. Levin TT, Li Y, Weiner JS, Lewis F, Bartell A, Piercy J, et al. How do-not-resuscitate orders are utilized in cancer patients: timing relative to death and communication-training implications. Palliat Support Care. 2008; 6:341–8.
Article20. van der Heide A, Deliens L, Faisst K, Nilstun T, Norup M, Paci E, et al. End-of-life decision-making in six European countries: descriptive study. Lancet. 2003; 362:345–50.
Article21. Sprung CL, Eidelman LA. Worldwide similarities and differences in the foregoing of life-sustaining treatments. Intensive Care Med. 1996; 22:1003–5.22. Way J, Back AL, Curtis JR. Withdrawing life support and resolution of conflict with families. BMJ. 2002; 325:1342–5.
Article23. Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015; 175:363–71.
Article24. Kong BH, An HJ, Kim HS, Ha SY, Kim IK, Lee JE, et al. Experience of advance directives in a hospice center. J Korean Med Sci. 2015; 30:151–4.
Article25. Hong JH, Kwon JH, Kim IK, Ko JH, Kang YJ, Kim HK. Adopting advance directives reinforces patient participation in end-of-life care discussion. Cancer Res Treat. 2016; 48:753–8.
Article26. Koh SJ, Kim S, Kim J, Keam B, Heo DS, Lee KH, et al. Experiences and opinions related to end-of-life discussion: from oncologists' and resident physicians' perspectives. Cancer Res Treat. 2018; 50:614–23.
Article27. Sohn KH, Nam S, Joo J, Kwon YJ, Yim JJ. Patient-centeredness during in-depth consultation in the outpatient clinic of a tertiary hospital in Korea: paradigm shift from disease to patient. J Korean Med Sci. 2019; 34:e119.
Article28. Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008; 300:1665–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hemodialysis as a life-sustaining treatment at the end of life
- Implementation of Antimicrobial Stewardship Programs in End-of-Life Care
- Life-Sustaining Treatment in End-Stage Liver Disease Patients: Patients’ Decisions and Results
- Problems Related to the Act on Decisions on Life-Sustaining Treatment and Directions for Improvement
- Well-Dying: Assisted Justice Act as a Dignified and Happy ‘Right to Self-Determination’