J Cerebrovasc Endovasc Neurosurg.
2020 Jun;22(2):85-89. 10.7461/jcen.2020.22.2.85.
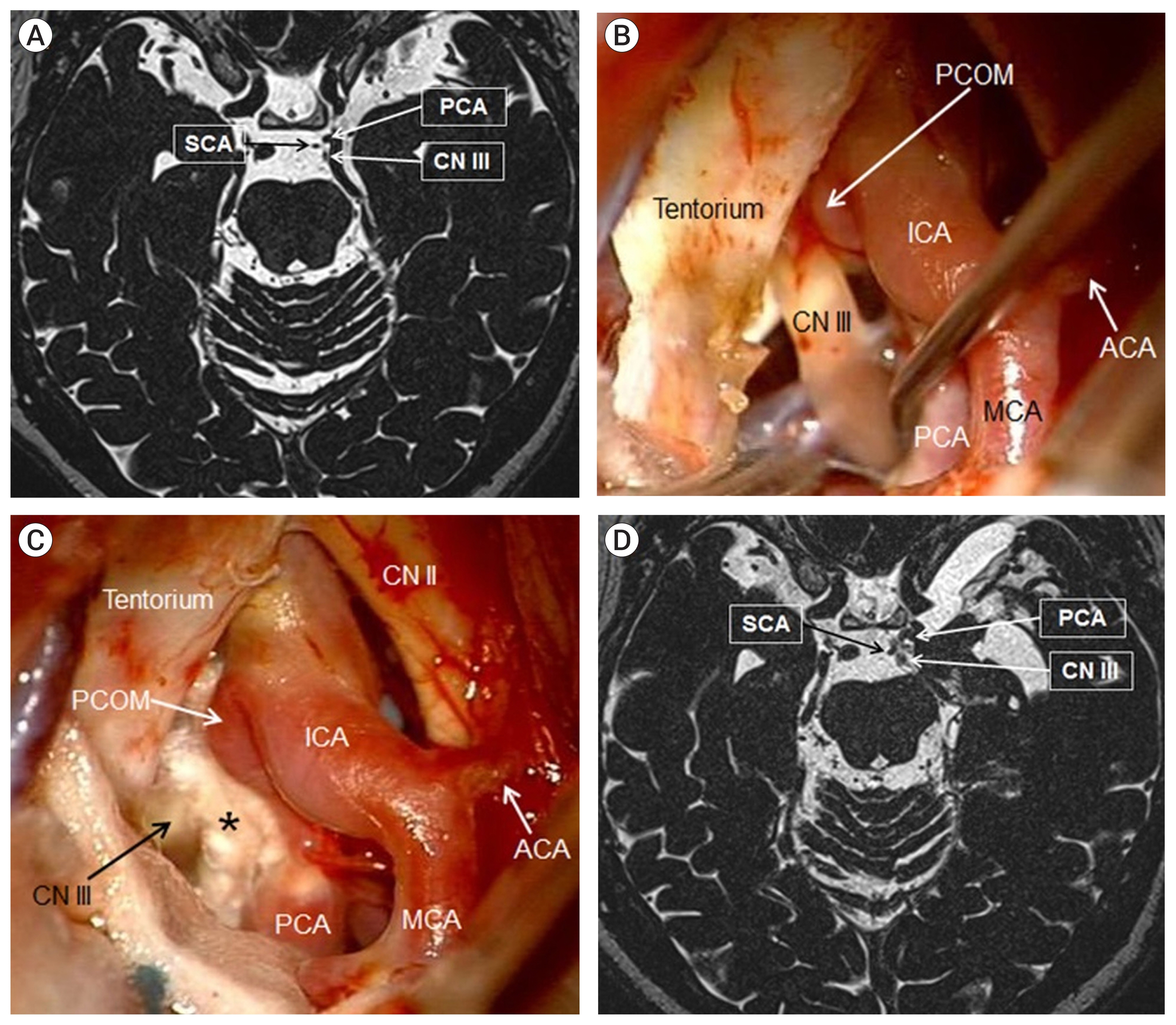
Microvascular decompression of the posterior cerebral artery for treatment of oculomotor nerve palsy
- Affiliations
-
- 1National Institute of Neurological Disorders and Stroke, Surgical Neurology Branch, National Institutes of Health, Bethesda, MD, USA
- 2Department of Neurological Surgery, University of Louisville School of Medicine, Louisville, KY, USA
- 3Department of Neurosurgery, University of Maryland School of Medicine, Baltimore, MD, USA
- 4Department of Neurological Surgery, University of Southern California, Los Angeles, CA, USA
- KMID: 2503821
- DOI: http://doi.org/10.7461/jcen.2020.22.2.85
Abstract
- Oculomotor nerve palsy resulting from non-aneurysmal vascular compression is extremely rare. Microvascular decompression (MVD) has been previously shown to improve oculomotor nerve palsy (ONP) secondary to arterial compression. A 71-year-old female, with a history of Cushing’s disease previously treated with two transsphenoidal resections and Gamma Knife radiosurgery, presented with one year of progressive left eye diplopia and was diagnosed with a partial left oculomotor nerve palsy. We performed an orbitozygomatic craniotomy for MVD of the left posterior cerebral artery, which was found to be compressing the oculomotor nerve against the tentorium. Unfortunately, the patient’s partial ONP remained unchanged at one year follow-up. The present case suggests inconsistent outcomes of MVD for ONP. Patients with prior sellar or parasellar irradiation may be less likely to benefit from this treatment approach.
Keyword
Figure
Reference
-
1. Albayram S, Ozer H, Sarici A, Murphy K, Miller N. Unilateral mydriasis without ophthalmoplegia--a sign of neurovascular compression? Case report. Neurosurgery. 2006; Mar. 58(3):E582–3. discussion E582–3.
Article2. Babbitz JD, Harsh GR 4th. Concomitant ectatic posterior communicating artery and tentorial meningioma as a source of oculomotor palsy: case report. Neurosurgery. 2005; Dec. 57(6):E1316. discussion E1316.
Article3. D’Andrea F, Maiuri F, Gangemi M, Iaconetta G. Megadolichobasilar anomaly. Clinical and diagnostic considerations on 30 cases. Acta Neurol (Napoli). 1992; Aug–Dec. 14(4–6):611–9.4. Ding D, Starke RM, Kano H, Nakaji P, Barnett GH, Mathieu D, et al. Gamma knife radiosurgery for cerebellopontine angle meningiomas: a multicenter study. Neurosurgery. 2014; Oct. 75(4):398–408. quiz 408.5. Ding D, Starke RM, Sheehan JP. Treatment paradigms for pituitary adenomas: defining the roles of radiosurgery and radiation therapy. J Neurooncol. 2014; May. 117(3):445–57.
Article6. Ding D, Yen CP, Starke RM, Lee CC, Sheehan JP. Unyielding progress: recent advances in the treatment of central nervous system neoplasms with radiosurgery and radiation therapy. J Neurooncol. 2014; Sep. 119(3):513–29.
Article7. Giombini S, Ferraresi S, Pluchino F. Reversal of oculomotor disorders after intracranial aneurysm surgery. Acta Neurochir (Wien). 1991; 112(1–2):19–24.
Article8. Hamer J. Prognosis of oculomotor palsy in patients with aneurysms of the posterior communicating artery. Acta Neurochir (Wien). 1982; 66(3–4):173–85.
Article9. Hashimoto M, Ohtsuka K, Akiba H, Harada K. Vascular compression of the oculomotor nerve disclosed by thin-slice magnetic resonance imaging. Am J Ophthalmol. 1998; Jun. 125(6):881–2.
Article10. Imes RK, Monteiro ML, Hoyt WF. Ophthalmoplegic migraine with proximal posterior cerebral artery vascular anomaly. J Clin Neuroophthalmol. 1984; Dec. 4(4):221–3.11. Kojo N, Lee S, Otsuru K, Takagi S, Shigemori M, Watanabe M. A case of ophthalmoplegic migraine with cerebral aneurysm. No Shinkei Geka. 1988; 16(5 Suppl):503–7.12. Leivo S, Hernesniemi J, Luukkonen M, Vapalahti M. Early surgery improves the cure of aneurysm-induced oculomotor palsy. Surg Neurol. 1996; May. 45(5):430–4.
Article13. Morimoto K, Nagatani M, Mogami H. A case simulating ophthalmoplegic migraine: clinicopathological study. Headache. 1985; Nov. 25(8):426–8.14. Nakagawa H, Nakajima S, Nakajima Y, Furuta Y, Nishi O, Nishi K. Bilateral oculomotor nerve palsies due to posterior cerebral arterial compression relieved by microvascular decompression--case report. Neurol Med Chir (Tokyo). 1991; Jan. 31(1):45–8.15. Peerless SJ, Hernesniemi JA, Gutman FB, Drake CG. Early surgery for ruptured vertebrobasilar aneurysms. J Neurosurg. 1994; Apr. 80(4):643–9.
Article16. Starke R, Kano H, Ding D, Nakaji P, Barnett GH, Mathieu D, et al. Stereotactic radiosurgery of petroclival meningiomas: a multicenter study. J Neurooncol. 2014; Aug. 119(1):169–76.
Article17. Starke RM, Przybylowski CJ, Sugoto M, Fezeu F, Awad AJ, Ding D, et al. Gamma Knife radiosurgery of large skull base meningiomas. J Neurosurg. 2015; Feb. 122(2):363–72.
Article18. Suzuki K, Muroi A, Kujiraoka Y, Takano S, Matsumura A. Oculomotor palsy treated by microvascular decompression. Surg Neurol. 2008; Aug. 70(2):210–2.
Article19. Zingale A, Chiaramonte I, Mancuso P, Consoli V, Albanese V. Craniofacial pain and incomplete oculomotor palsy associated with ipsilateral primitive trigeminal artery. Case report. J Neurosurg Sci. 1993; Dec. 37(4):251–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Giant Fusiform Aneurysm of Posterior Cerebral Artery Treated with Trapping after Temporal Lobectomy
- Pituitary Apoplexy Presenting as Isolated Oculomotor Nerve Palsy
- Oculomotor Nerve Palsy in Internal Carotid-Posterior Communicating Artery Aneurysm
- Oculomotor Nerve Palsy Associated with Rupture of Middle Cerebral Artery Aneurysm
- Resolution of Isolated Unilateral Hypoglossal Nerve Palsy Following Microvascular Decompression of the Intracranial Vertebral Artery