Korean J Orthod.
2020 May;50(3):206-215. 10.4041/kjod.2020.50.3.206.
Surgical approach and orthodontic treatment of mandibular condylar osteochondroma
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Jeonbuk National University, Jeonju, Korea
- 2Institute of Oral Biosciences, School of Dentistry, Jeonbuk National University, Jeonju, Korea
- 3Research Institute of Clinical Medicine of Jeonbuk National University- Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2502630
- DOI: http://doi.org/10.4041/kjod.2020.50.3.206
Abstract
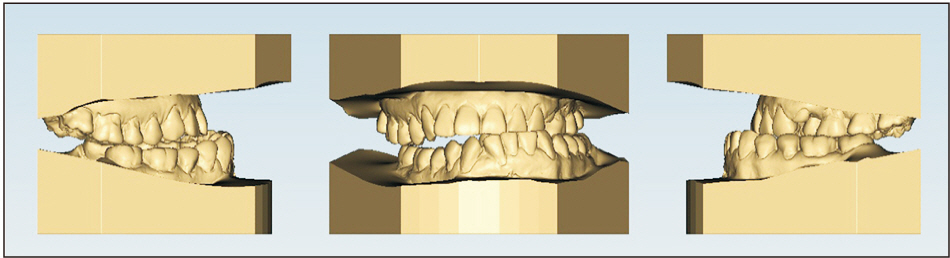
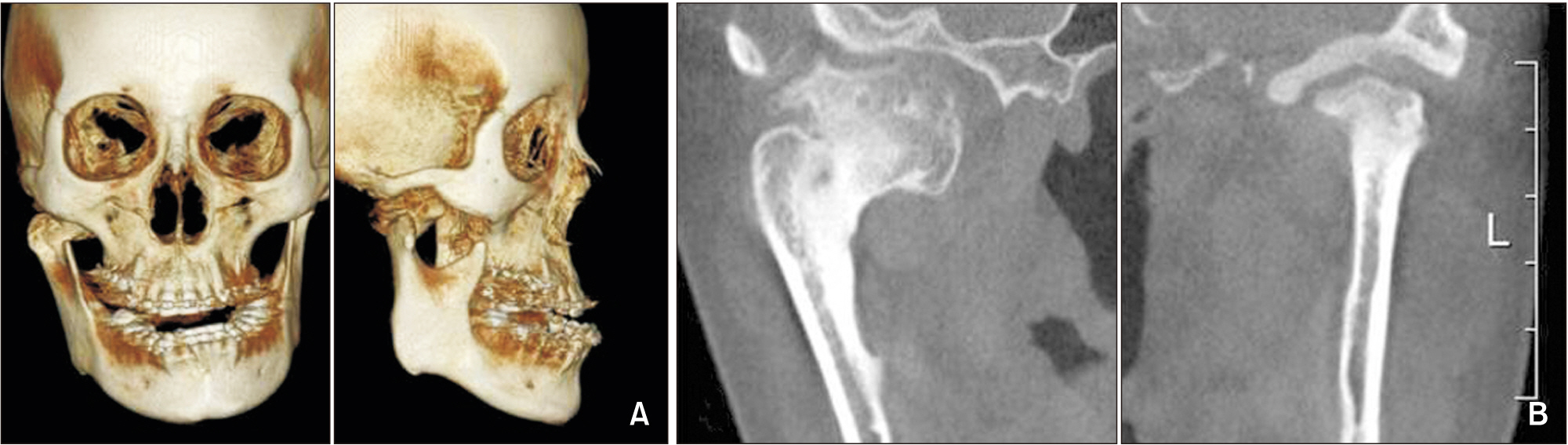
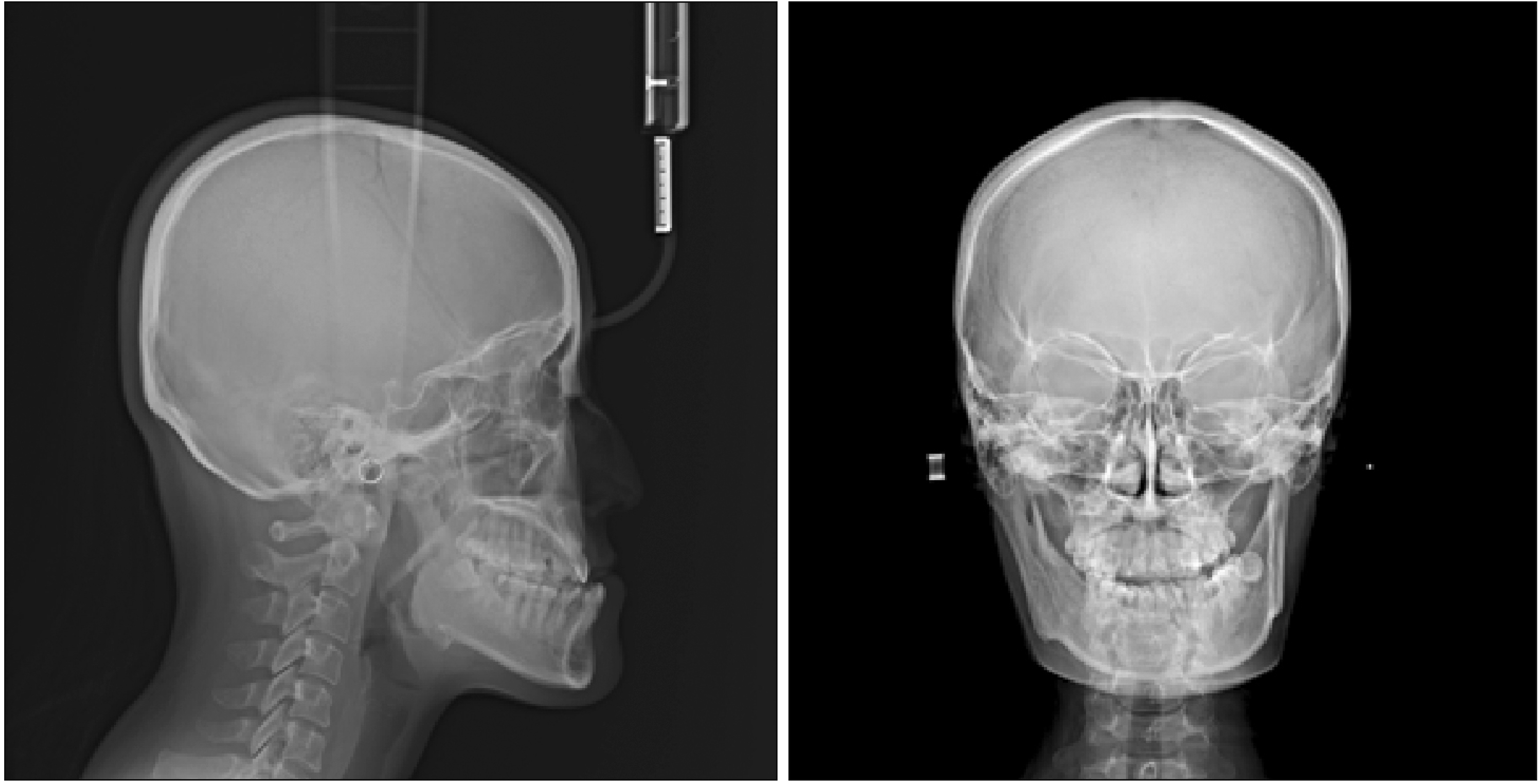
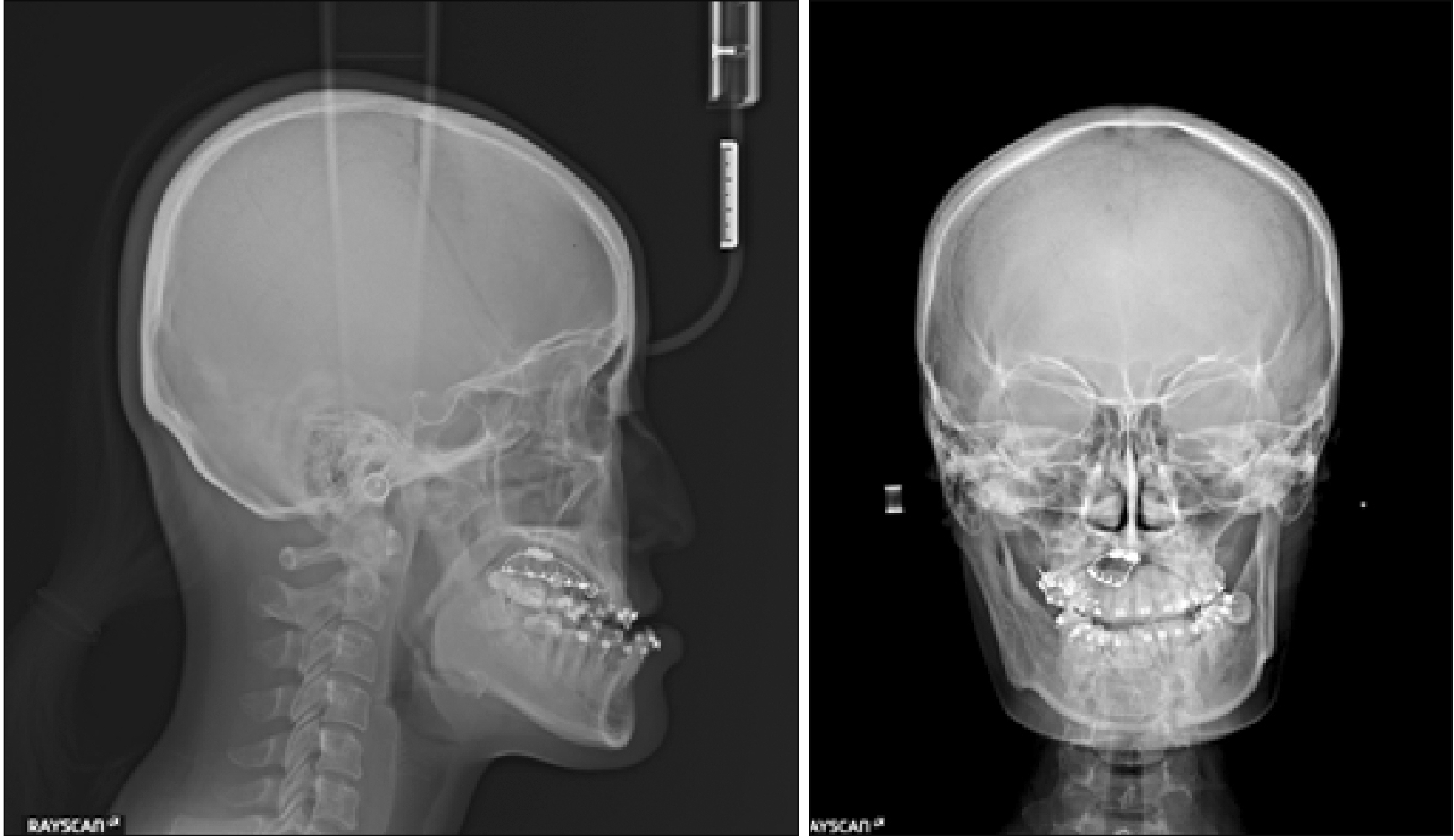
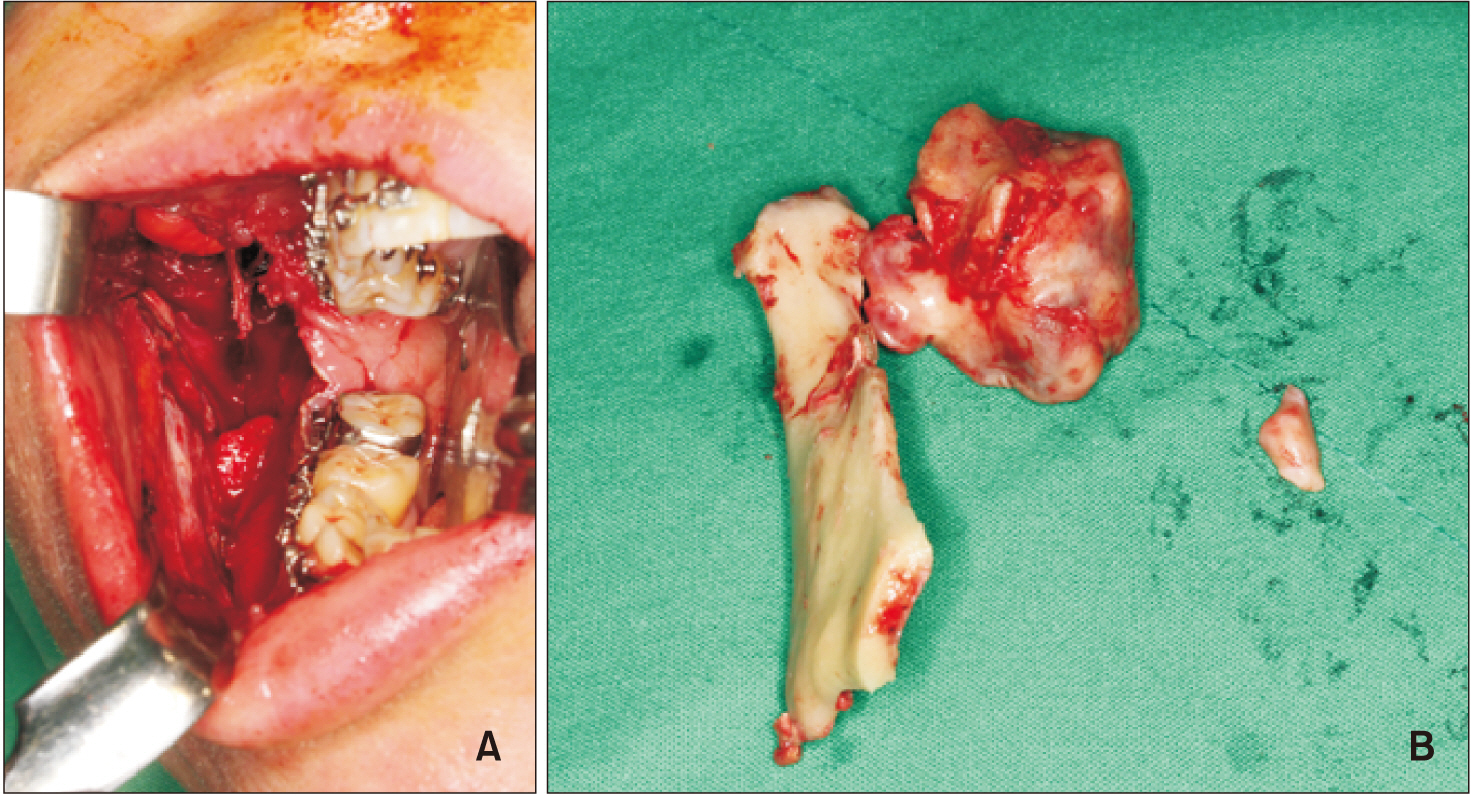
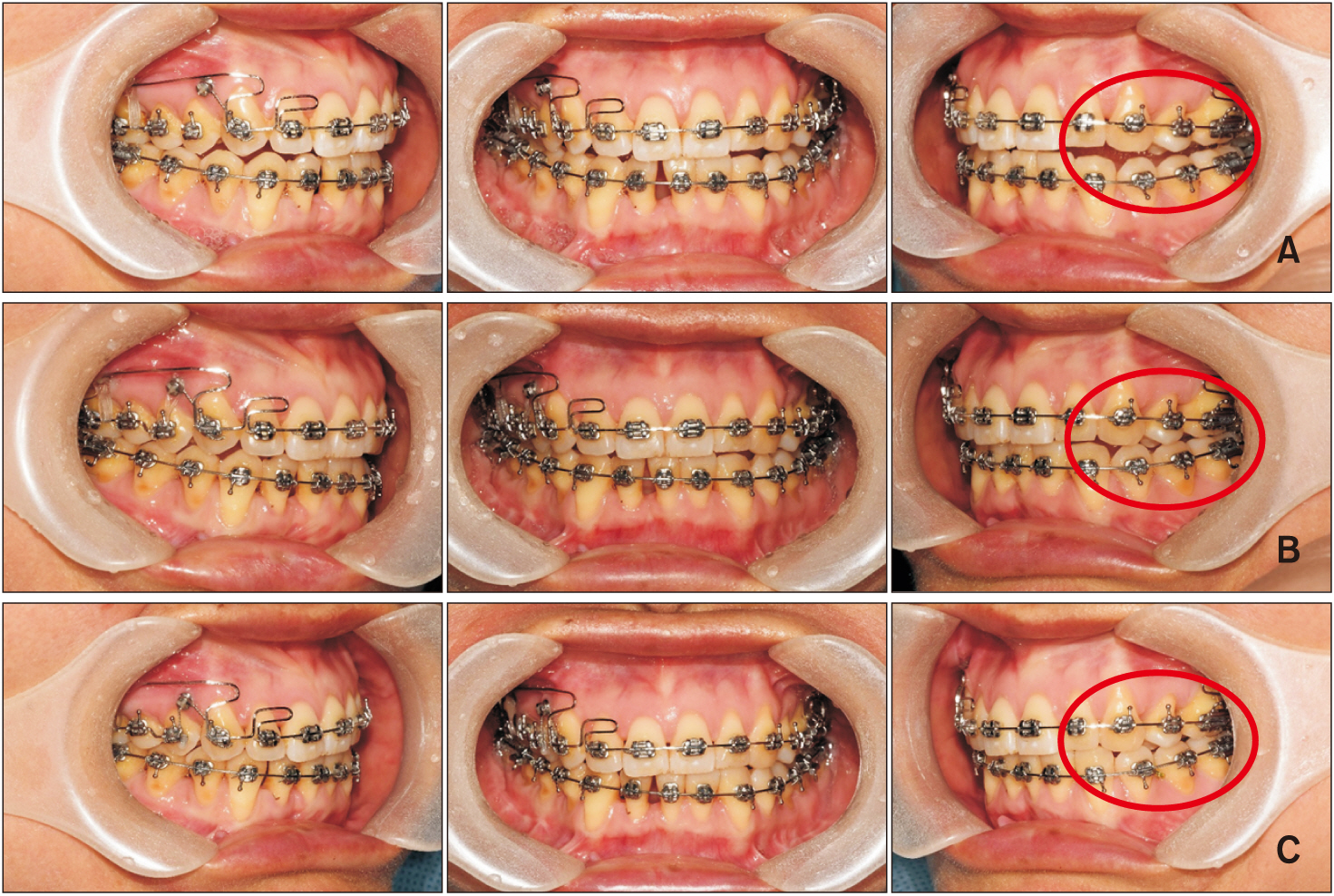
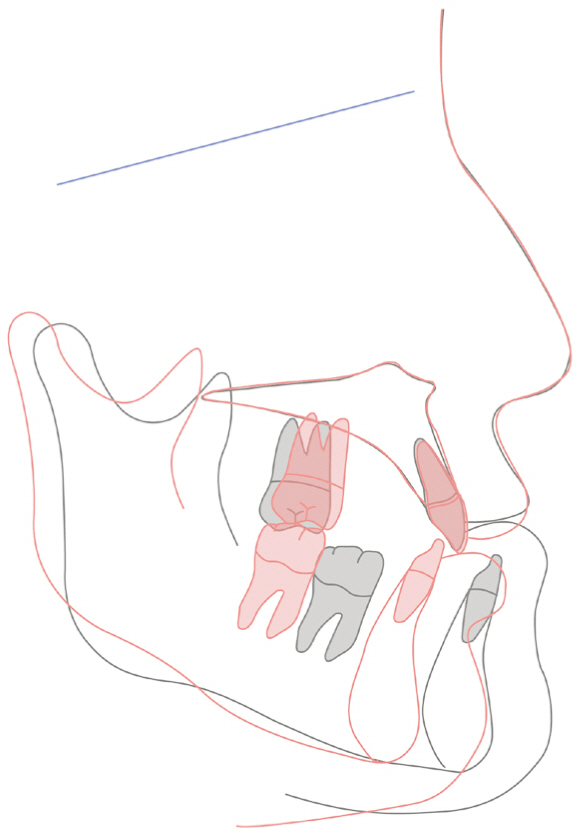
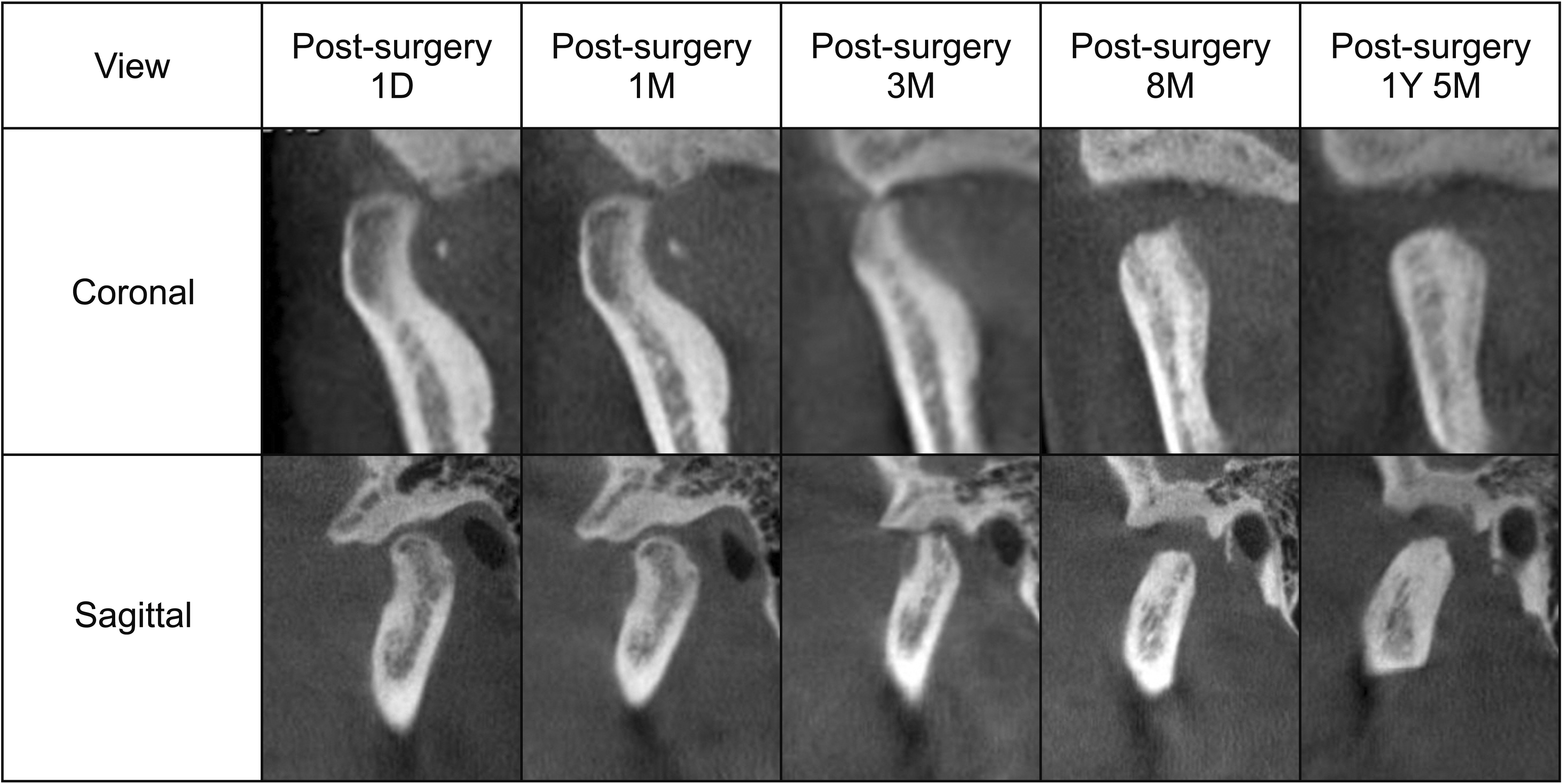
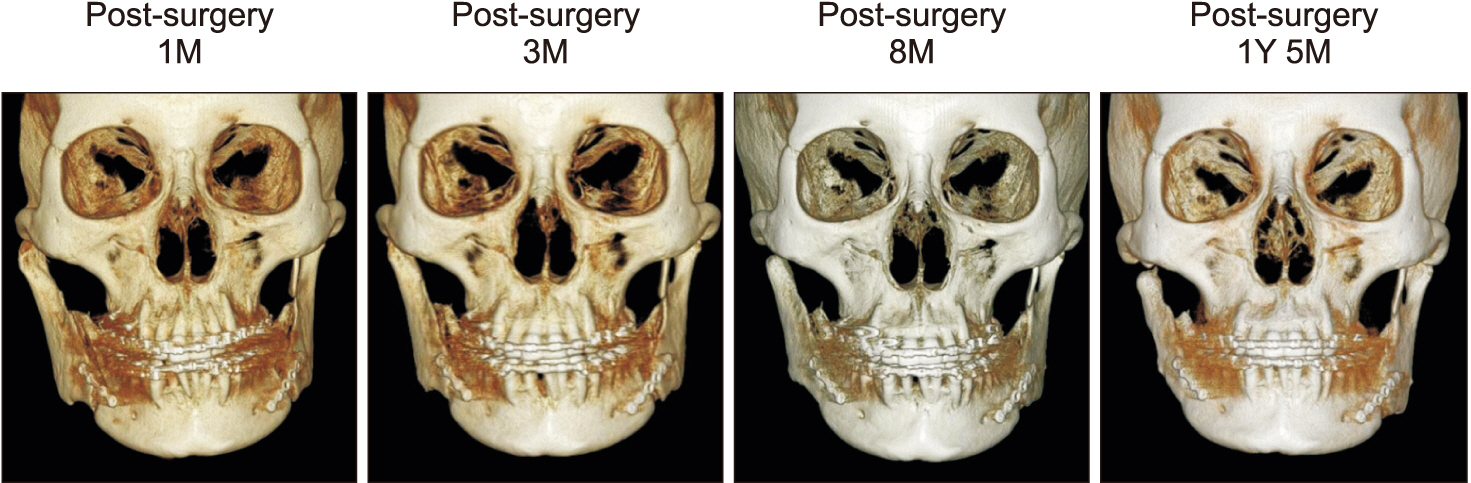
- Osteochondroma is a common benign tumor of bones, but it is rare in the mandibular condyle. With its outgrowth it manifests clinically as deviation of the mandible limitation of mouth opening, and facial asymmetry. After the tumor is diagnosed on the basis of clinical symptoms and radiographic examination including cone-beam computed tomography (CBCT) analysis, an appropriate surgery and treatment plan should be formulated. Herein, we present the case of a 44-year-old female patient who visited our dental hospital because her chin point had been deviating to the left side slowly but progressively over the last 3 years and she had difficulty masticating. Based on CBCT, she was diagnosed with skeletal Class III malocclusion accompanied by osteochondroma of the right mandibular condyle. Maxillary occlusal cant with the right side down was observed, but it was confirmed to be an extrusion of the molars associated with dental compensation. Therefore, after intrusion of the right molars with the use of temporary anchorage devices, sagittal split ramus osteotomy was used to remove the tumor and perform orthognathic surgery simultaneously. During 6 months after the surgery, continuous bone resorption and remodeling were observed in the condyle of the affected side, which led to a change in occlusion. During the postoperative orthodontic treatment, intrusive force and buccal torque were applied to the molars on the affected side, and a proper buccal overjet was created. After 18 months, CBCT revealed that the rate of bone absorption was continuously reduced, bone corticalization appeared, and good occlusion and a satisfying facial profile were achieved.
Keyword
Figure
Reference
-
1. Meng Q, Chen S, Long X, Cheng Y, Deng M, Cai H. 2012; The clinical and radiographic characteristics of condylar osteochondroma. Oral Surg Oral Med Oral Pathol Oral Radiol. 114:e66–74. DOI: 10.1016/j.oooo.2012.01.016. PMID: 22727110.
Article2. Cimino R, Steenks MH, Michelotti A, Farella M, PierFrancesco N. 2003; Mandibular condyle osteochondroma. Review of the literature and report of a misdiagnosed case. J Orofac Pain. 17:254–61. PMID: 14520772.3. Ribas Mde O, Martins WD, de Sousa MH, Zanferrari FL, Lanzoni T. 2007; Osteochondroma of the mandibular condyle: literature review and report of a case. J Contemp Dent Pract. 8:52–9. DOI: 10.5005/jcdp-8-4-52. PMID: 17486187.4. Avinash KR, Rajagopal KV, Ramakrishnaiah RH, Carnelio S, Mahmood NS. 2007; Computed tomographic features of mandibular osteochondroma. Dentomaxillofac Radiol. 36:434–6. DOI: 10.1259/dmfr/54329867. PMID: 17881606.
Article5. Henry CH, Granite EL, Rafetto LK. 1992; Osteochondroma of the mandibular condyle: report of a case and review of the literature. J Oral Maxillofac Surg. 50:1102–8. DOI: 10.1016/0278-2391(92)90500-Y. PMID: 1527664.
Article6. Karras SC, Wolford LM, Cottrell DA. 1996; Concurrent osteochondroma of the mandibular condyle and ipsilateral cranial base resulting in temperomandibular joint ankylosis: report of a case and review of the literature. J Oral Maxillofac Surg. 54:640–6. DOI: 10.1016/S0278-2391(96)90652-7. PMID: 8632254.
Article7. Vezeau PJ, Fridrich KL, Vincent SD. 1995; Osteochondroma of the mandibular condyle: literature review and report of two atypical cases. J Oral Maxillofac Surg. 53:954–63. DOI: 10.1016/0278-2391(95)90293-7. PMID: 7629631.8. Forssell H, Happonen RP, Forssell K, Virolainen E. 1985; Osteochondroma of the mandibular condyle. Report of a case and review of the literature. Br J Oral Maxillofac Surg. 23:183–9. DOI: 10.1016/0266-4356(85)90088-9. PMID: 3159417.
Article9. Gaines RE Jr, Lee MB, Crocker DJ. 1992; Osteochondroma of the mandibular condyle: case report and review of the literature. J Oral Maxillofac Surg. 50:899–903. DOI: 10.1016/0278-2391(92)90287-A. PMID: 1634981.
Article10. Tanaka E, Shiota C, Sato M, Fujihara S, Kondoh T, Kuroda S. 2016; Unilateral mandibular condylar osteochondroma treated with ipsilateral condylectomy and contralateral ramus osteotomy. Am J Orthod Dentofacial Orthop. 149:740–50. DOI: 10.1016/j.ajodo.2015.05.035. PMID: 27131256.
Article11. Iizuka T, Schroth G, Laeng RH, Lädrach K. 1996; Osteochondroma of the mandibular condyle: report of a case. J Oral Maxillofac Surg. 54:495–501. DOI: 10.1016/S0278-2391(96)90127-5. PMID: 8600267.
Article12. Miyamoto H, Shigematsu H, Suzuki S, Sakashita H. 2004; Regeneration of mandibular condyle following unilateral condylectomy in canines. J Craniomaxillofac Surg. 32:296–302. DOI: 10.1016/j.jcms.2004.04.005. PMID: 15458671.
Article13. Olate S, Cantín M, Palmieri C, Alister JP, Muñoz M, de Moraes M. 2015; Mandibular condyle repair after partial condylectomy in patients with active condylar hyperplasia. Int J Morphol. 33:759–63. DOI: 10.4067/S0717-95022015000200054.
Article14. Koole R, Steenks MH, Witkamp TD, Slootweg PJ, Shaefer J. 1996; Osteochondroma of the mandibular condyle. A case report. Int J Oral Maxillofac Surg. 25:203–5. DOI: 10.1016/S0901-5027(96)80030-0. PMID: 8872224.15. Chen MJ, Yang C, Qiu YT, Zhou Q, Huang D, Shi HM. 2014; Osteochondroma of the mandibular condyle: a classification system based on computed tomographic appearances. J Craniofac Surg. 25:1703–6. DOI: 10.1097/SCS.0000000000000898. PMID: 25119412.16. Yang JY, Leem DH. 2012; Surgical treatment of osteochondroma on the mandibular condyle through intraoral approach: case report. J Korean Assoc Maxillofac Plast Reconstr Surg. 34:349–56.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Osteochondroma on the Mandibular Condyle through Intraoral Approach: Case Report
- Conservative condylectomy alone for the correction of mandibular asymmetry caused by osteochondroma of the mandibular condyle: a report of five cases
- Osteochonrdoma Of The Mandibular Condyle: A Case Report
- Surgical excision of osteochondroma on mandibular condyle via preauricular approach with zygomatic arch osteotomy
- The Osteochondroma of the Mandibular Condyle: report of a case