Acute Crit Care.
2020 May;35(2):77-86. 10.4266/acc.2019.00661.
Effectiveness of a daytime rapid response system in hospitalized surgical ward patients
- Affiliations
-
- 1College of Nursing, Seoul National University, Seoul, Korea
- 2Rapid Response Team
- 3Department of Anesthesiology and Pain Medicine
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine
- 5Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul, Korea
- 6Department of Surgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2502337
- DOI: http://doi.org/10.4266/acc.2019.00661
Abstract
- Background
Clinical deteriorations during hospitalization are often preventable with a rapid response system (RRS). We aimed to investigate the effectiveness of a daytime RRS for surgical hospitalized patients.
Methods
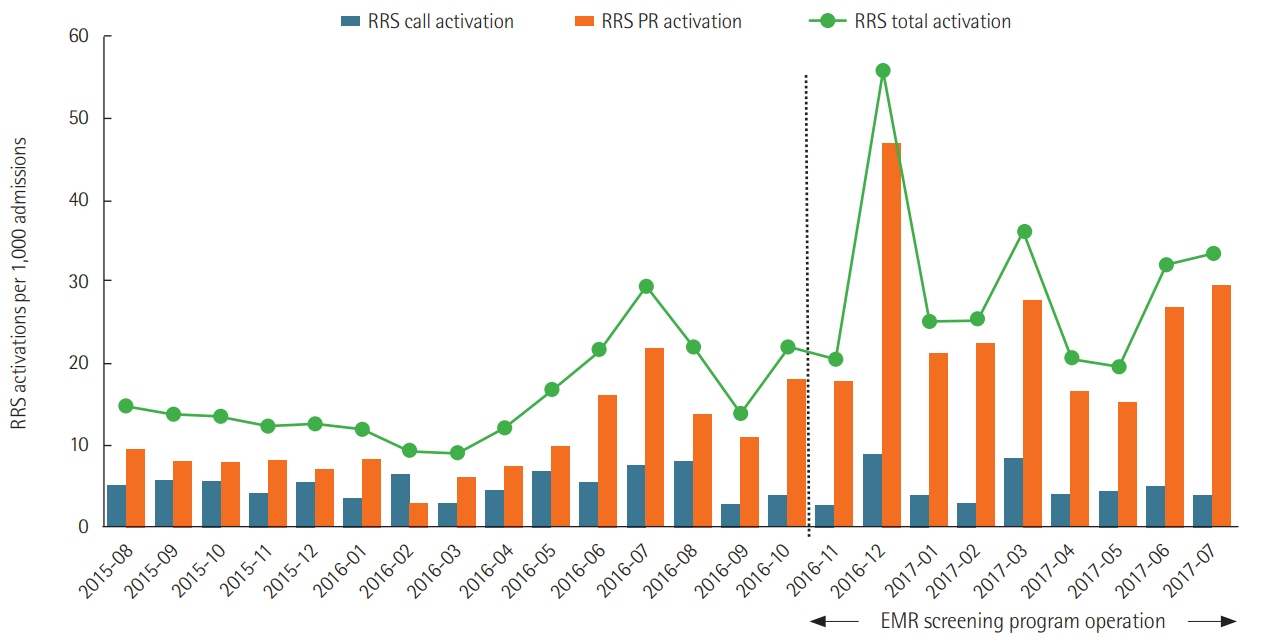
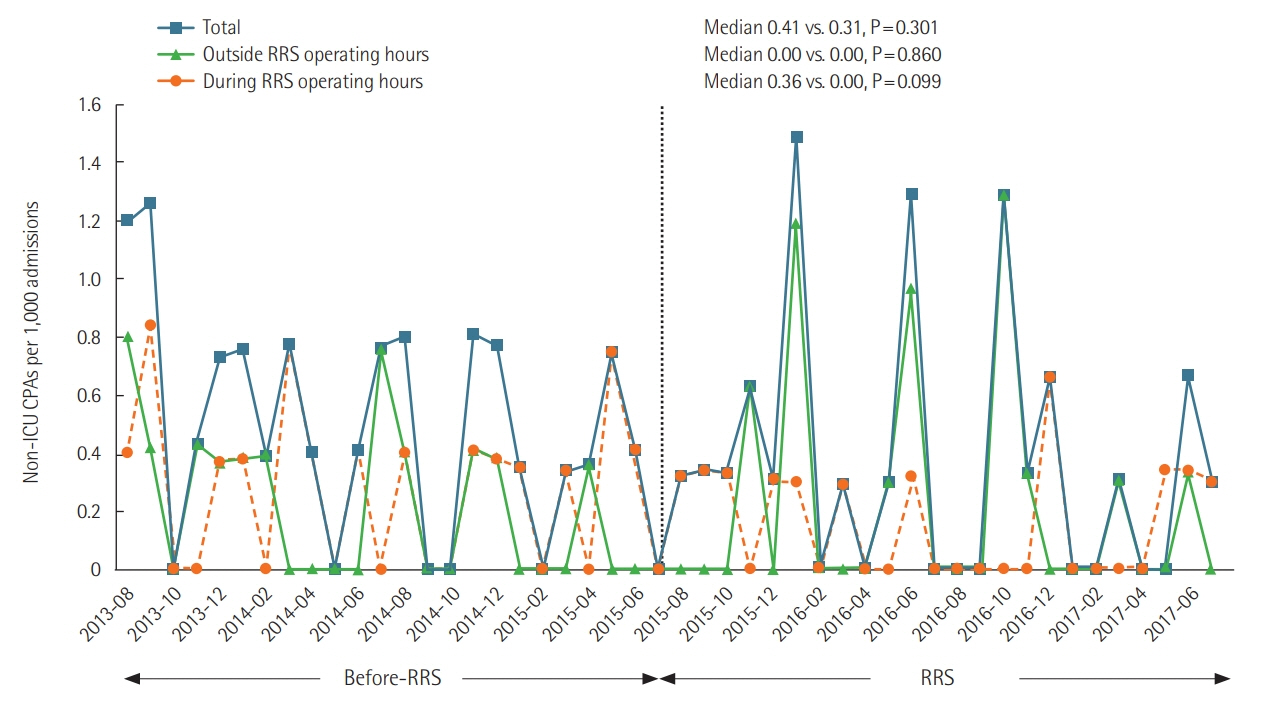
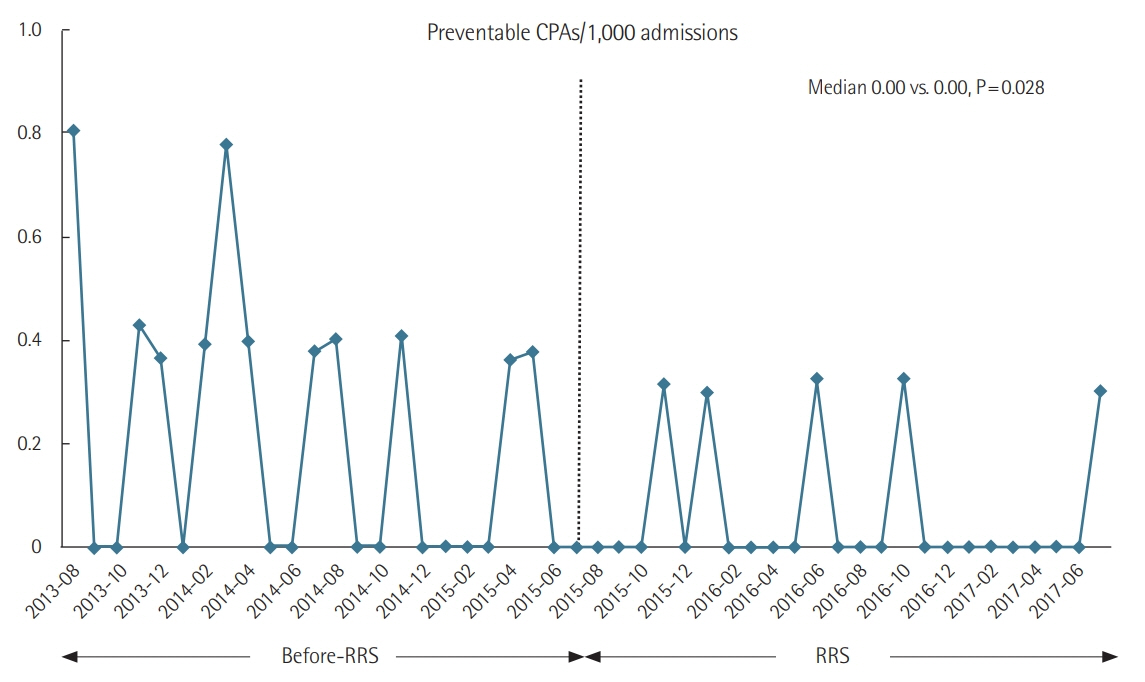
A retrospective cohort study was conducted in 20 general surgical wards at a 1,779- bed University hospital from August 2013 to July 2017 (August 2013 to July 2015, pre-RRSperiod; August 2015 to July 2017, post-RRS-period). The primary outcome was incidence of cardiopulmonary arrest (CPA) when the RRS was operating. The secondary outcomes were the incidence of total and preventable cardiopulmonary arrest, in-hospital mortality, the percentage of “do not resuscitate” orders, and the survival of discharged CPA patients.
Results
The relative risk (RR) of CPA per 1,000 admissions during RRS operational hours (weekdays from 7 AM to 7 PM) in the post-RRS-period compared to the pre-RRS-period was 0.53 (95% confidence interval [CI], 0.25 to 1.13; P=0.099) and the RR of total CPA regardless of RRS operating hours was 0.76 (95% CI, 0.46 to 1.28; P=0.301). The preventable CPA after RRS implementation was significantly lower than that before RRS implementation (RR, 0.31; 95% CI, 0.11 to 0.88; P=0.028). There were no statistical differences in in-hospital mortality and the survival rate of patients with in-hospital cardiac arrest. Do-not-resuscitate decisions significantly increased during after RRS implementation periods compared to pre-RRS periods (RR, 1.91; 95% CI, 1.40 to 2.59; P<0.001).
Conclusions
The day-time implementation of the RRS did not significantly reduce the rate of CPA whereas the system effectively reduced the rate of preventable CPA during periods when the system was operating.
Keyword
Figure
Cited by 2 articles
-
Characteristics and Prognosis of Hospitalized Patients at High Risk of Deterioration Identified by the Rapid Response System: a Multicenter Cohort Study
Sang Hyuk Kim, Ji Young Hong, Youlim Kim
J Korean Med Sci. 2021;36(32):e235. doi: 10.3346/jkms.2021.36.e235.Changes in the incidence of cardiopulmonary resuscitation before and after implementation of the Life-Sustaining Treatment Decisions Act
Hyunjae Im, Hyun Woo Choe, Seung-Young Oh, Ho Geol Ryu, Hannah Lee
Acute Crit Care. 2022;37(2):237-246. doi: 10.4266/acc.2021.01095.
Reference
-
1. Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA. 2006; 295:324–7.2. Andersen LW, Kim WY, Chase M, Berg KM, Mortensen SJ, Moskowitz A, et al. The prevalence and significance of abnormal vital signs prior to in-hospital cardiac arrest. Resuscitation. 2016; 98:112–7.
Article3. Winters BD, DeVita MA. Rapid response systems: history and terminology. In : DeVita MA, Hillman K, Bellomo R, editors. Textbook of rapid response systems. Cham: Springer;2017. p. 17–24.4. Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006; 34:2463–78.
Article5. Winters BD, Weaver SJ, Pfoh ER, Yang T, Pham JC, Dy SM. Rapid-response systems as a patient safety strategy: a systematic review. Ann Intern Med. 2013; 158(Pt 2):417–25.6. Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of inhospital cardiopulmonary arrest and mortality: a systematic review and meta-analysis. J Hosp Med. 2016; 11:438–45.
Article7. Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005; 365:2091–7.8. Winters BD, Pham J, Pronovost PJ. Rapid response teams: walk, don’t run. JAMA. 2006; 296:1645–7.9. Kim Y, Lee DS, Min H, Choi YY, Lee EY, Song I, et al. Effectiveness analysis of a part-time rapid response system during operation versus nonoperation. Crit Care Med. 2017; 45:e592–9.
Article10. Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. Part 1: executive summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132(18 Suppl 2):S315–67.11. Wood KA, Ranji SR, Ide B, Dracup K. Rapid response systems in adult academic medical centers. Jt Comm J Qual Patient Saf. 2009; 35:475–82.
Article12. Oh TK, Kim S, Lee DS, Min H, Choi YY, Lee EY, et al. A rapid response system reduces the incidence of in-hospital postoperative cardiopulmonary arrest: a retrospective study. Can J Anaesth. 2018; 65:1303–13.
Article13. Worster A, Bledsoe RD, Cleve P, Fernandes CM, Upadhye S, Eva K. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005; 45:448–51.
Article14. Han B, Chen X, Li Q. Application of case mix index in the allocation of nursing human resources. J Nurs Manag. 2018; 26:647–52.
Article15. Song KJ, Kim EH, Yoo CS, Park HO, Park KO. Development of KPCS(Korean Patient Classification System for Nurses) Based on Nursing Needs. J Korean Clin Nurs Res. 2009; 15:5–17.16. Guirgis FW, Gerdik C, Wears RL, Williams DJ, Kalynych CJ, Sabato J, et al. Proactive rounding by the rapid response team reduces inpatient cardiac arrests. Resuscitation. 2013; 84:1668–73.
Article17. Benin AL, Borgstrom CP, Jenq GY, Roumanis SA, Horwitz LI. Defining impact of a rapid response team: qualitative study with nurses, physicians and hospital administrators. BMJ Qual Saf. 2012; 21:391–8.
Article18. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015; 19:254.
Article19. Bonafide CP, Localio AR, Song L, Roberts KE, Nadkarni VM, Priestley M, et al. Cost-benefit analysis of a medical emergency team in a children’s hospital. Pediatrics. 2014; 134:235–41.
Article20. Simmes FM, Schoonhoven L, Mintjes J, Fikkers BG, van der Hoeven JG. Incidence of cardiac arrests and unexpected deaths in surgical patients before and after implementation of a rapid response system. Ann Intensive Care. 2012; 2:20.
Article21. Shearer B, Marshall S, Buist MD, Finnigan M, Kitto S, Hore T, et al. What stops hospital clinical staff from following protocols? An analysis of the incidence and factors behind the failure of bedside clinical staff to activate the rapid response system in a multi-campus Australian metropolitan healthcare service. BMJ Qual Saf. 2012; 21:569–75.
Article22. Ou L, Chen J, Hillman K, Flabouris A, Parr M, Green M. The effectiveness of a standardised rapid response system on the reduction of cardiopulmonary arrests and other adverse events among emergency surgical admissions. Resuscitation. 2020; 150:162–9.
Article23. Herod R, Frost SA, Parr M, Hillman K, Aneman A. Long term trends in medical emergency team activations and outcomes. Resuscitation. 2014; 85:1083–7.
Article24. Lee BY, Hong SB. Rapid response systems in Korea. Acute Crit Care. 2019; 34:108–16.
Article25. Hodgetts TJ, Kenward G, Vlackonikolis I, Payne S, Castle N, Crouch R, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation. 2002; 54:115–23.
Article26. Jones D, Bates S, Warrillow S, Goldsmith D, Kattula A, Way M, et al. Effect of an education programme on the utilization of a medical emergency team in a teaching hospital. Intern Med J. 2006; 36:231–6.
Article27. Salvatierra G, Bindler RC, Corbett C, Roll J, Daratha KB. Rapid response team implementation and in-hospital mortality. Crit Care Med. 2014; 42:2001–6.
Article28. Beitler JR, Link N, Bails DB, Hurdle K, Chong DH. Reduction in hospital-wide mortality after implementation of a rapid response team: a long-term cohort study. Crit Care. 2011; 15:R269.29. Santamaria J, Tobin A, Holmes J. Changing cardiac arrest and hospital mortality rates through a medical emergency team takes time and constant review. Crit Care Med. 2010; 38:445–50.
Article30. Sulmasy DP, Sood JR, Ury WA. Physicians’ confidence in discussing do not resuscitate orders with patients and surrogates. J Med Ethics. 2008; 34:96–101.
Article31. Tam B, Salib M, Fox-Robichaud A. The effect of rapid response teams on end-of-life care: a retrospective chart review. Can Respir J. 2014; 21:302–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a Rapid Response Team on the Clinical Outcomes of Cardiopulmonary Resuscitation of Patients Hospitalized in General Wards
- An Analysis of Cost and Profit of a Nursing Unit using Performance-Based Costing: Case of a General Surgical Ward in a General Hospital
- Factors Influencing the Activation Time of the Rapid Response Team
- Clinical significance of acute care surgery system as a part of hospital medical emergency team for hospitalized patients
- Computerization in Ward Nursing Information System Using Order-Communicating System