Effect of Underlying Comorbidities on the Infection and Severity of COVID-19 in Korea: a Nationwide Case-Control Study
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Division of Infectious Diseases, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Artificial Intelligence and Big-Data Convergence Center, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 4Department of Preventive Medicine, Gachon University College of Medicine, Incheon, Korea
- KMID: 2503664
- DOI: http://doi.org/10.3346/jkms.2020.35.e237
Abstract
- Background
The coronavirus disease 2019 (COVID-19) pandemic is an emerging threat worldwide. It remains unclear how comorbidities affect the risk of infection and severity of COVID-19.
Methods
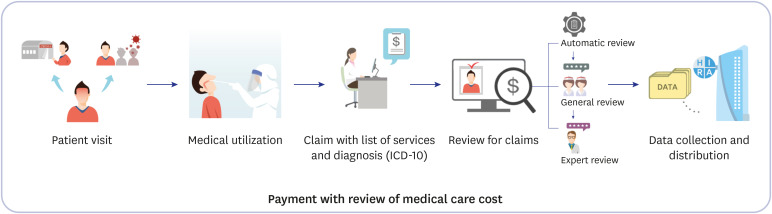
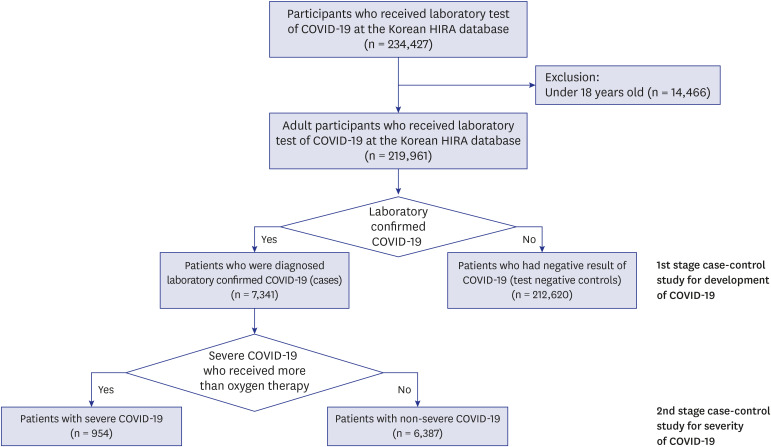
This is a nationwide retrospective case-control study of 219,961 individuals, aged 18 years or older, whose medical costs for COVID-19 testing were claimed until May 15, 2020. COVID-19 diagnosis and infection severity were identified from reimbursement data using diagnosis codes and on the basis of respiratory support use, respectively. Odds ratios (ORs) were estimated using multiple logistic regression, after adjusting for age, sex, region, healthcare utilization, and insurance status.
Results
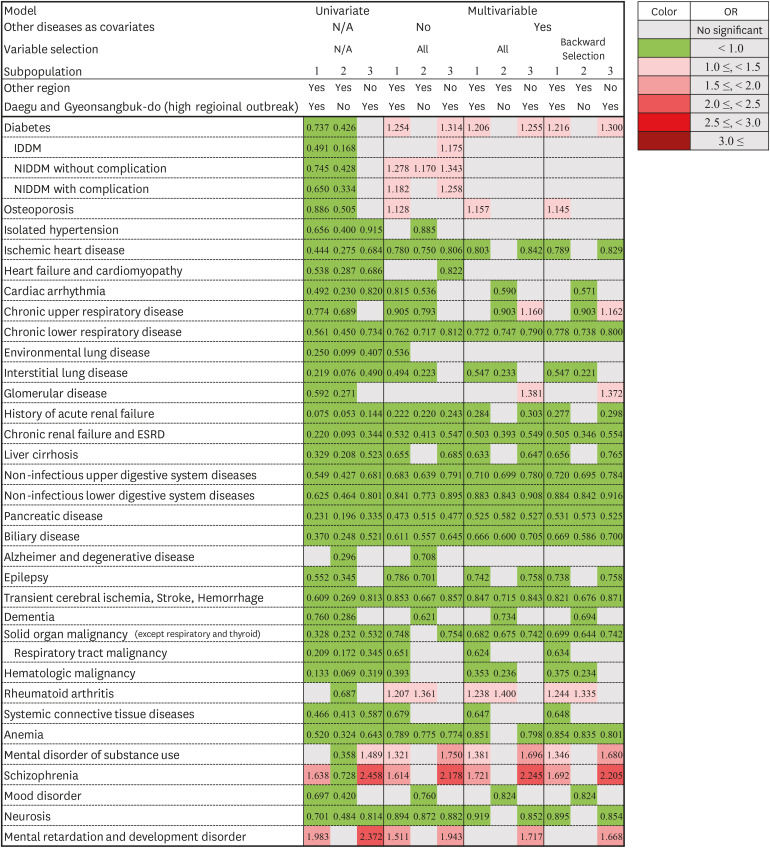
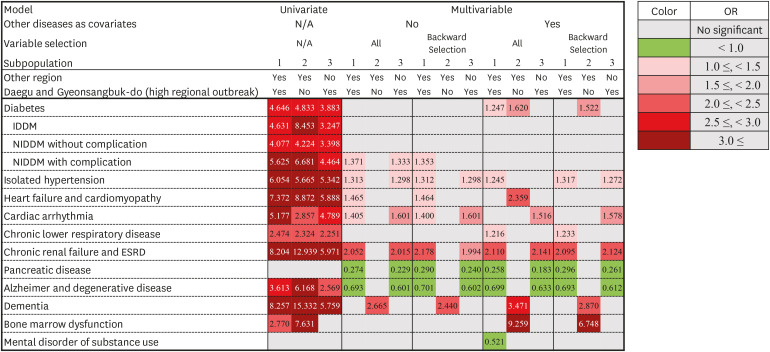
The COVID-19 group (7,341 of 219,961) was young and had a high proportion of female. Overall, 13.0% (954 of 7,341) of the cases were severe. The severe COVID-19 group had older patients and a proportion of male ratio than did the non-severe group. Diabetes (odds ratio range [ORR], 1.206–1.254), osteoporosis (ORR, 1.128–1.157), rheumatoid arthritis (ORR, 1.207–1.244), substance use (ORR, 1.321–1.381), and schizophrenia (ORR, 1.614–1.721) showed significant association with COVID-19. In terms of severity, diabetes (OR, 1.247; 95% confidential interval, 1.009–1.543), hypertension (ORR, 1.245–1.317), chronic lower respiratory disease (ORR, 1.216–1.233), chronic renal failure, and end-stage renal disease (ORR, 2.052–2.178) were associated with severe COVID-19.
Conclusion
We identified several comorbidities associated with COVID-19. Health care workers should be more careful while diagnosing and treating COVID-19 when patients have the abovementioned comorbidities.
Keyword
Figure
Cited by 4 articles
-
Coping with Dementia in the Middle of the COVID-19 Pandemic
Nayoung Ryoo, Jung-Min Pyun, Min Jae Baek, Jeewon Suh, Min Ju Kang, Min Jeong Wang, Young Chul Youn, Dong Won Yang, Seong Yoon Kim, Young Ho Park, SangYun Kim
J Korean Med Sci. 2020;35(42):e383. doi: 10.3346/jkms.2020.35.e383.Developing a Framework for Pandemic COVID-19 Vaccine Allocation: a Modified Delphi Consensus Study in Korea
Min Joo Choi, Won Suk Choi, Hye Seong, Jun Yong Choi, Jong-Hyun Kim, Yae-Jean Kim, Eun Young Cho, Dong-Hyun Kim, Hyesook Park, Heeyoung Lee, Nam Joong Kim, Joon Young Song, Hee Jin Cheong, Sang Il Kim, Kyong Ran Peck
J Korean Med Sci. 2021;36(23):e166. doi: 10.3346/jkms.2021.36.e166.A Long Way to the Recovery: COVID-19 Will Not Disappear
Jaehun Jung
J Korean Med Sci. 2021;36(32):e231. doi: 10.3346/jkms.2021.36.e231.Risk for Newly Diagnosed Type 2 Diabetes Mellitus after COVID-19 among Korean Adults: A Nationwide Matched Cohort Study
Jong Han Choi, Kyoung Min Kim, Keeho Song, Gi Hyeon Seo
Endocrinol Metab. 2023;38(2):245-252. doi: 10.3803/EnM.2023.1662.
Reference
-
1. World Health Organization. Coronavirus disease 2019 (COVID-19) situation report. Updated 2020. Accessed May 24, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/.2. Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020; 8(1):e35. PMID: 32232218.3. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94:91–95. PMID: 32173574.
Article4. Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020; 55(5):2000547. PMID: 32217650.
Article5. Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. Forthcoming. 2020; DOI: 10.1016/j.jaci.2020.04.006.
Article6. Jung J, Im JH, Ko YJ, Huh K, Yoon CG, Rhee C, et al. Complementing conventional infectious disease surveillance with national health insurance claims data in the Republic of Korea. Sci Rep. 2019; 9(1):8750. PMID: 31217476.
Article7. Korea Centers for Disease Control & Prevention. Coronavirus disease-19 in South Korea. Updated 2020. Accessed April 21, 2020. http://ncov.mohw.go.kr/.8. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.
Article9. Kim I, Lee J, Lee J, Shin E, Chu C, Lee SK. KCDC risk assessments on the initial phase of the COVID-19 outbreak in Korea. Osong Public Health Res Perspect. 2020; 11(2):67–73. PMID: 32257771.
Article10. COVID-19 National Emergency Response Center, Epidemiology & Case Management Team, Korea Centers for Disease Control & Prevention. Contact transmission of COVID-19 in South Korea: novel investigation techniques for tracing contacts. Osong Public Health Res Perspect. 2020; 11(1):60–63. PMID: 32149043.11. Her M. How is COVID-19 affecting South Korea? What is our current strategy? Disaster Med Public Health Prep. Forthcoming. 2020; DOI: 10.1017/dmp.2020.69.
Article12. Chung RY, Dong D, Li MM. Socioeconomic gradient in health and the covid-19 outbreak. BMJ. 2020; 369:m1329. PMID: 32238351.
Article13. Luo Y, Zhang L, He P, Pang L, Guo C, Zheng X. Individual-level and area-level socioeconomic status (SES) and schizophrenia: cross-sectional analyses using the evidence from 1.9 million Chinese adults. BMJ Open. 2019; 9(9):e026532.
Article14. Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. Forthcoming. 2020; DOI: 10.1002/dmrr.3319.15. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med. 2020; 382(21):2012–2022. PMID: 32227758.
Article16. Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020; 24(1):108. PMID: 32188484.
Article17. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020; 579(7798):270–273. PMID: 32015507.18. Zeng JH, Liu YX, Yuan J, Wang FX, Wu WB, Li JX, et al. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection. Forthcoming. 2020; DOI: 10.1007/s15010-020-01424-5.
Article19. Kim IC, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020; 41(19):1859. PMID: 32282027.
Article20. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020; 181(2):271–280.e8. PMID: 32142651.
Article21. Zhou Y, Vedantham P, Lu K, Agudelo J, Carrion R Jr, Nunneley JW, et al. Protease inhibitors targeting coronavirus and filovirus entry. Antiviral Res. 2015; 116:76–84. PMID: 25666761.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Treatments of Coronavirus Disease 2019 in Elderly
- Management of Patients with Chronic Liver Disease: The Era of the COVID-19 Pandemic
- Factors Affecting Compliance of Infection Control of Coronavirus Disease 2019 among Nurses Based on Health Belief Model
- Hospital Infection Control Practice in the COVID-19 Era: An Experience of University Affiliated Hospital
- Vitamin D Deficiency and Comorbidities as Risk Factors of COVID-19 Infection: A Systematic Review and Meta-analysis