Arch Hand Microsurg.
2020 Jun;25(2):77-89. 10.12790/ahm.20.0013.
Scapholunate Dissociation: Current Concepts of the Treatments
- Affiliations
-
- 1Department of Orthopaedic Surgery, Daegu Catholic University Medical Center, Daegu Catholic University School of Medicine, Daegu, Korea
- 2Department of Orthopaedic Surgery, H Plus Yangji Hospital, Seoul, Korea
- 3Department of Orthopaedic Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2502703
- DOI: http://doi.org/10.12790/ahm.20.0013
Abstract
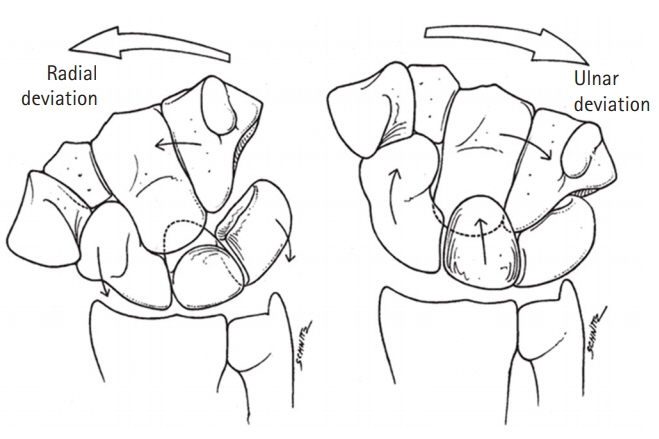
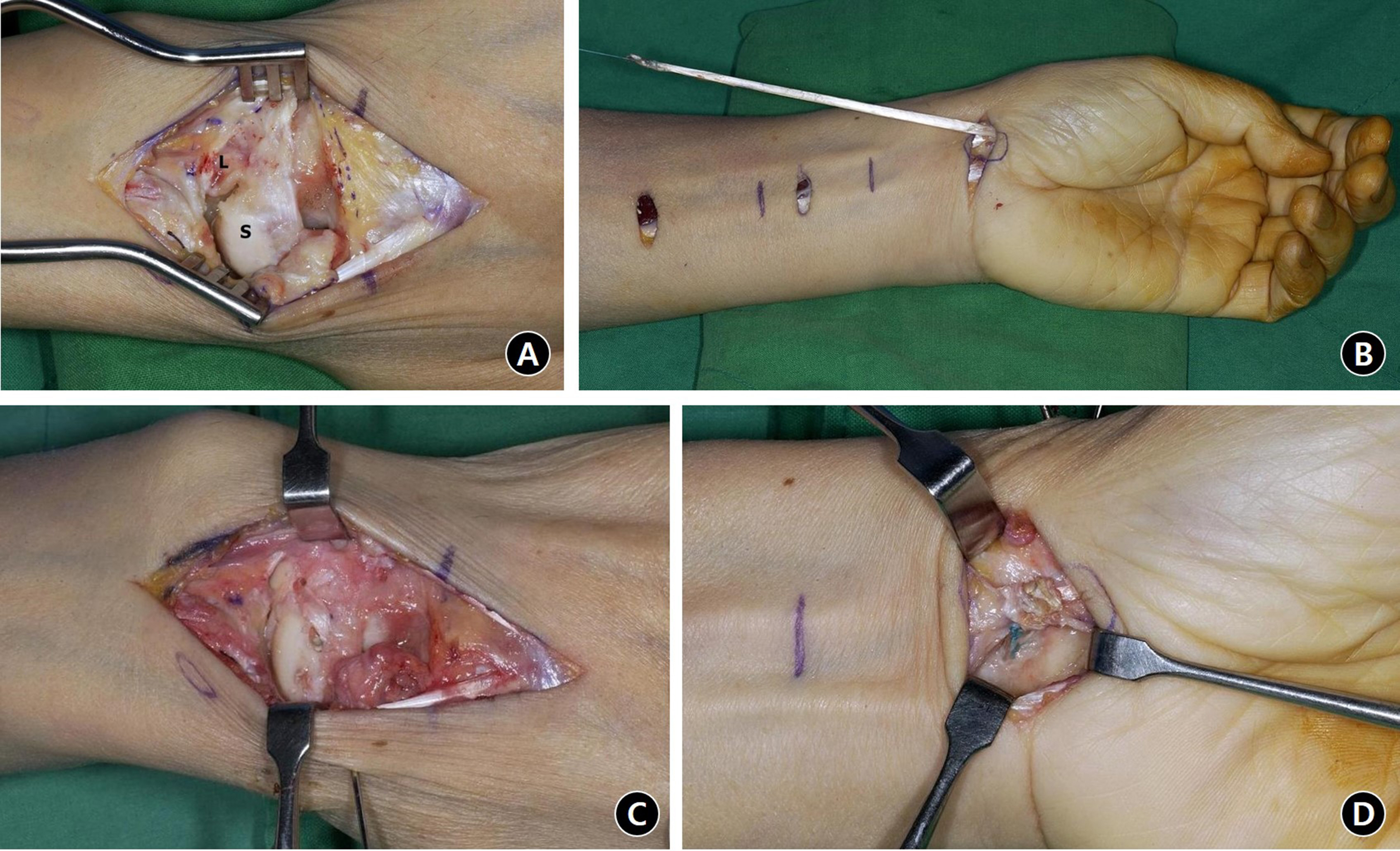
- Scapholunate dissociation is the most common cause of the wrist pain and instability and typically results from scapholunate interosseous ligament (SLIL) injury. It is difficult for surgeons to diagnose the SLIL injury due to its complex anatomy and biomechanics. The natural history of the SLIL injury is still not fully understood as most of the SLIL injuries are not detected in their acute stage. Careful physical examination and radiologic evaluation are essential aspects of SLIL injury diagnosis. We should consider five conditions to evaluate SLIL injuries: the integrity of the dorsal SLIL, the healing potential of the disrupted ligament, the alignment of the scaphoid, the reducibility of the carpal malalignment, and the cartilage condition. In this review, the stages classified based on these conditions and the current treatments according to each stage will be described in detail.
Figure
Reference
-
1. Destot E. The classic: injuries of the wrist: a radiological study. New York, NY: Paul B. Hoeber; 1926. Clin Orthop Relat Res. 2006; 445:8–14.2. Linscheid RL, Dobyns JH, Beabout JW, Bryan RS. Traumatic instability of the wrist: diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 1972; 54:1612–32.3. Berger RA, Imeada T, Berglund L, An KN. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg Am. 1999; 24:953–62.
Article4. Andersson JK. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev. 2017; 2:382–93.5. Cassidy C, Ruby LK. Carpal instability. Instr Course Lect. 2003; 52:209–20.6. Kamal RN, Starr A, Akelman E. Carpal kinematics and kinetics. J Hand Surg Am. 2016; 41:1011–8.
Article7. Park M. Hand & upper extremity surgery: the wrist & elbow. Seoul: PanMun Education;2017.8. Walsh JJ, Berger RA, Cooney WP. Current status of scapholunate interosseous ligament injuries. J Am Acad Orthop Surg. 2002; 10:32–42.
Article9. Wolfe SW. Scapholunate instability. J Am Soc Surg of Hand. 2001; 1:45–60.
Article10. Manuel J, Moran SL. The diagnosis and treatment of scapholunate instability. Hand Clin. 2010; 26:129–44.
Article11. Mayfield JK. Mechanism of carpal injuries. Clin Orthop Relat Res. 1980; 45–54.
Article12. Watson HK, Weinzweig J, Zeppieri J. The natural progression of scaphoid instability. Hand Clin. 1997; 13:39–49.
Article13. Lee YK, Kang HV, Jung YR, Lee JY. Surgical treatment of scapholunate instability. Arch Hand Microsurg. 2018; 23:139–49.
Article14. Sebald JR, Dobyns JH, Linscheid RL. The natural history of collapse deformities of the wrist. Clin Orthop Relat Res. 1974; (104):140–8.
Article15. Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980; 5:226–41.
Article16. Harrington RH, Lichtman DM, Brockmole DM. Common pathways of degenerative arthritis of the wrist. Hand Clin. 1987; 3:507–27.
Article17. Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2008; 33:998–1013.
Article18. Greditzer HGt, Zeidenberg J, Kam CC, et al. Optimal detection of scapholunate ligament tears with MRI. Acta Radiol. 2016; 57:1508–14.
Article19. Meister DW, Hearns KA, Carlson MG. Dorsal scaphoid subluxation on sagittal magnetic resonance imaging as a marker for scapholunate ligament tear. J Hand Surg Am. 2017; 42:717–21.
Article20. Lindau TR. The role of arthroscopy in carpal instability. J Hand Surg Eur Vol. 2016; 41:35–47.
Article21. Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996; 78:357–65.
Article22. Messina JC, Van Overstraeten L, Luchetti R, Fairplay T, Mathoulin CL. The EWAS classification of scapholunate tears: an anatomical arthroscopic study. J Wrist Surg. 2013; 2:105–9.23. Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006; 31:125–34.
Article24. O'Meeghan CJ, Stuart W, Mamo V, Stanley JK, Trail IA. The natural history of an untreated isolated scapholunate interosseus ligament injury. J Hand Surg Br. 2003; 28:307–10.25. Slutsky DJ, Nagle DJ. Wrist arthroscopy: current concepts. J Hand Surg Am. 2008; 33:1228–44.
Article26. Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg Am. 1996; 21:412–7.
Article27. Darlis NA, Weiser RW, Sotereanos DG. Partial scapholunate ligament injuries treated with arthroscopic debridement and thermal shrinkage. J Hand Surg Am. 2005; 30:908–14.
Article28. Dobyns JH, Linscheid RL. A short history of the wrist joint. Hand Clin. 1997; 13:1–12.
Article29. Minami A, Kato H, Iwasaki N. Treatment of scapholunate dissociation: ligamentous repair associated with modified dorsal capsulodesis. Hand Surg. 2003; 8:1–6.
Article30. Pomerance J. Outcome after repair of the scapholunate interosseous ligament and dorsal capsulodesis for dynamic scapholunate instability due to trauma. J Hand Surg Am. 2006; 31:1380–6.
Article31. Garcia-Elias M, Pitagoras T, Gilabert-Senar A. Relationship between joint laxity and radio-ulno-carpal joint morphology. J Hand Surg Br. 2003; 28:158–62.
Article32. Soong M, Merrell GA, Ortmann Ft, Weiss AP. Long-term results of bone-retinaculum-bone autograft for scapholunate instability. J Hand Surg Am. 2013; 38:504–8.
Article33. Weiss AP. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft. J Hand Surg Am. 1998; 23:205–15.
Article34. Harvey EJ, Berger RA, Osterman AL, Fernandez DL, Weiss AP. Bone-tissue-bone repairs for scapholunate dissociation. J Hand Surg Am. 2007; 32:256–64.
Article35. Deshmukh SC, Givissis P, Belloso D, Stanley JK, Trail IA. Blatt's capsulodesis for chronic scapholunate dissociation. J Hand Surg Br. 1999; 24:215–20.
Article36. Slater RR Jr, Szabo RM, Bay BK, Laubach J. Dorsal intercarpal ligament capsulodesis for scapholunate dissociation: biomechanical analysis in a cadaver model. J Hand Surg Am. 1999; 24:232–9.
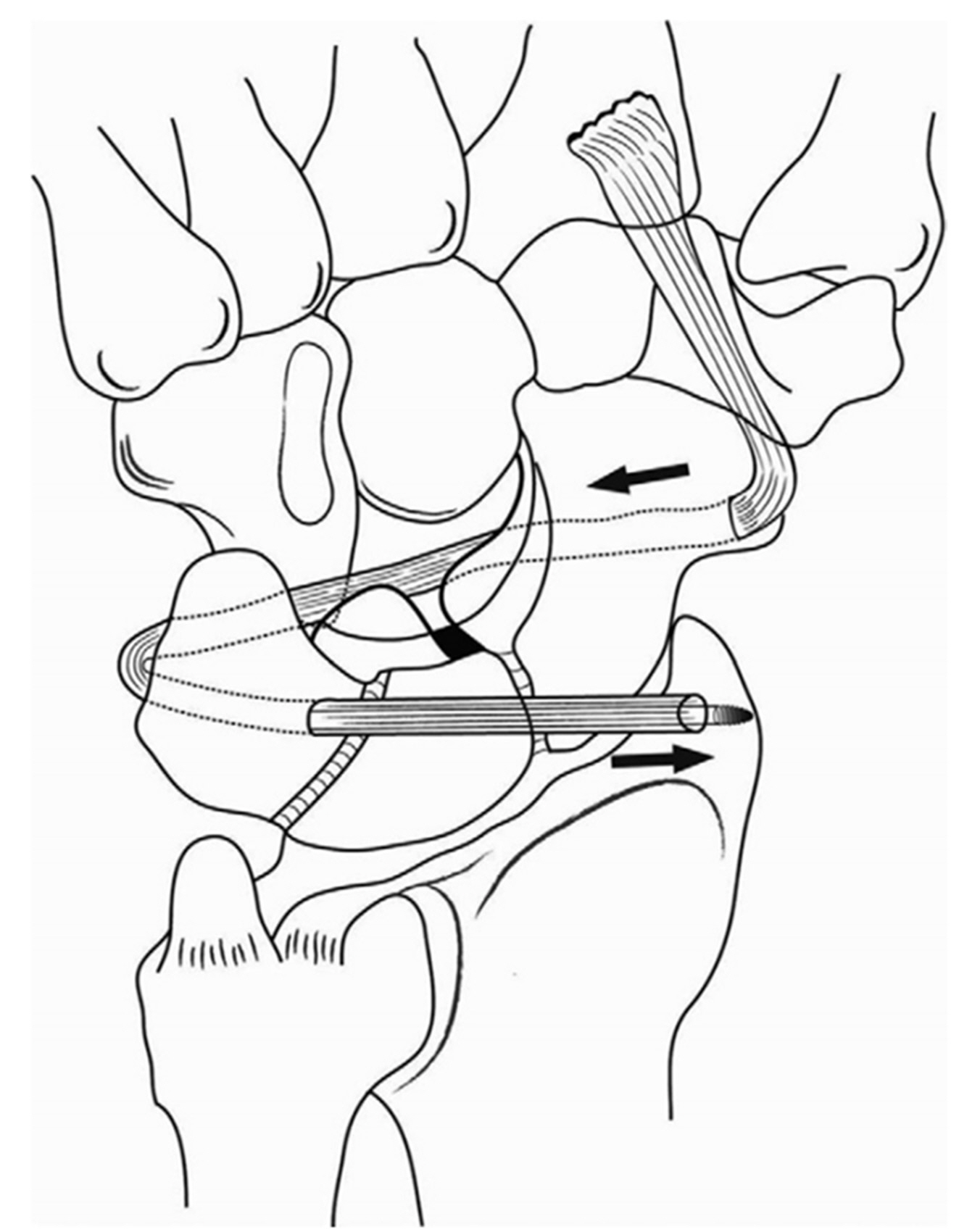
Article37. Brunelli GA, Brunelli GR. A new surgical technique for carpal instability with scapholunate dissociation. Surg Technol Int. 1996; 5:370–4.38. Van Den Abbeele KL, Loh YC, Stanley JK, Trail IA. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg Br. 1998; 23:258–61.
Article39. Short WH, Werner FW, Sutton LG. Dynamic biomechanical evaluation of the dorsal intercarpal ligament repair for scapholunate instability. J Hand Surg Am. 2009; 34:652–9.
Article40. Dobyns JH, Linscheid RL, EY C. Traumatic instability of the wrist. Instr Course Lect. 1975; 24:182–99.41. Henry M. Reconstruction of both volar and dorsal limbs of the scapholunate interosseous ligament. J Hand Surg Am. 2013; 38:1625–34.
Article42. Corella F, Del Cerro M, Ocampos M, Simon de Blas C, Larrainzar-Garijo R. Arthroscopic scapholunate ligament reconstruction, volar and dorsal reconstruction. Hand Clin. 2017; 33:687–707.
Article43. Chee KG, Chin AY, Chew EM, Garcia-Elias M. Antipronation spiral tenodesis: a surgical technique for the treatment of perilunate instability. J Hand Surg Am. 2012; 37:2611–8.44. Mullikin I, Srinivasan RC, Bagg M. Current techniques in scapholunate ligament reconstruction. Orthop Clin North Am. 2020; 51:77–86.
Article45. Rosenwasser MP, Paul SB, Froimson AI. Arthroplasty of the hand and wrist. Hand Clin. 1989; 5:487–505.
Article46. Watson HK, Goodman ML, Johnson TR. Limited wrist arthrodesis. Part II: intercarpal and radiocarpal combinations. J Hand Surg Am. 1981; 6:223–33.
Article47. Matheson LN, Melhorn JM, Mayer TG, Theodore BR, Gatchel RJ. Reliability of a visual analog version of the QuickDASH. J Bone Joint Surg Am. 2006; 88:1782–7.
Article48. Stewart DT, Froelich JM, Shin AY. Intercarpal arthrodeses. J Hand Surg Am. 2014; 39:373–7.
Article49. Garcia-Elias M, Lluch A, Ferreres A, Papini-Zorli I, Rahimtoola ZO. Treatment of radiocarpal degenerative osteoarthritis by radioscapholunate arthrodesis and distal scaphoidectomy. J Hand Surg Am. 2005; 30:8–15.
Article50. Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984; 9:358–65.
Article51. Berkhout MJ, Bachour Y, Zheng KH, Mullender MG, Strackee SD, Ritt MJ. Four-corner arthrodesis versus proximal row carpectomy: a retrospective study with a mean follow-up of 17 years. J Hand Surg Am. 2015; 40:1349–54.
Article52. Green DP, Perreira AC, Longhofer LK. Proximal row carpectomy. J Hand Surg Am. 2015; 40:1672–6.
Article53. Trail IA, Murali R, Stanley JK, et al. The long-term outcome of four-corner fusion. J Wrist Surg. 2015; 4:128–33.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scapholunate Dissociation Associated with Distal Radius Fracture
- Scapholunate Dissociation Associated with Intra-articular Fractures of Distal Radius
- Radial styloid process fractures associated with scapholunate dissociation
- Volar Perilunate Dislocation: A case report
- Depression as a Mediator of the Relationship Between Resilience and Posttraumatic Stress Symptoms and Dissociation in Firefighters