J Korean Med Sci.
2020 Jun;35(22):e165. 10.3346/jkms.2020.35.e165.
Urinary Angiotensinogen in addition to Imaging Classification in the Prediction of Renal Outcome in Autosomal Dominant Polycystic Kidney Disease
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea
- 2Hallym University Kidney Research Institute, Seoul, Korea
- 3Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 4Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea
- 5Truewords Dialysis Clinic, Incheon, Korea
- 6Department of Internal Medicine, Kangbuk Samsung Hospital, Seoul, Korea
- 7Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea
- 8Department of Internal Medicine, Busan Paik Hospital, Busan, Korea
- 9Preventive and Management Center, Inha University Hospital, Incheon, Korea
- KMID: 2502607
- DOI: http://doi.org/10.3346/jkms.2020.35.e165
Abstract
- Background
Intrarenal renin-angiotensin system (RAS) is known to play the major role in the development of hypertension and renal progression in autosomal dominant polycystic kidney disease (ADPKD). Urinary angiotensinogen to creatinine ratio (AGT/Cr) was suggested as a novel biomarker to reflect intrarenal RAS activity. This study was performed to evaluate urinary AGT/Cr as a predictive biomarker for renal function decline in addition to imaging classification in a prospective ADPKD cohort.
Methods
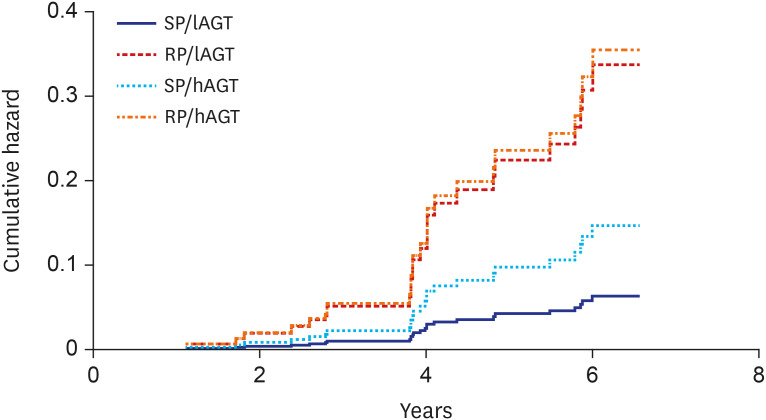
From 2011 to 2016, a total of 364 ADPKD patients were enrolled in the prospective cohort called the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD). Among them, a total of 207 subjects in chronic kidney disease stage 1–4 with baseline urinary AGT and total kidney volume and subsequent renal function follow-up data over more than 1 year were included in the analysis. Patients were defined as slow progressors (SP) if they are classified as 1A or 1B by imaging classification whereas rapid progressors (RP) if they are classified as 1C–1E. Patients were divided according to AGT/Cr quartiles and annual estimated glomerular filtration rate (eGFR) slope was compared among highest quartile (hAGT group) and the rest of quartiles (lAGT group). Patients were divided into 4 groups to evaluate the predictive value of urinary AGT/Cr in addition to imaging classification: SP/lAGT, SP/hAGT, RP/lAGT, and RP/hAGT. The Cox regression model was used to evaluate the hazard ratio (HR) between groups.
Results
The mean age was 45.9 years and 88.9% had hypertension. Baseline eGFR was 79.0 ± 28.4 mL/min/1.73 m2 and median height-adjusted total kidney volume was 788.2 (471.2;1,205.2) mL/m. The patients in the hAGT group showed lower eGFR (72.4 ± 24.8 vs. 81.1 ± 29.2 mL/min/1.73 m2, P = 0.039), lower plasma hemoglobin (13.0 ± 1.4 vs. 13.7 ± 1.6 g/dL, P = 0.007), higher urinary protein to creatinine ratio (0.14 [0.09, 0.38] vs. 0.07 [0.04, 0.12] g/g, P = 0.007) compared to the lAGT group. The hAGT group was an independent risk factor for faster eGFR decline after adjusting for gender, RP, baseline eGFR, and other known risk factors. During median follow-up duration of 4.6 years, a total of 29 renal events (14.0%) occurred. The SP/hAGT group showed significantly higher risk of developing renal outcome compared to SP/lAGT group (HR, 13.4; 95% confidence interval, 1.282–139.324; P = 0.03).
Conclusion
Urinary AGT/Cr can be a useful predictive marker in the patients with relatively small ADPKD. Various biomarkers should be considered to define RP when implementing novel treatment in the patients with ADPKD.
Keyword
Figure
Reference
-
1. Davies F, Coles GA, Harper PS, Williams AJ, Evans C, Cochlin D. Polycystic kidney disease re-evaluated: a population-based study. Q J Med. 1991; 79(290):477–485. PMID: 1946928.2. Higashihara E, Nutahara K, Kojima M, Tamakoshi A, Yoshiyuki O, Sakai H, et al. Prevalence and renal prognosis of diagnosed autosomal dominant polycystic kidney disease in Japan. Nephron. 1998; 80(4):421–427. PMID: 9832641.
Article3. Neumann HP, Jilg C, Bacher J, Nabulsi Z, Malinoc A, Hummel B, et al. Epidemiology of autosomal-dominant polycystic kidney disease: an in-depth clinical study for south-western Germany. Nephrol Dial Transplant. 2013; 28(6):1472–1487. PMID: 23300259.
Article4. Chebib FT, Perrone RD, Chapman AB, Dahl NK, Harris PC, Mrug M, et al. A practical guide for treatment of rapidly progressive ADPKD with Tolvaptan. J Am Soc Nephrol. 2018; 29(10):2458–2470. PMID: 30228150.
Article5. Irazabal MV, Rangel LJ, Bergstralh EJ, Osborn SL, Harmon AJ, Sundsbak JL, et al. Imaging classification of autosomal dominant polycystic kidney disease: a simple model for selecting patients for clinical trials. J Am Soc Nephrol. 2015; 26(1):160–172. PMID: 24904092.
Article6. Kocyigit I, Yilmaz MI, Unal A, Ozturk F, Eroglu E, Yazici C, et al. A link between the intrarenal renin angiotensin system and hypertension in autosomal dominant polycystic kidney disease. Am J Nephrol. 2013; 38(3):218–225. PMID: 23988725.
Article7. Park HC, Kang AY, Jang JY, Kim H, Han M, Oh KH, et al. Increased urinary angiotensinogen/creatinine (AGT/Cr) ratio may be associated with reduced renal function in autosomal dominant polycystic kidney disease patients. BMC Nephrol. 2015; 16(1):86. PMID: 26092580.
Article8. Kim H, Park S, Jhee JH, Yun HR, Park JT, Han SH, et al. Urinary angiotensinogen level is associated with potassium homeostasis and clinical outcome in patients with polycystic kidney disease: a prospective cohort study. BMC Nephrol. 2019; 20(1):104. PMID: 30909873.
Article9. Fitzgibbon WR, Dang Y, Bunni MA, Baicu CF, Zile MR, Mullick AE, et al. Attenuation of accelerated renal cystogenesis in PKD1 mice by renin-angiotensin system blockade. Am J Physiol Renal Physiol. 2018; 314(2):F210–8. PMID: 29021226.
Article10. Kang E, Han M, Kim H, Park SK, Lee J, Hyun YY, et al. baseline general characteristics of the Korean chronic kidney disease: report from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD). J Korean Med Sci. 2017; 32(2):221–230. PMID: 28049232.
Article11. Oh KH, Park SK, Park HC, Chin HJ, Chae DW, Choi KH, et al. KNOW-CKD (KoreaN cohort study for Outcome in patients With Chronic Kidney Disease): design and methods. BMC Nephrol. 2014; 15(1):80. PMID: 24884708.
Article12. Pei Y, Obaji J, Dupuis A, Paterson AD, Magistroni R, Dicks E, et al. Unified criteria for ultrasonographic diagnosis of ADPKD. J Am Soc Nephrol. 2009; 20(1):205–212. PMID: 18945943.
Article13. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150(9):604–612. PMID: 19414839.
Article14. Vonesh E, Tighiouart H, Ying J, Heerspink HL, Lewis J, Staplin N, et al. Mixed-effects models for slope-based endpoints in clinical trials of chronic kidney disease. Stat Med. 2019; 38(22):4218–4239. PMID: 31338848.
Article15. Park HC, Ahn C. Diagnostic evaluation as a biomarker in patients with ADPKD. Adv Exp Med Biol. 2016; 933:85–103. PMID: 27730437.
Article16. Meijer E, Boertien WE, Nauta FL, Bakker SJ, van Oeveren W, Rook M, et al. Association of urinary biomarkers with disease severity in patients with autosomal dominant polycystic kidney disease: a cross-sectional analysis. Am J Kidney Dis. 2010; 56(5):883–895. PMID: 20888104.
Article17. Parikh CR, Dahl NK, Chapman AB, Bost JE, Edelstein CL, Comer DM, et al. Evaluation of urine biomarkers of kidney injury in polycystic kidney disease. Kidney Int. 2012; 81(8):784–790. PMID: 22258321.
Article18. Messchendorp AL, Meijer E, Boertien WE, Engels GE, Casteleijn NF, Spithoven EM, et al. Urinary biomarkers to identify autosomal dominant polycystic kidney disease patients with a high likelihood of disease progression. Kidney Int Rep. 2017; 3(2):291–301. PMID: 29725632.
Article19. Kocer D, Karakukcu C, Ozturk F, Eroglu E, Kocyigit I. Evaluation of fibrosis markers: apelin and transforming growth factor-β1 in autosomal dominant polycystic kidney disease patients. Ther Apher Dial. 2016; 20(5):517–522. PMID: 26991810.
Article20. Park HC, Hwang JH, Kang AY, Ro H, Kim MG, An JN, et al. Urinary N-acetyl-β-D glucosaminidase as a surrogate marker for renal function in autosomal dominant polycystic kidney disease: 1 year prospective cohort study. BMC Nephrol. 2012; 13(1):93. PMID: 22935351.
Article21. Salih M, Bovée DM, Roksnoer LC, Casteleijn NF, Bakker SJ, Gansevoort RT, et al. Urinary renin-angiotensin markers in polycystic kidney disease. Am J Physiol Renal Physiol. 2017; 313(4):F874–81. PMID: 28747358.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Renal Cell Carcinoma in Autosomal Dominant Polycystic Kidney Disease Hemodialyzed
- Autosomal Dominant Polycystic Kidney Disease: 2009 Update for Internists
- Autosomal Dominant Polycystic Kidney Desease Coexisting with Renal Dysplasia. First Case Described and Followed Since Prenatal Period
- A Case of Transitional Cell Carcinoma Associated with Adult Polycystic Kidney Disease
- A Case Report: Prenatal Ultrasonographic Diagnosis of Autosomal Dominant Polycystic Kidney Disease