Clin Endosc.
2020 May;53(3):328-333. 10.5946/ce.2019.133.
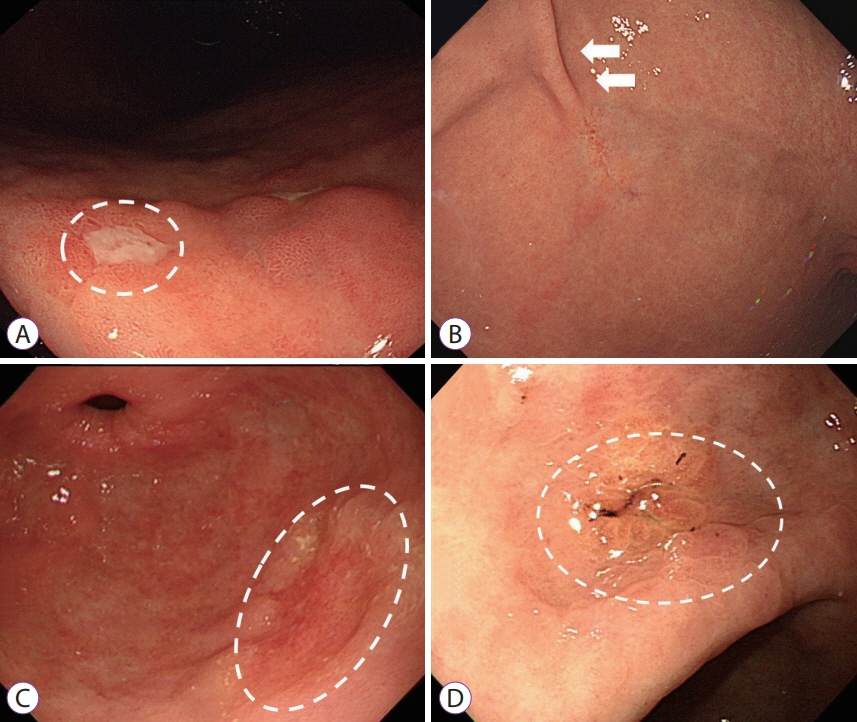
Endoscopic Factors that Can Predict Histological Ulcerations in Early Gastric Cancers
- Affiliations
-
- 1Department of Internal Medicine, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 2Department of Pathology, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- KMID: 2502767
- DOI: http://doi.org/10.5946/ce.2019.133
Abstract
- Background/Aims
Predicting histological ulceration in early gastric cancer (EGC) during endoscopic examination is crucial for endoscopists deciding on the treatment modality. The aim of this study was to investigate the endoscopic factors that can predict histological ulcerations in EGCs.
Methods
We retrospectively analyzed patients who underwent endoscopic submucosal dissection (ESD) for EGC. Clinical features and endoscopic characteristics of EGC such as location, histological differentiation, longest diameter, tumor morphology, mucosal break, converging fold, color change, and surface irregularity were reviewed. Histological ulceration was defined based on ESD specimens.
Results
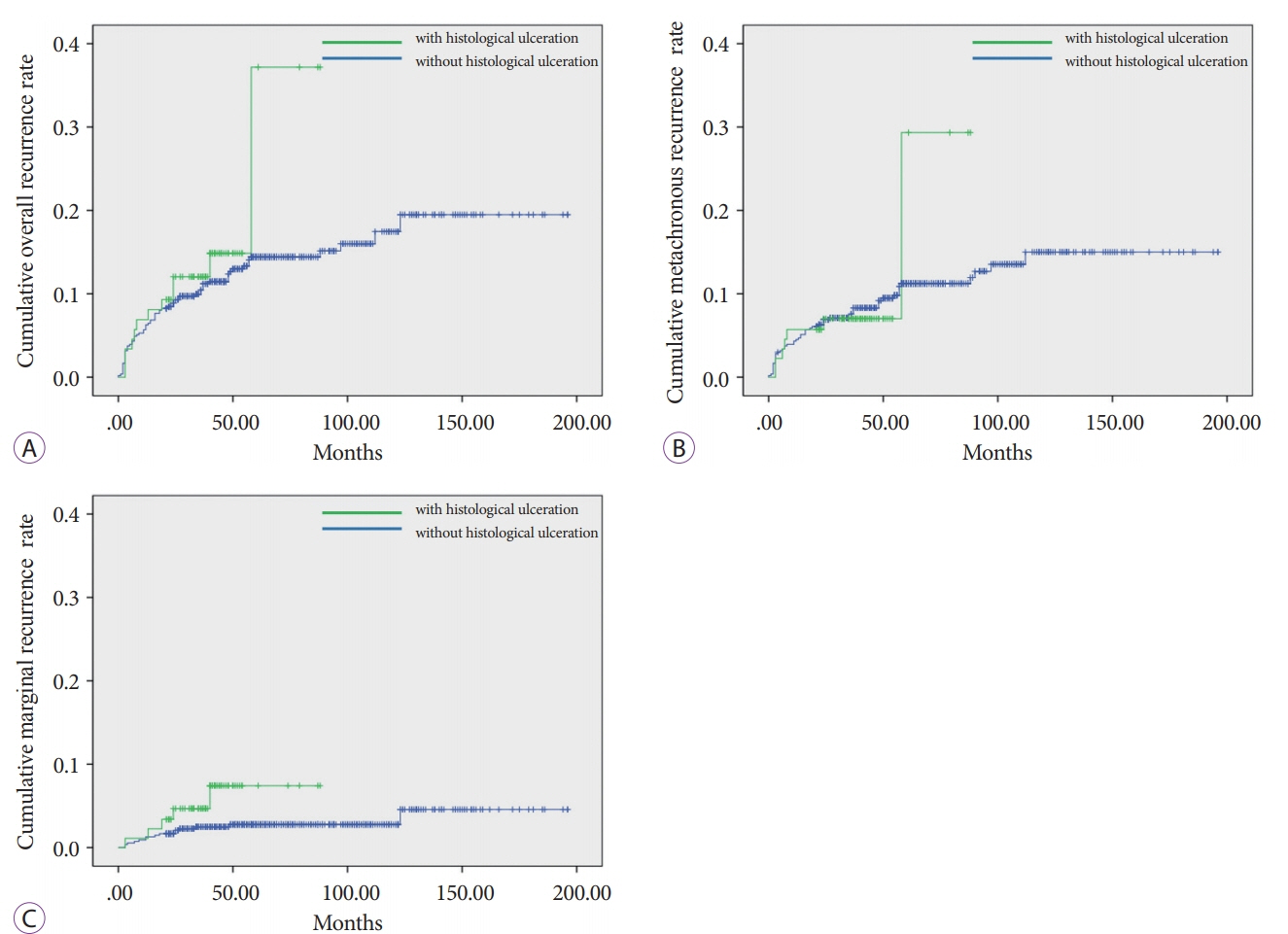
A total of 633 EGC lesions from 613 patients were included and histological ulcerations were found in 90 lesions (14.2%). Presence of converging folds, tumor morphology, and color changes on endoscopic examination were related to histological ulceration in the univariate analysis and converging folds along with color changes were statistically significant factors in the multivariate analysis. Kaplan–Meier analysis showed that patients with histological ulcerations in EGCs tended to have higher marginal recurrence rates.
Conclusions
Mucosal breaks are not equivalent to histological ulcerations. Rather, the existence of converging folds and color changes during endoscopic examination suggest histological ulcerations. Endoscopists should consider these factors when they decide the treatment modality for EGCs.
Figure
Cited by 1 articles
-
What is the Most Precise Endoscopic Finding for Predicting the Clinicopathological Behaviors in Ulcerative Early Gastric Cancer?
Youngdae Kim
Clin Endosc. 2020;53(3):249-250. doi: 10.5946/ce.2020.107.
Reference
-
1. Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009; 69:1228–1235.
Article2. Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000; 3:219–225.
Article3. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines. 5th ed. Tokyo: Kanehara-Shuppan;2018.4. Lee JH, Kim JG, Jung HK, et al. Clinical practice guidelines for gastric cancer in Korea: an evidence-based approach. J Gastric Cancer. 2014; 14:87–104.
Article5. Park SM, Kim BW, Kim JS, Kim YW, Kim GJ, Ryu SJ. Can endoscopic ulcerations in early gastric cancer be clearly defined before endoscopic resection? A survey among endoscopists. Clin Endosc. 2017; 50:473–478.
Article6. Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000; 47:251–255.
Article7. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.8. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003; 58(6 Suppl):S3–S43.9. Kwee RM, Kwee TC. Predicting lymph node status in early gastric cancer. Gastric Cancer. 2008; 11:134–148.
Article10. Park JS, Kim H, Bang B, Kwon K, Shin Y. Accuracy of endoscopic ultrasonography for diagnosing ulcerative early gastric cancers. Medicine (Baltimore). 2016; 95:e3955.
Article11. Akashi K, Yanai H, Nishikawa J, et al. Ulcerous change decreases the accuracy of endoscopic ultrasonography diagnosis for the invasive depth of early gastric cancer. Int J Gastrointest Cancer. 2006; 37:133–138.
Article12. Sakita T, Oguro Y, Takasu S, Fukutomi H, Miwa T. Observations on the healing of ulcerations in early gastric cancer. The life cycle of the malignant ulcer. Gastroenterology. 1971; 60:835–839 passim.13. Lee JI, Kim JH, Kim JH, et al. Indication for endoscopic treatment of ulcerative early gastric cancer according to depth of ulcer and morphological change. J Gastroenterol Hepatol. 2012; 27:1718–1725.
Article14. Honmyo U, Misumi A, Murakami A, et al. Mechanisms producing color change in flat early gastric cancers. Endoscopy. 1997; 29:366–371.
Article15. Yao K, Yao T, Matsui T, Iwashita A, Oishi T. Hemoglobin content in intramucosal gastric carcinoma as a marker of histologic differentiation: a clinical application of quantitative electronic endoscopy. Gastrointest Endosc. 2000; 52:241–245.
Article16. Lee HH, Lee SY, Yoon HY, et al. Change of mucosal color in early gastric cancer. J Dig Dis. 2012; 13:510–516.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Systematic Endoscopic Approach to Early Gastric Cancer in Clinical Practice
- Endoscopic diagnosis of early gastric cancer
- Can Endoscopic Ulcerations in Early Gastric Cancer Be Clearly Defined before Endoscopic Resection? A Survey among Endoscopists
- Endoscopic treatment for early gastric cancer
- Discrepancy between Clinical and Final Pathological Evaluation Findings in Early Gastric Cancer Patients Treated with Endoscopic Submucosal Dissection