J Educ Eval Health Prof.
2019;16:32. 10.3352/jeehp.2019.16.32.
Effect of student-directed solicitation of evaluation forms on the timeliness of completion by preceptors in the United States
- Affiliations
-
- 1Pediatric Critical Care Medicine, Department of Pediatrics, Penn State Children’s Hospital, Hershey, PA, USA
- 2Department of Public Health Sciences, Pennsylvania State College of Medicine, Hershey, PA, USA
- 3General Pediatrics, Department of Pediatrics, Penn State Children’s Hospital, Hershey, PA, USA
- KMID: 2502167
- DOI: http://doi.org/10.3352/jeehp.2019.16.32
Abstract
- Purpose
Summative evaluation forms assessing a student’s clinical performance are often completed by a faculty preceptor at the end of a clinical training experience. At our institution, despite the use of an electronic system, timeliness of completion has been suboptimal, potentially limiting our ability to monitor students’ progress. The aim of the present study was to determine whether a student-directed approach to summative evaluation form collection at the end of a pediatrics clerkship would enhance timeliness of completion for third-year medical students.
Methods
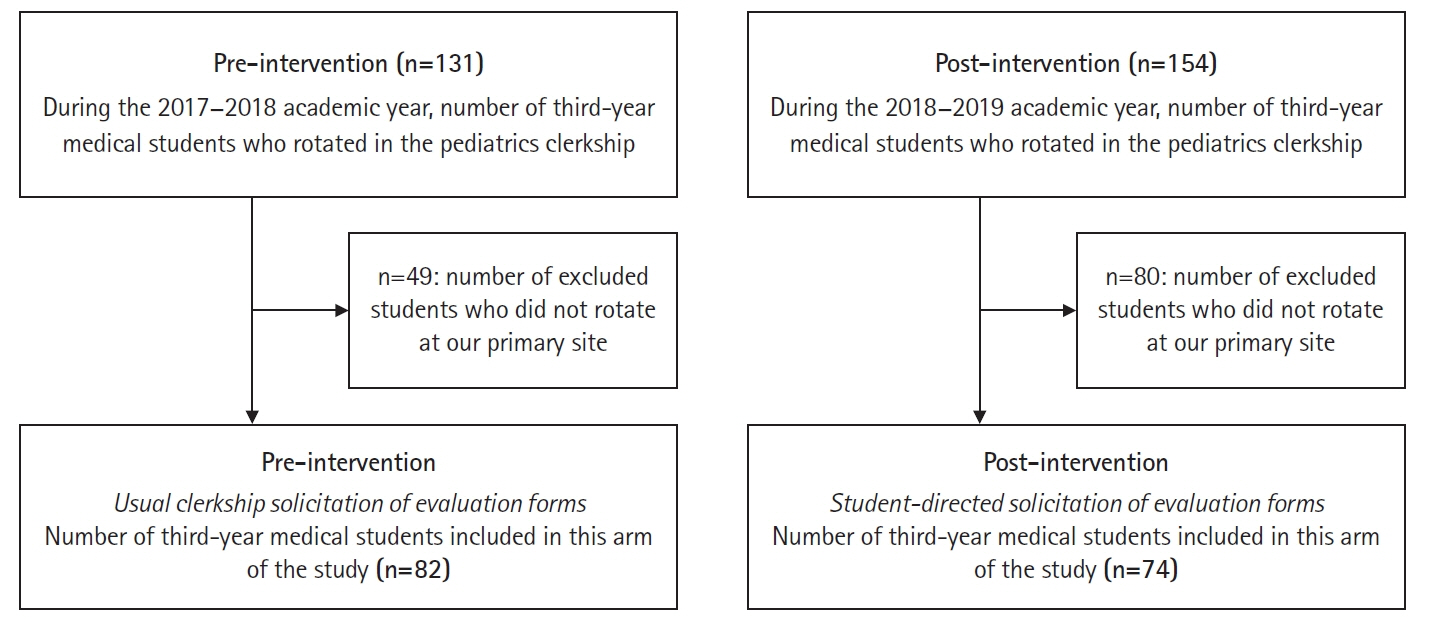
This was a pre- and post-intervention educational quality improvement project focused on 156 (82 pre-intervention, 74 post-intervention) third-year medical students at Penn State College of Medicine completing their 4-week pediatric clerkship. Utilizing REDCap (Research Electronic Data Capture) informatics support, student-directed evaluation form solicitation was encouraged. The Wilcoxon rank-sum test was applied to compare the pre-intervention (May 1, 2017 to March 2, 2018) and post-intervention (April 2, 2018 to December 21, 2018) percentages of forms completed before the rotation midpoint.
Results
In total, 740 evaluation forms were submitted during the pre-intervention phase and 517 during the post-intervention phase. The percentage of forms completed before the rotation midpoint increased after implementing student-directed solicitation (9.6% vs. 39.7%, P<0.05).
Conclusion
Our clerkship relies on subjective summative evaluations to track students’ progress, deploy improvement strategies, and determine criteria for advancement; however, our preceptors struggled with timely submission. Allowing students to direct the solicitation of evaluation forms enhanced the timeliness of completion and should be considered in clerkships facing similar challenges.
Keyword
Figure
Reference
-
References
1. Liaison Committee on Medical Education. Standards, publications, & notification forms [Internet]. Washington (DC): Liaison Committee on Medical Education;2019. [cited 2019 May 13]. Available from: http://lcme.org/publications/.2. Harrison CJ, Konings KD, Schuwirth LW, Wass V, van der Vleuten CP. Changing the culture of assessment: the dominance of the summative assessment paradigm. BMC Med Educ. 2017; 17:73. https://doi.org/10.1186/s12909-017-0912-5.
Article3. Christner JG, Dallaghan GB, Briscoe G, Casey P, Fincher RM, Manfred LM, Margo KI, Muscarella P, Richardson JE, Safdieh J, Steiner BD. The community preceptor crisis: recruiting and retaining community-based faculty to teach medical students: a shared perspective from the alliance for clinical education. Teach Learn Med. 2016; 28:329–336. https://doi.org/10.1080/10401334.2016.1152899.
Article4. Konopasek L, Norcini J, Krupat E. Focusing on the formative: building an assessment system aimed at student growth and development. Acad Med. 2016; 91:1492–1497. https://doi.org/10.1097/ACM.0000000000001171.
Article5. Holmboe ES. Work-based assessment and co-production in postgraduate medical training. GMS J Med Educ. 2017; 34:Doc58. https://doi.org/10.3205/zma001135.
Article6. Plymale MA, French J, Donnelly MB, Iocono J, Pulito AR. Variation in faculty evaluations of clerkship students attributable to surgical service. J Surg Educ. 2010; 67:179–183. https://doi.org/10.1016/j.jsurg.2010.03.003.
Article7. Rousseau M, Konings KD, Touchie C. Overcoming the barriers of teaching physical examination at the bedside: more than just curriculum design. BMC Med Educ. 2018; 18:302. https://doi.org/10.1186/s12909-018-1403-z.
Article8. Damp JB, Dewey CM, Wells Q, Horn L, Kroop SF, Mendes L. Faculty development on clinical teaching skills: an effective model for the busy clinician. J Med Educ Curric Dev. 2016; 3:JMECD.S40798. https://doi.org/10.4137/JMECD.S40798.
Article9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010.
Article10. R Core Team. R: a language and environment for statistical computing [Internet]. Vienna: R Foundation for Statistical Computing;2015. [cited 2019 May 13]. Available from: https://www.r-project.org/.11. Wormald BW, Schoeman S, Somasunderam A, Penn M. Assessment drives learning: an unavoidable truth? Anat Sci Educ. 2009; 2:199–204. https://doi.org/10.1002/ase.102.
Article12. Dudas RA, Colbert JM, Goldstein S, Barone MA. Validity of faculty and resident global assessment of medical students’ clinical knowledge during their pediatrics clerkship. Acad Pediatr. 2012; 12:138–141. https://doi.org/10.1016/j.acap.2011.09.002.
Article13. Dubosh NM, Fisher J, Lewis J, Ullman EA. Faculty evaluations correlate poorly with medical student examination performance in a fourth-year emergency medicine clerkship. J Emerg Med. 2017; 52:850–855. https://doi.org/10.1016/j.jemermed.2016.09.018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Student's Evaluation of Educational Behavior of clinical preceptors in a teaching hospital
- Discovering social learning ecosystems during clinical clerkship from United States medical students’ feedback encounters: a content analysis
- Content Analysis of the Experience of Preceptors in Clinical Education for Senior Student Nurses
- Geriatrics Education and Training Experience in the United States
- Analysis of the Clinical Education Situation framework: a tool for identifying the root cause of student failure in the United States