Clin Endosc.
2020 May;53(3):355-360. 10.5946/ce.2019.113.
Endoscopic Therapy for Pancreatic Fluid Collections: A Definitive Management Using a Dedicated Algorithm
- Affiliations
-
- 1Division of Gastroenterology, Southern California Permanente Medical Group, Los Angeles, CA, USA
- 2Division of Gastroenterology, Rutgers University, Robert Wood Johnson Medical School, New Brunswick, NJ, USA
- 3Division of Gastroenterology, Thomas Jefferson University Hospital, Philadelphia, PA, USA
- 4Division of Gastroenterology, Weill Cornell Medical College, New York, NY, USA
- KMID: 2502771
- DOI: http://doi.org/10.5946/ce.2019.113
Abstract
- Background/Aims
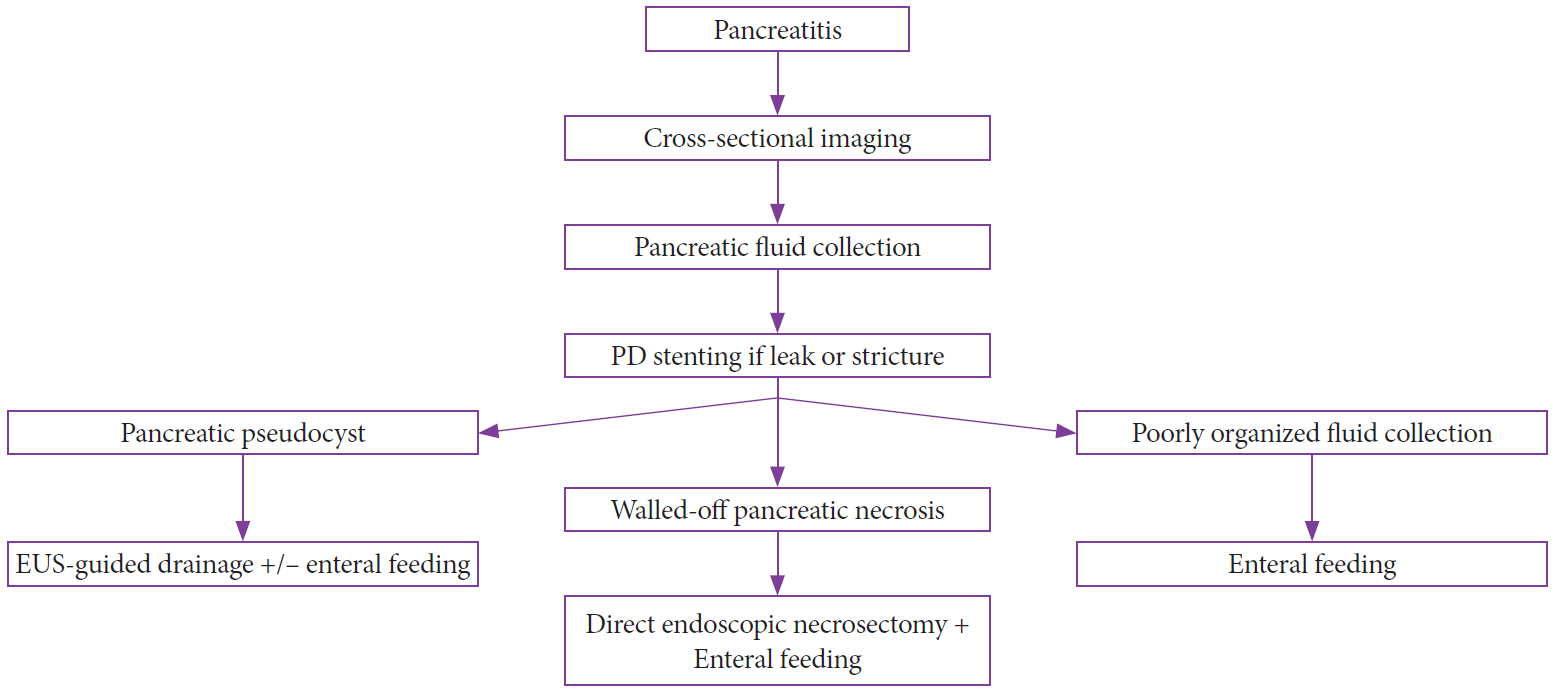
Endoscopic ultrasonography (EUS)-guided drainage is the preferred approach for infected or symptomatic pancreatic fluid collections (PFCs). Here, we developed an algorithm for the management of pancreatitis complicated by PFCs and report on its effcacy and safety.
Methods
Between September 2011 and October 2017, patients were prospectively managed according to the algorithm. PFCs were classified as poorly organized fluid collections (POFCs), pancreatic pseudocysts (PPs), or walled-off pancreatic necrosis (WOPN). Clinical success was defined as a decrease in PFC size by ≥50% of the maximal diameter or to ≤2 cm.
Results
A total of 108 patients (62% male; mean age, 53 years) were included: 13 had POFCs, 43 had PPs, and 52 had WOPN. Seventytwo patients (66%) required a pancreatic duct (PD) stent, whereas 65 (60%) received enteral feeding. A total of 103 (95%) patients achieved clinical success. Eight patients experienced complications including bleeding (n=6) and surgical intervention (n=2). Patients with enteral feeding were 3.4 times more likely to achieve resolution within 60 days (p=0.0421), whereas those with PD stenting was five times more likely to achieve resolution within 90 days (p=0.0069).
Conclusions
A high PFC resolution rate can be achieved when a dedicated algorithm encompassing EUS-guided drainage, PD stenting, and early enteral feeding is adopted.
Figure
Cited by 1 articles
-
Importance of Pancreatic Duct Stenting and Enteral Feeding in Treatment Algorithm of Pancreatic Fluid Collections
Seong-Hun Kim, Eun Ji Shin
Clin Endosc. 2020;53(3):253-254. doi: 10.5946/ce.2020.112.
Reference
-
1. Holt BA, Varadarajulu S. The endoscopic management of pancreatic pseudocysts (with videos). Gastrointest Endosc. 2015; 81:804–812.
Article2. ASGE Standards of Practice Committee, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of inflammatory pancreatic fluid collections. Gastrointest Endosc. 2016; 83:481–488.
Article3. Tyberg A, Karia K, Gabr M, et al. Management of pancreatic fluid collections: a comprehensive review of the literature. World J Gastroenterol. 2016; 22:2256–2270.
Article4. Bergman S, Melvin WS. Operative and nonoperative management of pancreatic pseudocysts. Surg Clin North Am. 2007; 87:1447–1460. ix.
Article5. Ge PS, Weizmann M, Watson RR. Pancreatic pseudocysts: advances in endoscopic management. Gastroenterol Clin North Am. 2016; 45:9–27.6. Aghdassi A, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD, Lerch MM. Diagnosis and treatment of pancreatic pseudocysts in chronic pancreatitis. Pancreas. 2008; 36:105–112.
Article7. Rana SS, Bhasin DK, Reddy YR, et al. Morphological features of fluid collections on endoscopic ultrasound in acute necrotizing pancreatitis: do they change over time? Ann Gastroenterol. 2014; 27:258–261.8. Fisher JM, Gardner TB. Endoscopic therapy of necrotizing pancreatitis and pseudocysts. Gastrointest Endosc Clin N Am. 2013; 23:787–802.
Article9. Aghdassi AA, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD, Lerch MM. Pancreatic pseudocysts--when and how to treat? HPB (Oxford). 2006; 8:432–441.10. Varadarajulu S, Bang JY, Phadnis MA, Christein JD, Wilcox CM. Endoscopic transmural drainage of peripancreatic fluid collections: outcomes and predictors of treatment success in 211 consecutive patients. J Gastrointest Surg. 2011; 15:2080–2088.
Article11. Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology. 2013; 145:583–590.e1.
Article12. van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011; 141:1254–1263.
Article13. Warshaw AL, Rattner DW. Timing of surgical drainage for pancreatic pseudocyst. Clinical and chemical criteria. Ann Surg. 1985; 202:720–724.14. Neoptolemos JP, London NJ, Carr-Locke DL. Assessment of main pancreatic duct integrity by endoscopic retrograde pancreatography in patients with acute pancreatitis. Br J Surg. 1993; 80:94–99.
Article15. Howard TJ, Moore SA, Saxena R, Matthews DE, Schmidt CM, Wiebke EA. Pancreatic duct strictures are a common cause of recurrent pancreatitis after successful management of pancreatic necrosis. Surgery. 2004; 136:909–916.
Article16. Nealon WH, Bhutani M, Riall TS, Raju G, Ozkan O, Neilan R. A unifying concept: pancreatic ductal anatomy both predicts and determines the major complications resulting from pancreatitis. J Am Coll Surg. 2009; 208:790–799. discussion 799-801.
Article17. Trevino JM, Tamhane A, Varadarajulu S. Successful stenting in ductal disruption favorably impacts treatment outcomes in patients undergoing transmural drainage of peripancreatic fluid collections. J Gastroenterol Hepatol. 2010; 25:526–531.
Article18. Lau ST, Simchuk EJ, Kozarek RA, Traverso LW. A pancreatic ductal leak should be sought to direct treatment in patients with acute pancreatitis. Am J Surg. 2001; 181:411–415.
Article19. Iso Y, Kubota K. Intragastric stapled pancreatic pseudocystgastrostomy under endoscopic guidance. Surg Laparosc Endosc Percutan Tech. 2013; 23:330–333.
Article20. Makola D, Krenitsky J, Parrish C, et al. Efficacy of enteral nutrition for the treatment of pancreatitis using standard enteral formula. Am J Gastroenterol. 2006; 101:2347–2355.
Article21. Li JY, Yu T, Chen GC, et al. Enteral nutrition within 48 hours of admission improves clinical outcomes of acute pancreatitis by reducing complications: a meta-analysis. PLoS One. 2013; 8:e64926.
Article22. Chang YS, Fu HQ, Xiao YM, Liu JC. Nasogastric or nasojejunal feeding in predicted severe acute pancreatitis: a meta-analysis. Crit Care. 2013; 17:R118.
Article23. Al-Omran M, Albalawi ZH, Tashkandi MF, Al-Ansary LA. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010; CD002837.
Article24. Penn DE, Draganov PV, Wagh MS, Forsmark CE, Gupte AR, Chauhan SS. Prospective evaluation of the use of fully covered self-expanding metal stents for EUS-guided transmural drainage of pancreatic pseudocysts. Gastrointest Endosc. 2012; 76:679–684.
Article25. Bang JY, Varadarajulu S. Endoscopic ultrasound-guided management of pancreatic pseudocysts and walled-off necrosis. Clin Endosc. 2014; 47:429–431.
Article26. Antillon MR, Shah RJ, Stiegmann G, Chen YK. Single-step EUS-guided transmural drainage of simple and complicated pancreatic pseudocysts. Gastrointest Endosc. 2006; 63:797–803.
Article27. Park DH, Lee SS, Moon SH, et al. Endoscopic ultrasound-guided versus conventional transmural drainage for pancreatic pseudocysts: a prospective randomized trial. Endoscopy. 2009; 41:842–848.
Article28. Kahaleh M, Shami VM, Conaway MR, et al. Endoscopic ultrasound drainage of pancreatic pseudocyst: a prospective comparison with conventional endoscopic drainage. Endoscopy. 2006; 38:355–359.
Article29. Varadarajulu S, Christein JD, Tamhane A, Drelichman ER, Wilcox CM. Prospective randomized trial comparing EUS and EGD for transmural drainage of pancreatic pseudocysts (with videos). Gastrointest Endosc. 2008; 68:1102–1111.
Article30. Bang JY, Hawes R, Bartolucci A, Varadarajulu S. Efficacy of metal and plastic stents for transmural drainage of pancreatic fluid collections: a systematic review. Dig Endosc. 2015; 27:486–498.31. Baron TH, Thaggard WG, Morgan DE, Stanley RJ. Endoscopic therapy for organized pancreatic necrosis. Gastroenterology. 1996; 111:755–764.
Article32. Seewald S, Groth S, Omar S, et al. Aggressive endoscopic therapy for pancreatic necrosis and pancreatic abscess: a new safe and effective treatment algorithm (videos). Gastrointest Endosc. 2005; 62:92–100.
Article33. Voermans RP, Besselink MG, Fockens P. Endoscopic management of walled-off pancreatic necrosis. J Hepatobiliary Pancreat Sci. 2015; 22:20–26.
Article34. Seifert H, Biermer M, Schmitt W, et al. Transluminal endoscopic necrosectomy after acute pancreatitis: a multicentre study with long-term follow-up (the GEPARD Study). Gut. 2009; 58:1260–1266.
Article35. Walter D, Will U, Sanchez-Yague A, et al. A novel lumen-apposing metal stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: a prospective cohort study. Endoscopy. 2015; 47:63–67.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-Guided Management of Pancreatic Pseudocysts and Walled-Off Necrosis
- Endoscopic Management of Pancreatic Fluid Collections in Children
- Endoscopic Management of Peri-Pancreatic Fluid Collections
- Endoscopic Ultrasound-Guided Drainage of Pancreatic Fluid Collections (with Video)
- The role of endoscopic therapy in the minimally invasive management of pancreatic necrosis