J Rhinol.
2020 May;27(1):41-45. 10.18787/jr.2019.00307.
Endoscopic Resection of Functional Paraganglioma of the Pterygopalatine Fossa: A Case Report
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2502793
- DOI: http://doi.org/10.18787/jr.2019.00307
Abstract
- Functional paraganglioma is a rare tumor that secretes the catecholamine which is able to cause secondary hypertension. Surgical resection is the only curative treatment modality for this tumor, which can correct the secondary hypertension. The pterygopalatine fossa is a small retromaxillary space which contains a neurovascular bundle that crosses the middle cranial fossa to the nasal cavity, nasal septum, and oral cavity. To our knowledge, two cases have been reported for functional paraganglioma involving the pterygopalatine fossa removed by surgery. We present a patient who had a catecholamine-secreting paraganglioma in the pterygopalatine fossa, which is the first case successfully resected with an endoscopic approach.
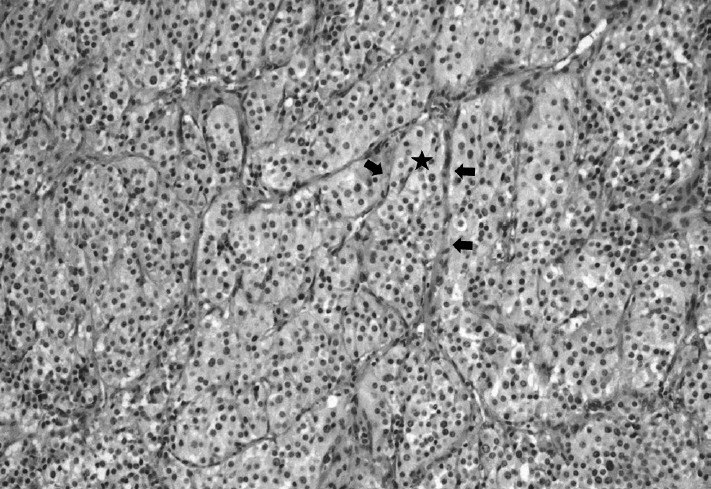
Figure
Reference
-
1. Wasserman PG, Savargaonkar P. Paragangliomas: classification, pathology, and differential diagnosis. Otolaryngol Clin North Am. 2001; 34(5):845–62. v-vi.2. Young WF Jr. Paragangliomas: clinical overview. Ann N Y Acad Sci. 2006; 1073:21–9.3. Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Curr Probl Cancer. 2014; 38(1):7–41.4. Boedeker CC, Ridder GJ, Schipper J. Paragangliomas of the head and neck: diagnosis and treatment. Fam Cancer. 2005; 4(1):55–9.5. Williams MD. Paragangliomas of the head and neck: an overview from diagnosis to genetics. Head Neck Pathol. 2017; 11(3):278–87.6. Hayward N, Cousins V. Head and neck paraganglioma: medical assessment, management, and literature update. J Otorhinolaryngol Hear Balance Med. 2018; 1:4.7. Walker PJ, Fagan PA. Catecholamine-secreting paraganglioma of the pterygopalatine fossa: case report. Am J Otol. 1993; 14(3):306–8.8. Otokida K, Ohira A, Kamimura A, Fujimori M, Kato M, et al. Cervical cathecolamine-secreting paraganglioma in the pterygopalatine fossa. Tohoku J Exp Med. 1987; 153(4):347–54.9. White JB, Link MJ, Cloft HJ. Endovascular embolization of paragangliomas: a safe adjuvant to treatment. J Vasc Interv Neurol. 2008; 1(2):37–41.10. Tashi S, Purohit BS, Becker M, Mundada P. The pterygopalatine fossa: imaging anatomy, communications, and pathology revisited. Insights Imaging. 2016; 7(4):589–99.11. DelGaudio JM. Endoscopic transnasal approach to the pterygopalatine fossa. Arch Otolaryngol Head Neck Surg. 2003; 129(4):441–6.12. Hofstetter CP, Singh A, Anand VK, Kacker A, Schwartz TH. The endoscopic, endonasal, transmaxillary transpterygoid approach to the pterygopalatine fossa, infratemporal fossa, petrous apex, and the Meckel cave. J Neurosurg. 2010; 113(5):967–74.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transnasal Endoscopic Resection of Juvenile Nasopharyngeal Angiofibroma: A Case Report
- Periampullary Gangliocytic Paraganglioma Successfully Treated by Endoscopic Mucosal Resection
- Resection Via Transpalatal Approach of Huge Solitary Fibrous Tumor Involving Pterygopalatine Fossa
- A Case of Malignant Fibrous Histiocytoma of the Pterygopalatine Fossa
- A Case of Neurofibroma of the Orbit and Pterygopalatine Fossa