Acute Crit Care.
2020 May;35(2):102-109. 10.4266/acc.2019.00780.
Inclusion of lactate level measured upon emergency room arrival in trauma outcome prediction models improves mortality prediction: a retrospective, single-center study
- Affiliations
-
- 1Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine and Graduate School of Medicine, Suwon, Korea
- 2Department of Biomedical Informatics, Ajou University School of Medicine and Department of Biomedical Sciences, Ajou University Graduate School of Medicine, Suwon, Korea
- KMID: 2502340
- DOI: http://doi.org/10.4266/acc.2019.00780
Abstract
- Background
This study aimed to develop a model for predicting trauma outcomes by adding arterial lactate levels measured upon emergency room (ER) arrival to existing trauma injury severity scoring systems.
Methods
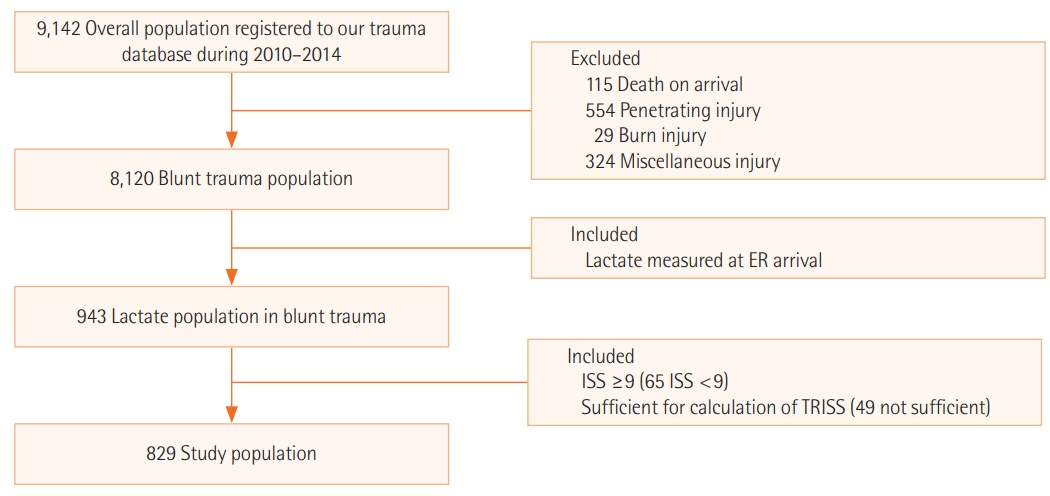
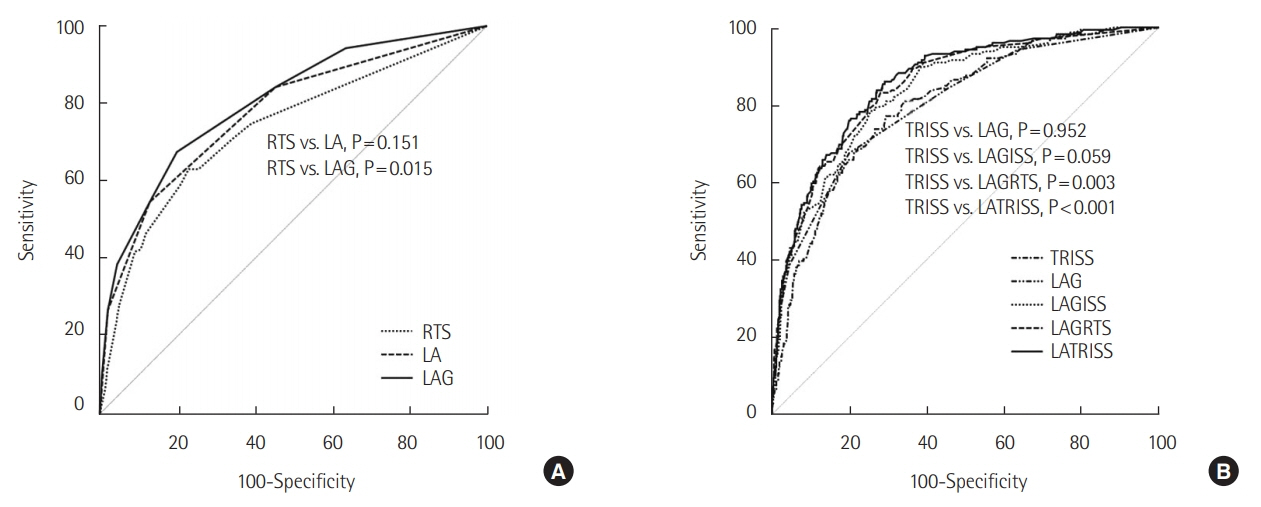
We examined blunt trauma cases that were admitted to our hospital during 2010– 2014. Eligibility criteria were cases with an Injury Severity Score of ≥9, complete Trauma and Injury Severity Score (TRISS) variable data, and lactate levels that were assessed upon ER arrival. Survivor and non-survivor groups were compared and lactate-based prediction models were generated using logistic regression. We compared the predictive performances of traditional prediction models (Revised Trauma Score [RTS] and TRISS) and lactate-based models using the area under the curve (AUC) of receiver operating characteristic curves.
Results
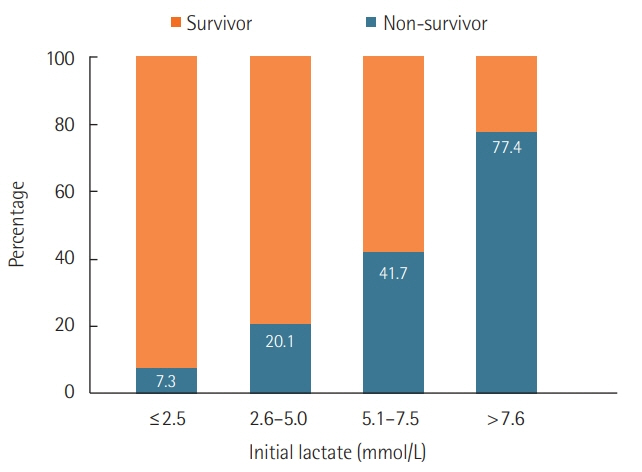
We included 829 patients, and the in-hospital mortality rate among these patients was 21.6%. The model that used lactate levels and age provided a significantly better AUC value than the RTS model. The model with lactate added to the TRISS variables provided the highest Youden J statistic, with 86.0% sensitivity and 70.8% specificity at a cutoff value of 0.15, as well as the highest predictive value, with a significantly higher AUC than the TRISS.
Conclusions
These findings indicate that lactate testing upon ER arrival may help supplement or replace traditional physiological parameters to predict mortality outcomes among Korean trauma patients. Adding lactate levels also appears to improve the predictive abilities of existing trauma outcome prediction models.
Keyword
Figure
Reference
-
1. Cook A, Weddle J, Baker S, Hosmer D, Glance L, Friedman L, et al. A comparison of the Injury Severity Score and the Trauma Mortality Prediction Model. J Trauma Acute Care Surg. 2014; 76:47–52.
Article2. Cassidy LD, Cook A, Ertl A, Gourlay D, Osler T. Is the Trauma Mortality Prediction Model (TMPM-ICD-9) a valid predictor of mortality in pediatric trauma patients? J Pediatr Surg. 2014; 49:189–92.
Article3. Vivien B, Yeguiayan JM, Le Manach Y, Bonithon-Kopp C, Mirek S, Garrigue D, et al. The motor component does not convey all the mortality prediction capacity of the Glasgow Coma Scale in trauma patients. Am J Emerg Med. 2012; 30:1032–41.
Article4. Haider AH, Villegas CV, Saleem T, Efron DT, Stevens KA, Oyetunji TA, et al. Should the IDC-9 Trauma Mortality Prediction Model become the new paradigm for benchmarking trauma outcomes? J Trauma Acute Care Surg. 2012; 72:1695–701.
Article5. Moore L, Lavoie A, Turgeon AF, Abdous B, Le Sage N, Emond M, et al. Improving trauma mortality prediction modeling for blunt trauma. J Trauma. 2010; 68:698–705.
Article6. Huber-Wagner S, Stegmaier J, Mathonia P, Paffrath T, Euler E, Mutschler W, et al. The sequential trauma score: a new instrument for the sequential mortality prediction in major trauma. Eur J Med Res. 2010; 15:185–95.7. Glance LG, Osler TM, Mukamel DB, Meredith W, Wagner J, Dick AW. TMPM-ICD9: a trauma mortality prediction model based on ICD-9-CM codes. Ann Surg. 2009; 249:1032–9.8. Osler T, Glance L, Buzas JS, Mukamel D, Wagner J, Dick A. A trauma mortality prediction model based on the anatomic injury scale. Ann Surg. 2008; 247:1041–8.
Article9. Marcin JP, Pollack MM. Triage scoring systems, severity of illness measures, and mortality prediction models in pediatric trauma. Crit Care Med. 2002; 30(11 Suppl):S457–67.
Article10. Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method: trauma score and the injury severity score. J Trauma. 1987; 27:370–8.11. Schluter PJ, Nathens A, Neal ML, Goble S, Cameron CM, Davey TM, et al. Trauma and Injury Severity Score (TRISS) coefficients 2009 revision. J Trauma. 2010; 68:761–70.
Article12. de Munter L, Polinder S, Lansink KW, Cnossen MC, Steyerberg EW, de Jongh MA. Mortality prediction models in the general trauma population: a systematic review. Injury. 2017; 48:221–9.
Article13. Schluter PJ. Trauma and Injury Severity Score (TRISS): is it time for variable re-categorisations and re-characterisations? Injury. 2011; 42:83–9.
Article14. Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW Jr, et al. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990; 30:1356–65.15. Becher RD, Meredith JW, Kilgo PD. Injury severity scoring and outcomes research. In : Mattox KL, Moore EE, Feliciano DV, editors. Trauma. 7th ed. New York: McGraw-Hill;2013. p. 77–90.16. Jung K, Huh Y, Lee JC, Kim Y, Moon J, Youn SH, et al. The applicability of trauma and injury severity score for a blunt trauma population in Korea and a proposal of new models using score predictors. Yonsei Med J. 2016; 57:728–34.
Article17. Jung K, Lee JC, Park RW, Yoon D, Jung S, Kim Y, et al. The best prediction model for trauma outcomes of the current Korean population: a comparative study of three injury severity scoring systems. Korean J Crit Care Med. 2016; 31:221–8.
Article18. Jung K, Lee JC, Kim J. Injury severity scoring system for trauma patients and trauma outcomes research in Korea. J Acute Care Surg. 2016; 6:11–7.
Article19. Park JH, Na JY, Lee BW, Chung NE, Choi YS. A statistical analysis on forensic autopsies performed in Korea in 2015. Korean J Leg Med. 2016; 40:104–18.
Article20. Statistics Korea. Korean statistical information service [Internet]. Daejeon: Statistics Korea;2018. [cited 2020 May 20]. Available from: http://kosis.kr/publication/publicationThema.do.21. Baxter J, Cranfield KR, Clark G, Harris T, Bloom B, Gray AJ. Do lactate levels in the emergency department predict outcome in adult trauma patients? A systematic review. J Trauma Acute Care Surg. 2016; 81:555–66.
Article22. Lewis CT, Naumann DN, Crombie N, Midwinter MJ. Prehospital point-of-care lactate following trauma: a systematic review. J Trauma Acute Care Surg. 2016; 81:748–55.23. Parsikia A, Bones K, Kaplan M, Strain J, Leung PS, Ortiz J, et al. The predictive value of initial serum lactate in trauma patients. Shock. 2014; 42:199–204.
Article24. Ouellet JF, Roberts DJ, Tiruta C, Kirkpatrick AW, Mercado M, Trottier V, et al. Admission base deficit and lactate levels in Canadian patients with blunt trauma: are they useful markers of mortality? J Trauma Acute Care Surg. 2012; 72:1532–5.25. Vandromme MJ, Griffin RL, Weinberg JA, Rue LW 3rd, Kerby JD. Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg. 2010; 210:861–9.
Article26. Callaway DW, Shapiro NI, Donnino MW, Baker C, Rosen CL. Serum lactate and base deficit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma. 2009; 66:1040–4.
Article27. Mizushima Y, Ueno M, Watanabe H, Ishikawa K, Matsuoka T. Discrepancy between heart rate and makers of hypoperfusion is a predictor of mortality in trauma patients. J Trauma. 2011; 71:789–92.
Article28. Neville AL, Nemtsev D, Manasrah R, Bricker SD, Putnam BA. Mortality risk stratification in elderly trauma patients based on initial arterial lactate and base deficit levels. Am Surg. 2011; 77:1337–41.
Article29. Hasler RM, Nuesch E, Jüni P, Bouamra O, Exadaktylos AK, Lecky F. Systolic blood pressure below 110 mm Hg is associated with increased mortality in blunt major trauma patients: multicentre cohort study. Resuscitation. 2011; 82:1202–7.30. Hasler RM, Nüesch E, Jüni P, Bouamra O, Exadaktylos AK, Lecky F. Systolic blood pressure below 110 mmHg is associated with increased mortality in penetrating major trauma patients: Multicentre cohort study. Resuscitation. 2012; 83:476–81.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum lactate levels in cirrhosis and non-cirrhosis patients with septic shock
- Effects of Trauma Center Establishment on the Clinical Characteristics and Outcomes of Patients with Traumatic Brain Injury : A Retrospective Analysis from a Single Trauma Center in Korea
- Association of Serum Lactate Levels Measured in the Emergency Department with 30-Day Mortality in Older Patients with Unilateral Hip Fractures
- Association of lactate clearance with outcomes of patients with gastrointestinal bleeding visiting the emergency department
- Development of a New Index for Mortality Prediction Due to Hemorrhagic Shock using Lactate Concentration and Perfusion in S-D Rats